
It’s 2026, and your doctor prescribes you generic metformin for type 2 diabetes. It’s cheap, effective, and the standard first-line treatment. But when you walk to the pharmacy, the pharmacist says, "I can’t fill this yet. Your insurance needs prior authorization." You’re stunned. This isn’t a $10,000 specialty drug. It’s a pill that costs $4. Why does your insurance company need to sign off on it?
Why Are Generic Drugs Now Subject to Prior Authorization?
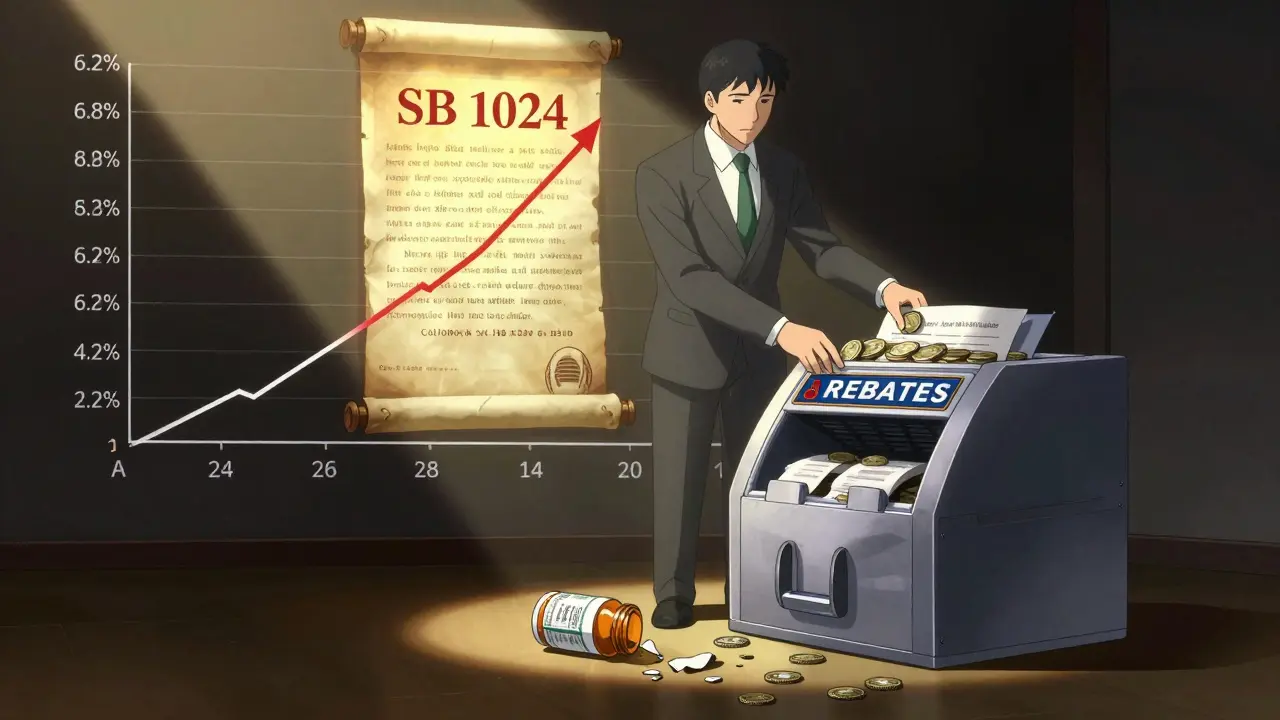
For decades, prior authorization was reserved for expensive brand-name drugs or high-risk specialty medications. Generics were the opposite - the solution to rising drug costs. But that’s changed. In 2024, 15-20% of generic prescriptions required prior authorization, up from just 5% in 2018. That’s not a glitch. It’s a policy shift. Insurance companies and pharmacy benefit managers (PBMs) are now applying the same approval rules to generics as they do to brand-name drugs. Why? It’s not about cost. Generics make up 90% of all prescriptions but only 23% of total drug spending. The real driver is control. PBMs collect over $138 billion a year in rebates and fees. By forcing providers to jump through hoops, they can steer patients toward specific generics - often the ones that give the PBM the biggest kickback. For example, your doctor might prescribe a generic lisinopril for high blood pressure. But your insurer’s formulary favors a different generic version made by a company that pays them a higher rebate. So they block the first one - even though both are chemically identical - and force your doctor to justify why the other isn’t better. It’s not medical. It’s financial.How the Process Actually Works (And Why It’s So Slow)
When a generic drug needs prior authorization, your doctor’s office must submit paperwork to your insurer. This can be done electronically, by fax, or over the phone. Most practices now use platforms like CoverMyMeds, which cut approval time by 32% compared to faxing. But even then, it’s not fast. Approval times vary wildly. Cigna says decisions take 5-10 business days. Mayo Clinic says it can be “a few days to a few weeks.” For urgent cases, you can request an expedited review - which should take 72 hours. But in practice, many patients wait longer. One Kaiser Family Foundation case study showed a patient’s HbA1c jumped from 6.8% to 8.2% over 14 days while waiting for approval of generic metformin. That’s not a delay. That’s a health risk. The paperwork is also messy. Insurers often demand:- Specific ICD-10 diagnosis codes that match the drug’s approved use
- Proof you tried (and failed) other generics first - even if those didn’t work
- Clinical notes explaining why the prescribed generic is better than the insurer’s preferred version
Who’s Getting Hit the Hardest?
Not all generics are treated the same. Some face approval requirements far more often than others.- Oncology generics - like methotrexate or capecitabine - require prior authorization in 35% of cases. Even though they’re cheaper than brand-name chemo drugs, insurers treat them like high-risk treatments.
- Cardiovascular generics - such as atorvastatin or losartan - are approved in 12% of cases. Still, that’s up from 2% five years ago.
- Thyroid meds - like levothyroxine - are now being blocked in some states. Patients report switching brands mid-treatment, causing fatigue, weight gain, and heart palpitations.
What Insurers Say vs. What Doctors and Patients Experience
Insurers argue they’re protecting patients. Dr. Mark Doolittle of AHIP claims prior authorization ensures “clinically appropriate treatment.” But here’s what doctors and patients see:- 88% of physicians say prior authorization for generics causes treatment delays (AMA, 2023)
- 24% say delays have led to hospitalizations
- On Reddit, hundreds of patients share stories of being denied generic levothyroxine, metformin, or hydrochlorothiazide - drugs they’ve taken for years without issue
- One provider wrote: “My clinic spends 17.3 hours a week on prior auths for generics. That’s a full-time job just to get patients their meds.”
What’s Changing in 2026 - And What’s Still Broken
There’s some good news. On June 23, 2025, six major insurers - Aetna, UnitedHealthcare, Cigna, Humana, Elevance, and Blue Cross Blue Shield - agreed to reforms starting January 2026. They’re:- Eliminating prior authorization for 12 common generic classes: ACE inhibitors, statins, metformin, beta-blockers, and others
- Standardizing electronic forms across all plans
- Setting a 72-hour deadline for urgent requests
What You Can Do Right Now
If your generic medication is being blocked:- Ask your doctor if they’ve submitted the prior authorization. Many offices don’t track it properly.
- Request an urgent review if your condition is unstable (e.g., uncontrolled blood pressure, high blood sugar).
- Get documentation - ask for copies of all denial letters and clinical notes. 67% of denials can be overturned with better paperwork.
- Appeal - every insurer has an appeals process. Don’t accept “no” as final.
- Check your state’s rules - California, New York, and several others now ban prior authorization for certain generics. Your drug might be protected.
Is This Trend Going to Last?
Probably not. The Congressional Budget Office projects a 40% drop in prior authorization for generics by 2028. Why? Because it’s not saving money - it’s costing more. A 2025 study by the American Gastroenterological Association found that prior authorization for first-line generics increases total healthcare costs by 18%. Why? Because delays lead to complications: uncontrolled diabetes, heart attacks, hospitalizations. The $4 pill that was denied ends up costing $12,000 in emergency care. The system was built to control costs. But now, it’s creating them. And patients are paying the price - in time, stress, and health.Why do insurance companies require prior authorization for cheap generic drugs?
Insurance companies and pharmacy benefit managers (PBMs) use prior authorization to control which version of a generic drug gets dispensed - often favoring the one that gives them the biggest rebate, not the one your doctor thinks is best. Even though generics cost far less than brand-name drugs, PBMs still profit by steering prescriptions. This isn’t about safety - it’s about profit.
How long does prior authorization for a generic drug usually take?
Approval times vary. Most insurers say 5-10 business days, but in practice, it can take up to two weeks or longer. For urgent cases, you can request an expedited review, which should be decided within 72 hours. However, delays are common, and many patients wait longer than promised.
Can I get a generic drug without prior authorization if it’s on my insurance’s formulary?
Sometimes. Many insurers have moved away from requiring prior authorization for common generics like metformin, lisinopril, and statins - especially after new 2026 reforms. But it depends on your plan and state laws. Even if a drug is on the formulary, your insurer might still require approval if they’ve placed restrictions on it. Always check with your pharmacy before filling the prescription.
What should I do if my generic medication is denied?
Don’t give up. Ask your doctor to file an appeal with additional clinical documentation - like lab results or notes explaining why other generics didn’t work. About 67% of denials are overturned on appeal. Also, check if your state has laws banning prior authorization for certain generics. California, New York, and others now protect common drugs like levothyroxine and metformin.
Are there any generic drugs that never need prior authorization?
Yes - in some states and under some plans. Starting in January 2026, major insurers will no longer require prior authorization for 12 common generic classes, including ACE inhibitors, statins, metformin, and beta-blockers. Additionally, California’s SB 1024 bans prior authorization for 47 essential generics. But outside these protections, many insurers still require approval for even basic medications.




Neil Ellis
January 21, 2026 AT 08:08Man, I remember when generics were the hero of the healthcare system - cheap, reliable, no drama. Now it’s like we’re back in the 1990s trying to get a fax machine to work during a thunderstorm. I’ve had my grandma wait two weeks for metformin while her sugar went through the roof. And the worst part? The pharmacy staff looks at you like you’re asking for a unicorn. It’s not medical care anymore. It’s a bureaucratic obstacle course designed by people who’ve never had to take a pill for anything.
But hey, at least the PBMs are making bank. I bet their bonuses are tied to how many people they delay. Maybe next they’ll make us fill out a form in triplicate just to buy aspirin.
Still… I’m holding out hope. If enough of us scream loud enough, maybe they’ll realize that $4 pills shouldn’t come with a PhD requirement.
Rob Sims
January 23, 2026 AT 01:41Oh wow. A whole article about how insurance companies are… *gasp*… acting like corporations? Shocking. Next you’ll tell me that CEOs care more about quarterly earnings than patient outcomes. What a twist.
Let me guess - the real villain here is the PBM? Not the government that let them grow into monopolistic monsters? Not the doctors who don’t push back hard enough? Not the patients who just shrug and take whatever’s handed to them?
Wake up. This isn’t a conspiracy. It’s capitalism. And if you think a $4 pill should be immune to profit motives, you’ve been living in a fairy tale written by hippies and pharmacists.
Daphne Mallari - Tolentino
January 23, 2026 AT 13:10It is, quite frankly, an egregious abdication of the fundamental principles of evidence-based medicine. The institutionalization of financial gatekeeping under the guise of clinical stewardship represents not merely inefficiency, but a profound epistemological failure. One cannot reasonably justify the imposition of administrative barriers to the dispensation of chemically identical, therapeutically validated pharmaceuticals - particularly when such barriers demonstrably exacerbate morbidity and increase aggregate system costs.
The conflation of cost-containment with access-restriction is a semantic sleight-of-hand, and the data - as cited in the original post - is unequivocal. The American Medical Association’s findings are not anecdotal; they are epidemiological. One must ask: at what point does administrative overhead become a public health crisis?
Jasmine Bryant
January 24, 2026 AT 03:20Just had this happen with my levothyroxine last month. Doctor prescribed the generic, pharmacy said ‘nope, need auth.’ Called my doc’s office - they said they submitted it three days ago. Checked my portal - still pending. Called insurer - automated system said ‘your request is being processed.’
I ended up paying $38 out of pocket for a 30-day supply just to not feel like a zombie for two weeks. My HbA1c didn’t jump, but my stress level did. And honestly? I didn’t even know I could appeal until I read this post. Thanks for the heads-up.
Also - typo in the article: ‘formulary favors a different generic version made by a company that pays them a higher rebate’ - should be ‘pays them *a* higher rebate.’ Just saying. 😅