
For millions of people taking warfarin, the idea of eating spinach, kale, or broccoli can feel like a minefield. You’ve probably heard you should avoid these foods entirely. But that advice is outdated-and dangerous. The truth? You don’t need to cut out green leafy vegetables. You just need to eat the same amount every week.
Why Vitamin K Matters with Warfarin
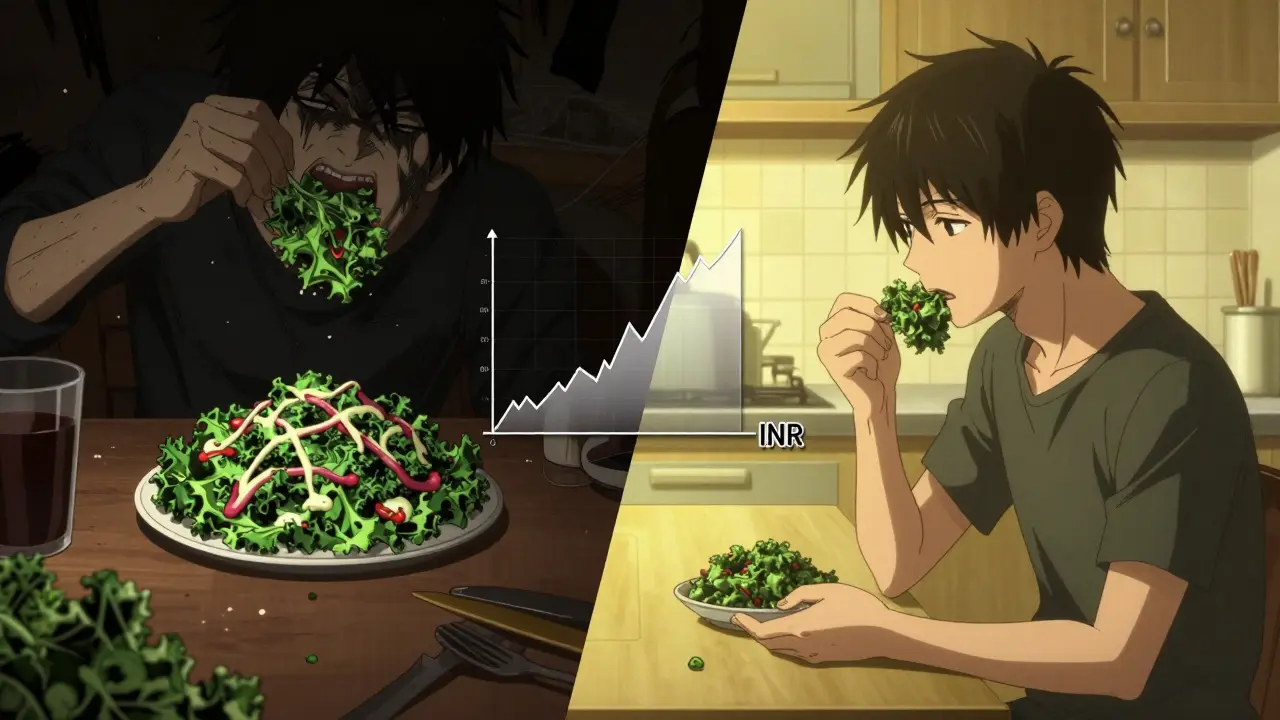
Warfarin, sold under brand names like Coumadin and Jantoven, works by blocking vitamin K in your body. Vitamin K helps your blood clot. Warfarin slows that down so clots don’t form where they shouldn’t-like in your heart, lungs, or legs. But here’s the catch: if your vitamin K intake jumps up or down, your blood’s clotting ability changes too. That’s measured by your INR (International Normalized Ratio). A stable INR between 2.0 and 3.0 means your blood is thin enough to prevent clots, but not so thin that you bleed easily.When you eat a big plate of cooked spinach one day and none the next, your INR swings. A sudden spike in vitamin K can drop your INR by 0.5 to 1.0 in just a few days. That means your blood starts clotting faster, raising your risk of stroke or pulmonary embolism. On the flip side, skipping greens for a week can spike your INR, making you bleed more easily-even from a small cut or bruise.
How Much Vitamin K Is in Common Greens?
Not all greens are created equal. The amount of vitamin K varies wildly:- Cooked spinach: 889 mcg per cup (Mayo Clinic, 2023)
- Cooked kale: 547 mcg per cup (University of Iowa Hospitals & Clinics, 2023)
- Cooked collard greens: 772 mcg per cup (GoodRx, 2023)
- Cooked broccoli: 220 mcg per cup (NHS, 2024)
- Cooked cabbage: 415 mcg per cup (NIH, 2024)
The average adult needs 90-120 mcg of vitamin K daily. That means one cup of cooked spinach gives you nearly 10 times your daily requirement. But here’s the key: you don’t need to avoid it. You just need to eat the same portion every day.
The NIH Study That Changed the Game
In March 2024, researchers from Universitas Padjadjaran published a study in the NIH’s database (PMC11844272) that settled a long-standing debate. They followed warfarin patients who ate exactly 100 grams of spinach daily-about ⅔ cup cooked. The results? No dangerous INR swings. Their blood thinning stayed stable. The study concluded that consistent spinach intake is safe and effective.This isn’t an outlier. The same pattern holds for kale, collards, and broccoli. The problem isn’t the food. It’s the inconsistency. A sudden salad bar binge on Saturday? That’s the problem. Eating the same amount every day? That’s perfectly fine.
What About Newer Blood Thinners?
Newer drugs like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) don’t interact with vitamin K. That’s why 68% of patients switched from warfarin to these drugs in a 2022 study-dietary freedom was a top reason.But here’s the reality: warfarin is still the go-to for many. If you have a mechanical heart valve-especially in the mitral position-DOACs aren’t approved. If your kidneys are severely impaired (eGFR under 15), warfarin is often safer. And cost? Warfarin runs $4-$10 a month. The newer drugs? $500-$600.
For people who can’t afford DOACs or need warfarin for medical reasons, learning to manage vitamin K isn’t a burden-it’s a lifeline.
What You Can Eat Without Worrying
You don’t have to live on white rice and chicken. Many vegetables are low in vitamin K and safe to eat freely:- Lettuce: ½ cup (80g) (NHS, 2024)
- Carrots: 3 dessert spoons
- Cauliflower: 8 florets
- Courgettes (zucchini): ½ large one
- Mushrooms: 3-4 dessert spoons
- Green beans: ½ cup
- Potatoes: any amount
These can be your daily staples. Mix them with your regular serving of spinach or kale. The goal isn’t to eliminate high-vitamin K foods-it’s to make them predictable.
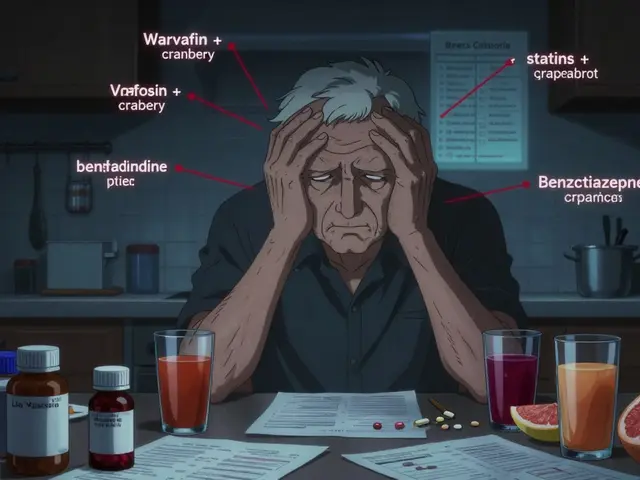
What to Avoid (Besides Inconsistency)
Some things can mess with warfarin even if your greens are steady:- Grapefruit juice - can boost warfarin levels
- St. John’s Wort - makes warfarin less effective
- Danshen and Ginkgo Biloba - increase bleeding risk
- Cod liver oil - high in vitamin A and D, can interfere
- Glucosamine - may raise INR in some people
Also, if you get sick-diarrhea, fever, vomiting-your body absorbs vitamin K differently. Contact your doctor. Your INR might need checking sooner than usual.
How to Stay Consistent
Here’s how real people do it:- Choose one high-vitamin K food you like-spinach, kale, or broccoli-and eat the same portion every day. For example: ½ cup cooked spinach daily.
- Track it in a notebook or phone app. Note the food, amount, and date.
- Don’t skip days. If you miss one, don’t double up the next day.
- When eating out, ask how food is prepared. Steamed? Fine. Sautéed in butter? Might be okay if it’s a one-off.
- Get your INR checked every 2-4 weeks when stable. More often if your diet changes.
A 2024 study from the University of Iowa found that patients using digital food trackers reduced INR variability by 27% compared to those relying on memory alone. Technology helps, but consistency is still the core.
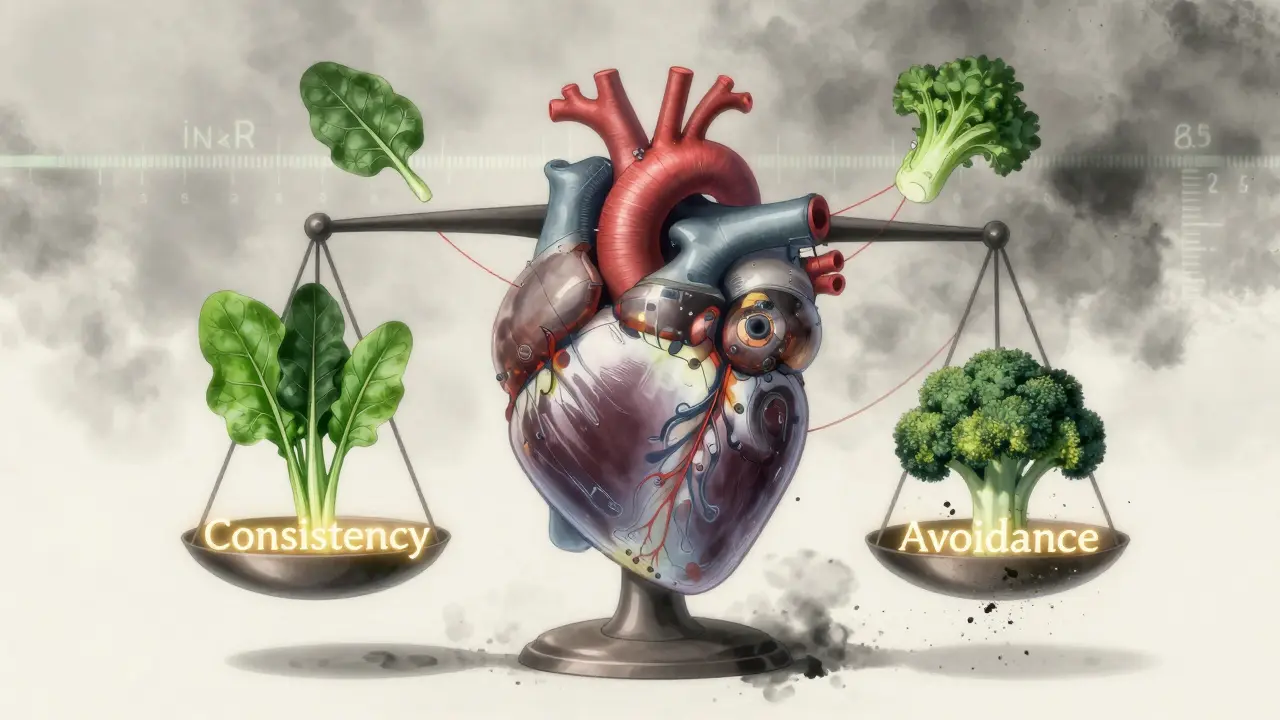
Why Avoidance Is Risky
Some alternative health sources still push complete avoidance of vitamin K. That’s not just wrong-it’s dangerous. If you cut out greens entirely, your vitamin K levels drop too low. Your body can’t make enough clotting factors. That doesn’t make your blood thinner-it makes it unstable. You’re at higher risk for both clots and bleeding.Major health organizations agree: the American College of Chest Physicians, Mayo Clinic, NHS, and University of Iowa all say the same thing: Consistency over avoidance. The evidence is clear. People who eat steady amounts of leafy greens have fewer hospital visits, fewer emergency INR adjustments, and better long-term outcomes.
What Happens When You Don’t Stick to It
In 2021, the American Heart Association found that 38% of warfarin-related ER visits were due to dietary changes. One patient ate a big kale salad after a week of no greens. His INR dropped from 2.8 to 1.6 in three days. He developed a blood clot in his leg. Another skipped greens for a week while traveling. His INR spiked to 6.2. He ended up in the hospital with internal bleeding.These aren’t rare cases. They’re predictable. And they’re preventable.
Final Takeaway
You don’t have to give up your greens. You don’t have to live in fear of broccoli. You just need to eat the same amount every day. Pick your favorite leafy vegetable. Measure it. Eat it. Repeat. That’s it.Warfarin works best when your diet is steady-not when it’s restricted. Your body doesn’t need perfect nutrition. It needs predictable nutrition. And that’s something you can control.
Can I eat spinach if I’m on warfarin?
Yes, you can eat spinach-just keep the portion size consistent. A study from the NIH found that 100 grams (about ⅔ cup cooked) of spinach daily is safe for warfarin users. The key isn’t avoiding it-it’s eating the same amount every day.
What happens if I eat a lot of kale one day?
A single large serving can drop your INR by 0.5-1.0 within 3-5 days, increasing your risk of blood clots. It doesn’t mean you’ve ruined everything, but you should notify your doctor and get an INR test sooner than scheduled.
Do I need to stop eating greens forever?
No. Avoiding greens entirely can actually raise your risk of bleeding by making your vitamin K levels too low. The goal is consistency, not elimination. Most doctors now recommend keeping your intake steady, not zero.
Are there any greens I can eat without tracking?
Yes. Lettuce, carrots, cauliflower, zucchini, mushrooms, and green beans are low in vitamin K and can be eaten freely without affecting your INR. These are great options for daily meals.
Why do some doctors still say to avoid greens?
Some older guidelines recommended avoidance, but that’s outdated. Modern research, including studies from the NIH and Mayo Clinic, shows that consistent intake is safer and more effective. If your doctor still tells you to avoid greens, ask them to review the latest guidelines from the American College of Chest Physicians.
Can I switch to a different blood thinner to avoid this issue?
Yes, newer drugs like Eliquis and Xarelto don’t interact with vitamin K. But they’re much more expensive-about $500-$600 a month versus $4-$10 for warfarin. They’re also not safe for everyone, especially those with mechanical heart valves. Talk to your doctor about whether switching makes sense for you.
How often should I check my INR?
When your diet and dose are stable, check every 2-4 weeks. If you’ve changed your food intake, started a new medication, or gotten sick, check weekly until your INR stabilizes again.



Meghan Hammack
January 10, 2026 AT 00:44I used to avoid spinach like it was poison because my doctor said ‘avoid vitamin K.’ Then I got lazy and started eating my usual ½ cup cooked spinach every day without thinking - and my INR stayed rock solid. No more panic attacks before blood tests. Seriously, consistency is the cheat code. 🙌
Lindsey Wellmann
January 11, 2026 AT 19:39OMG I CRIED WHEN I READ THIS. 😭 I thought I had to give up my weekly kale smoothie forever… I’ve been eating ¾ cup cooked kale every Monday, Wednesday, Friday for 8 months now. My INR? Perfect. My therapist? Also impressed. This isn’t dieting - it’s self-love with greens. 🥬💖
Pooja Kumari
January 13, 2026 AT 09:16Let me tell you something - I’ve been on warfarin for 12 years. I used to starve myself of greens because I was terrified. Then I had a stroke scare in 2020 because my INR spiked after I skipped my usual broccoli for a week while visiting family. I was in the ER for three days. My husband cried. My cat stopped purring when I walked in. That’s when I realized - it’s not about avoiding food. It’s about honoring your body’s rhythm. Now I eat 1 cup of collard greens every single night. No exceptions. No guilt. Just peace. And if you’re not doing that? You’re playing Russian roulette with your blood. I’m not mad. I’m just… disappointed. 🌿💔
Drew Pearlman
January 14, 2026 AT 19:42This is such an important message, and I’m so glad someone finally put it out there clearly. I work with a lot of elderly patients on warfarin, and the fear around leafy greens is rampant. So many end up malnourished because they’re avoiding entire food groups - and ironically, that makes their INR *more* unstable. The NIH study is solid, and the data from Iowa on digital trackers? Game-changer. People don’t need to be scared. They need to be empowered with routine. Consistency isn’t boring - it’s freedom. And if you’re still telling patients to avoid kale? You’re doing them a disservice. 💪🥦
Chris Kauwe
January 16, 2026 AT 11:56Let’s be real - this is just another example of how the medical-industrial complex is trying to normalize chaos under the guise of ‘personalization.’ The fact that you have to track your spinach intake like a lab rat proves the system is broken. Warfarin is a 1950s drug with a 1950s diet protocol. The real solution isn’t ‘eat the same amount’ - it’s ditching warfarin entirely. DOACs exist for a reason. If you can’t afford them? That’s a policy failure, not a personal one. Stop glorifying archaic regimens. This isn’t discipline - it’s institutional neglect dressed up as advice.
RAJAT KD
January 16, 2026 AT 21:41Consistency > avoidance. Period.
Ian Long
January 17, 2026 AT 21:18Chris makes a good point about DOACs - and I get it. But for people with mechanical valves or kidney failure? Warfarin is still the only option. And for someone on Medicare with a $5 monthly copay? Switching isn’t a choice - it’s a fantasy. The real win here isn’t the drug. It’s the mindset shift. You’re not a prisoner of your diet. You’re the architect of your stability. That’s powerful. I’ve seen patients go from panic to pride just by eating their ½ cup of spinach like it’s a daily ritual. It’s not about restriction. It’s about ownership.
Angela Stanton
January 18, 2026 AT 06:18Let’s analyze this statistically: 38% of ER visits linked to dietary inconsistency? That’s a 2.7x higher risk than non-compliance with medication timing. And yet, only 12% of patients use food tracking apps. The cognitive load here is underreported. The ‘eat the same amount’ advice sounds simple - until you’re at a wedding with 7 different salads, a side of sautéed kale, and no idea what’s in the dressing. This isn’t just about spinach. It’s about systemic lack of support. No one gives you a grocery list. No one teaches you how to estimate portions in restaurants. You’re just told ‘be consistent’ and left to drown. The real failure isn’t the patient. It’s the healthcare system that treats nutrition like a math problem instead of a human experience. 📊📉