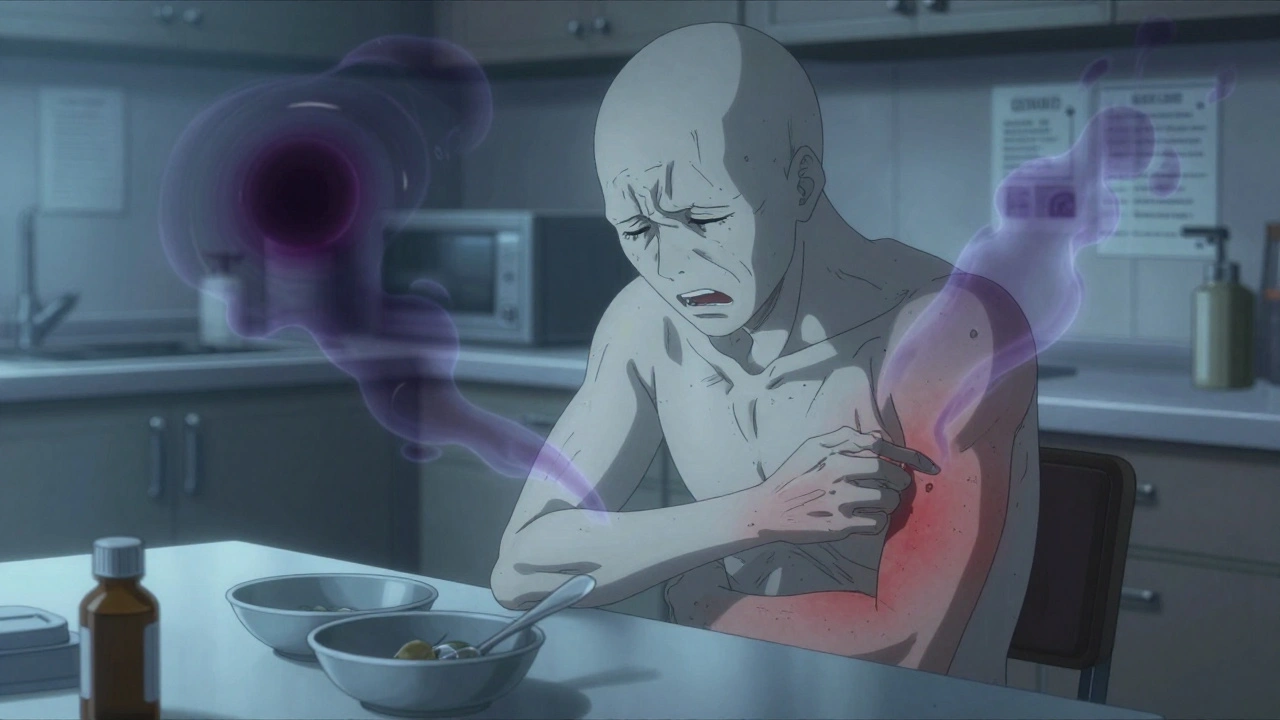
When your kidneys stop working, your body doesn’t just slow down-it starts to poison itself. Uremic symptoms like constant nausea and unbearable itching aren’t just uncomfortable; they’re warning signs your body is drowning in waste it can’t flush out. For many people with advanced kidney disease, these symptoms are the reason they finally go to the doctor. But here’s the truth: waiting until you feel terrible to start dialysis can cost you more than just comfort-it can cost you time, health, and even life.
What Exactly Are Uremic Symptoms?
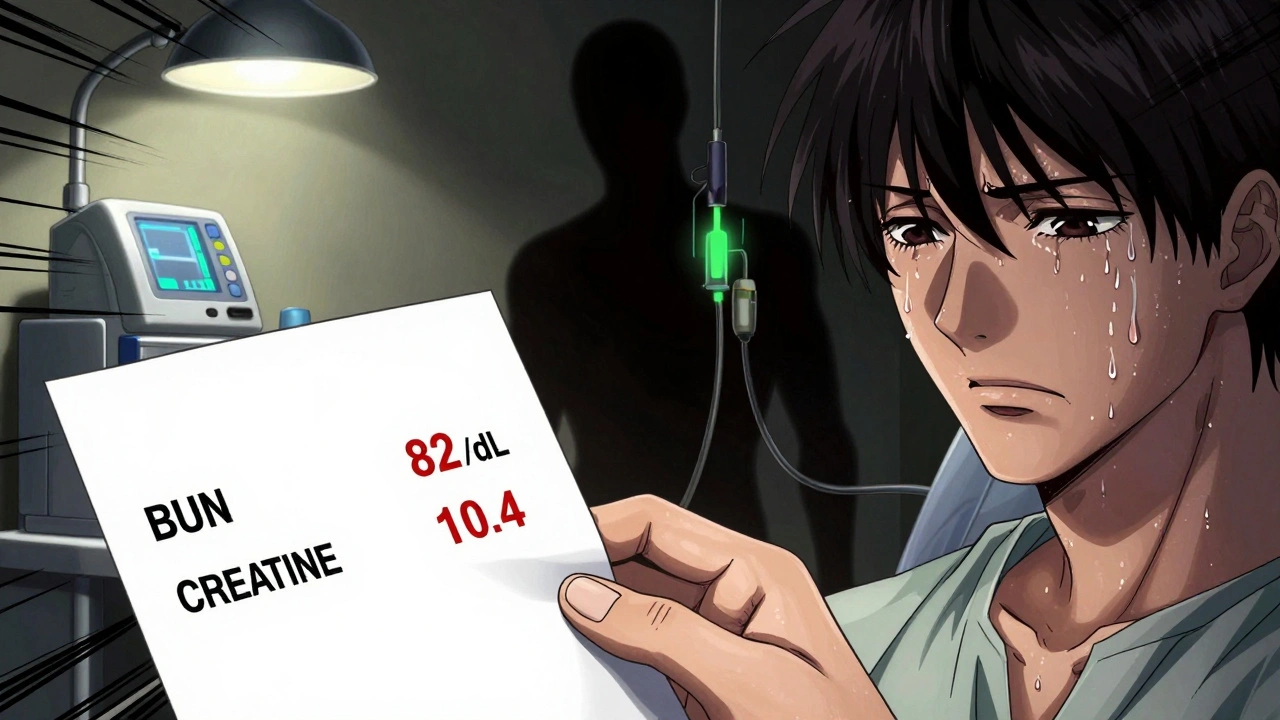
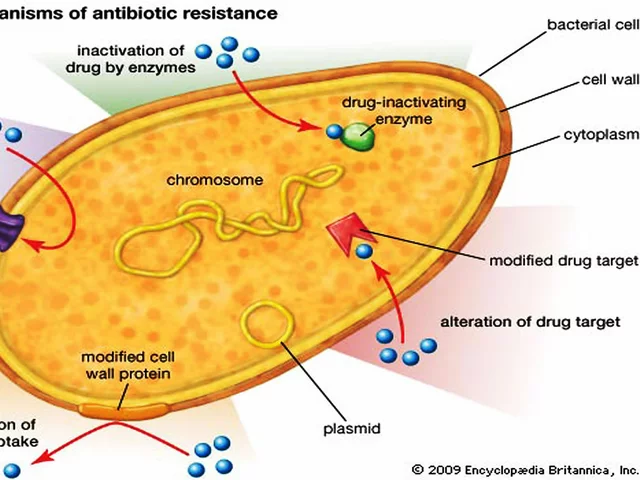
Uremia isn’t a single disease. It’s the collection of symptoms caused by your kidneys failing to remove toxins from your blood. When creatinine climbs above 10 mg/dL and BUN hits 60 mg/dL or higher, your body starts to react. These aren’t random side effects-they’re direct results of chemicals like urea, indoxyl sulfate, and p-cresyl sulfate building up in your bloodstream. They don’t just sit there. They trigger nerves, inflame tissues, and mess with your brain’s signals. Nausea is one of the most common. About 68% of people with stage 5 chronic kidney disease (CKD) report feeling sick to their stomach regularly. It’s not just morning sickness. It’s persistent, often worse after eating, and doesn’t go away with antacids. For some, it turns food into something they can’t stand. One patient on a kidney forum described eating as “swallowing sand.” That’s not exaggeration-it’s the metallic taste from uremic toxins making even water taste wrong. Then there’s the itching. Not the kind you get from dry skin or an allergic reaction. This is uremic pruritus-deep, relentless, and often worse at night. Studies show it affects up to 70% of people on dialysis and nearly 40% of those still not on dialysis. You scratch until your skin bleeds. You lose sleep. You stop going out. You change jobs because you can’t focus. The itching isn’t just in your skin-it’s tied to inflammation. People with severe itching have CRP levels nearly three times higher than those without it. That’s a clear sign your immune system is on high alert.Why Nausea and Itch Don’t Go Away on Their Own
You might think, “I’ll just take an anti-nausea pill” or “I’ll use lotion for the itch.” But these symptoms aren’t caused by something simple. They’re caused by toxins your kidneys used to handle. No amount of OTC medicine will flush out indoxyl sulfate or p-cresyl sulfate. These molecules cling to proteins in your blood and keep circulating. They don’t get cleared by vomiting or scratching. Nausea comes from these toxins hitting the chemoreceptor trigger zone in your brainstem. That’s the part that controls vomiting. When urea levels climb past 80 mg/dL, this area goes haywire. No wonder anti-nausea meds like ondansetron help-but only temporarily. Once the toxin load increases again, the nausea returns. The itching is even more complex. It’s not just one cause. It’s inflammation. It’s nerve damage. It’s mineral imbalances. High phosphate and calcium-phosphorus product levels above 55 mg²/dL² are strongly linked to itching. Parathyroid hormone levels over 600 pg/mL make it worse. Even your dialysis treatment-if it’s not adequate (Kt/V under 1.4)-won’t remove enough toxins to help. That’s why topical creams rarely work. That’s why antihistamines don’t touch it. You can’t treat the symptom without treating the root: failing kidneys.When Should You Start Dialysis?
The old rule was: wait until you’re near death. Back in the 1970s, people only started dialysis when they were vomiting constantly, confused, or had fluid flooding their lungs. But that’s not the standard anymore. Current guidelines from the National Kidney Foundation say dialysis should begin when symptoms become unmanageable-not just when your eGFR hits a number. That’s huge. You don’t have to wait until your kidney function drops to 5% if you’re already suffering. Here’s what doctors look for now:- Persistent nausea that causes weight loss (5% or more in 3 months)
- Severe itching scoring above 15 on the 5-D Itch Scale (duration, degree, direction, disability, distribution)
- Fluid overload that won’t respond to diuretics
- Pericarditis (inflammation around the heart) confirmed by ultrasound
- Neurological symptoms like confusion, tremors, or seizures
What Happens If You Wait Too Long?
Delaying dialysis doesn’t make you tougher. It makes you sicker. A 2022 study found that patients who waited until they were hospitalized with severe uremic symptoms had 18% higher hospitalization rates than those who started earlier. Why? Because toxins don’t just cause discomfort-they damage organs. High levels of uremic waste can lead to:- Heart damage from high potassium and fluid overload
- Bone fractures from calcium-phosphate imbalance
- Brain fog and depression from toxin buildup
- Malnutrition from nausea and loss of appetite
How Doctors Treat the Symptoms Before Dialysis
You don’t have to suffer until dialysis starts. There are ways to manage symptoms while you wait. For nausea:- Ondansetron (4mg, 3 times a day) is first-line. It blocks the brain’s vomiting center.
- Domperidone can help if ondansetron doesn’t work, but it’s risky if you have heart issues-it can prolong your QTc interval by nearly 30 milliseconds.
- Small, frequent meals. Avoid heavy, greasy foods. Cold foods often taste better when your sense of taste is off.
- Optimize dialysis-if you’re already on it, make sure your Kt/V is above 1.4.
- Gabapentin (starting at 100mg at night, up to 300mg three times daily) helps calm overactive nerves.
- Difelikefalin (Korsuva) is FDA-approved for this. It’s given IV during dialysis and reduces itching by over 30% in weeks.
- Nalfurafine (not yet FDA-approved in the U.S.) is a powerful option overseas-patients report sleeping through the night after years of insomnia.
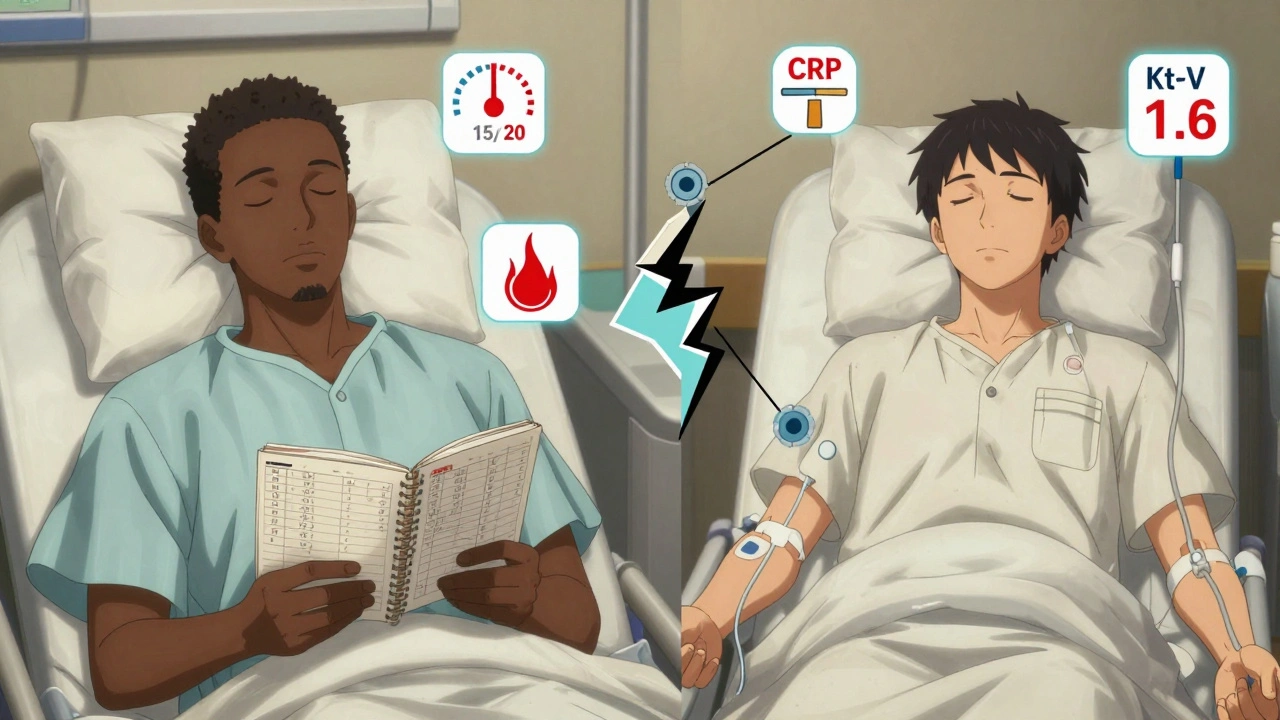
What’s Changing in Kidney Care?
The future of dialysis decisions is shifting. Instead of just looking at eGFR, doctors are starting to use patient-reported outcomes. The 2024 KDIGO guidelines are expected to include tools like the PROMIS-Itch scale. If your itch score hits above 15, you might qualify for dialysis-even if your eGFR is still at 10. That’s a game-changer. It puts your experience first. New drugs are coming too. Nemifitide, a new kappa-opioid agonist, showed 45% better itch reduction than placebo in trials. That’s huge for people who can’t tolerate gabapentin or don’t respond to Korsuva. But access is still unequal. Only 67% of U.S. dialysis centers use formal itch assessment tools. In Europe, it’s 92%. That gap means many Americans are still being told to “just live with it.” They shouldn’t be.What You Should Do Right Now
If you have advanced kidney disease and you’re dealing with nausea or itching:- Track your symptoms. Use a notebook or app. Note when nausea hits, how bad the itching is, whether you’re sleeping, and if you’ve lost weight.
- Ask for a 5-D Itch Scale assessment. Don’t assume your doctor knows how bad it is-show them your notes.
- Request blood tests for BUN, creatinine, phosphate, calcium, and CRP. Don’t wait for them to order them.
- If you’re already on dialysis, ask: “Is my Kt/V above 1.4?” If not, push for more time or a better machine.
- Don’t accept “it’s just part of the disease.” There are treatments. There are options. You deserve relief.
Can uremic itching be cured without dialysis?
No, uremic itching can’t be cured without dialysis because it’s caused by toxins your kidneys can’t remove. Medications like gabapentin or difelikefalin can reduce the itch, but they only manage the symptom. Once dialysis starts, toxin levels drop-and itching often improves dramatically. Without dialysis, the itching will return and worsen as kidney function declines.
How do I know if my nausea is from kidney disease and not something else?
If you have advanced kidney disease (eGFR under 30) and your nausea doesn’t improve with antacids, diet changes, or anti-nausea meds, it’s likely uremic. Key signs: it’s constant, worse after eating, and paired with a metallic taste, loss of appetite, or weight loss. Blood tests showing high BUN (over 80 mg/dL) and creatinine (over 8 mg/dL) confirm it. If you’re not on dialysis and have these symptoms, talk to your nephrologist immediately.
Is it safe to delay dialysis if I feel okay?
No, feeling okay doesn’t mean you’re safe. Many people with severe uremia feel fine until they suddenly collapse. Toxins build up silently, damaging your heart, bones, and nerves. The IDEAL trial showed that people who waited until they had symptoms had worse quality of life-even if their survival rates were similar. If you have nausea, itching, fatigue, or swelling, don’t wait for a crisis. Start the conversation with your doctor now.
Why do some people get severe itching while others don’t?
It varies because of genetics, inflammation levels, and mineral imbalances. People with higher CRP, phosphate, and parathyroid hormone levels are far more likely to have severe itching. Also, some people’s nerves are more sensitive to toxins. Studies show that even with the same kidney function, one person might have mild itch while another is scratching until they bleed. That’s why personalized treatment matters.
What’s the best treatment for uremic itching right now?
The most effective treatment approved in the U.S. is difelikefalin (Korsuva), given during dialysis. It reduces itching by over 30% within days. For those not on dialysis, gabapentin is often used first. Nalfurafine works even better but isn’t available in the U.S. Yet. Topical creams and antihistamines rarely help. The key is treating the root cause: toxin buildup. Dialysis remains the most reliable solution.
Can diet help with uremic symptoms?
Yes, but it’s not a cure. Limiting phosphorus (no colas, processed cheese, nuts), reducing sodium (to control fluid), and eating small, cold meals can reduce nausea and itching. Avoiding protein-heavy meals may help lower toxin production. But diet alone can’t replace dialysis when kidney function is very low. It’s a tool to make symptoms more manageable-not a replacement for treatment.



Elizabeth Farrell
December 2, 2025 AT 15:42It’s wild how much we ignore our bodies until they scream. I had a friend with CKD who kept saying, ‘It’s just stress,’ for months-until she collapsed at work. The itching? She scratched her arms raw. The nausea? She lost 20 pounds. No one told her dialysis wasn’t a last resort-it was a lifeline. I wish someone had handed her this post earlier.
Sheryl Lynn
December 3, 2025 AT 16:06Ah, the exquisite poetry of uremic toxins-indoxyl sulfate, p-cresyl sulfate-these aren’t merely metabolic byproducts, they’re the silent poets of systemic decay, whispering through the blood-brain barrier in iambic pentameter of despair. One must admire the elegance of nature’s revenge: the body, once a temple, now a derelict cathedral echoing with the cacophony of failed filtration. Truly, the sublime horror of nephrology.
Fern Marder
December 5, 2025 AT 02:44OMG this is SO REAL. 😭 I’ve seen this with my mom. She was ‘just tired’ for 6 months. Then one day she couldn’t stand up. Dialysis saved her life. But the itching?? She used to wear long sleeves in July. Don’t wait. Just go. 💔
william tao
December 6, 2025 AT 19:37It is regrettable that medical decision-making has devolved into a subjective exercise predicated upon anecdotal symptomatology rather than objective, quantifiable biomarkers. The IDEAL trial, as cited, clearly demonstrates no mortality benefit from early initiation; thus, to prioritize patient-reported discomfort over evidence-based thresholds constitutes a dangerous precedent.
Sandi Allen
December 8, 2025 AT 16:02THEY DON’T WANT YOU TO KNOW THIS-dialysis isn’t about saving lives… it’s about keeping the system running. Big Pharma loves Korsuva-$10,000 a dose! And the doctors? They’re paid by the machine. They don’t care if you’re itching-they care if you show up for your 3x/week slot. They’ll tell you ‘it’s normal’… until you’re on a ventilator. Wake up.
John Webber
December 9, 2025 AT 20:44my bro had kidney issues and he kept saying he was fine till he almost died. doctors said he waited too long. now he’s on dialysis and he says it was the best thing ever. i used to think it was scary but now i get it. just talk to your doc. don’t be dumb.
Shubham Pandey
December 10, 2025 AT 00:21Same in India. People wait till they can’t walk. Then rush to hospital. Dialysis is expensive. No one talks about it. Just suffer in silence.
Paul Santos
December 11, 2025 AT 05:23One must interrogate the epistemological foundations of symptom-driven dialysis initiation. Is suffering, after all, a valid metric for clinical intervention-or merely a culturally mediated construct? The 5-D Itch Scale, while charmingly quantified, remains a phenomenological proxy for a deeper ontological rupture: the disintegration of the embodied self. One wonders if the true cure lies not in filtration, but in reimagining the body as a site of resilience, not failure.
Eddy Kimani
December 11, 2025 AT 23:13This is such a crucial breakdown. I’m a med student and I had no idea how much symptom burden drives dialysis decisions now. The shift from eGFR-only to PROMIS-Itch and patient-reported outcomes is huge. I’m going to bring this up in my nephrology rotation tomorrow. Also, Korsuva’s 30% reduction is massive-why isn’t this first-line everywhere?
Chelsea Moore
December 13, 2025 AT 20:32HOW DARE THEY TELL PEOPLE TO JUST ‘LIVE WITH IT’?!?!? My cousin was told that for 11 months. She had to beg for blood tests. Then they said, ‘Oh, you’re in crisis now-better start dialysis.’ NO. NO. NO. This is medical neglect. Someone needs to sue these hospitals. This is not healthcare. This is torture with a clipboard.
John Biesecker
December 14, 2025 AT 20:20man i had no idea how deep this goes. i thought itching was just dry skin. but the part about CRP levels being 3x higher? that’s wild. i mean… our bodies are so smart but also so broken. i feel bad for everyone who’s been told it’s ‘just part of it.’ you deserve to sleep. you deserve to eat. you’re not weak for needing help.
Genesis Rubi
December 16, 2025 AT 10:27USA is falling apart. In my country we get free dialysis. Here you need insurance, a good job, and a miracle. My neighbor’s husband died waiting for approval. They call it ‘healthcare’ but it’s a lottery. If you’re poor, you die slow. And they wonder why people are angry.
Doug Hawk
December 17, 2025 AT 23:07Reading this made me think about my uncle. He was diagnosed with CKD but refused dialysis because he didn’t want to be a burden. He didn’t complain. He just got quieter. I didn’t realize until after he passed that his itching was so bad he’d wear gloves to bed. This post should be required reading for every patient with advanced kidney disease. You’re not weak for needing help. You’re brave for asking.
Elizabeth Farrell
December 19, 2025 AT 19:07Thank you for sharing your uncle’s story. That’s exactly why I’m sharing this-people think silence means strength. But sometimes silence is just fear. And fear keeps people from asking for help. If one person reads this and goes to their doctor because of it, then this post mattered.