
When your skin starts showing dark patches-especially on your face-it’s easy to assume it’s just a tan that won’t fade. But if those patches don’t go away after summer, or if they come back even when you’re careful in the sun, you’re probably dealing with hyperpigmentation. Not all dark spots are the same. Two of the most common types, melasma and sun damage, look similar but behave very differently. And treating them the same way can make things worse.
What’s Really Going On With Your Skin?
Hyperpigmentation means your skin is making too much melanin, the pigment that gives skin its color. This overproduction doesn’t happen randomly. It’s triggered by specific factors, and those factors determine what kind of dark spots you get.Sun damage, also called solar lentigines, shows up as small, flat, brown spots. They appear on areas you’ve spent the most time in the sun-your cheeks, nose, hands, shoulders. These spots are the result of years of UV exposure. Every time your skin gets burned or tanned, melanocytes (the pigment-making cells) get a little more activated. Over time, they cluster and form visible spots. By age 60, about 90% of fair-skinned people have them.
Melasma is different. It doesn’t just show up on sun-exposed skin-it shows up symmetrically. Think dark patches on both cheeks, the bridge of your nose, your forehead, or above your upper lip. It’s not just from the sun. Hormones play a huge role. Pregnancy, birth control pills, hormone replacement therapy-they can all trigger melasma. It’s why it affects women far more than men, especially those with medium to darker skin tones (Fitzpatrick skin types III to VI). In fact, Black, Asian, and Hispanic women are 3 to 5 times more likely to develop it than Caucasian women.
And here’s the kicker: melasma isn’t just triggered by UV light. Visible light-like the kind that comes through windows or from your phone screen-and even heat can activate melanocytes. That’s why someone can have melasma flare up even when they’re wearing sunscreen. Standard sunscreens that only block UV rays aren’t enough.
Why Sunscreen Isn’t Enough (And What Actually Works)
Most people think SPF 30+ is the golden rule. And it is-for preventing skin cancer and slowing sun damage. But for melasma? It’s not enough.Harvard Medical School’s Dr. Kourosh says it plainly: “The sun is stronger than any medicine I can give you.” That’s not hyperbole. If you’re treating melasma but still letting visible light hit your skin, you’re fighting a losing battle. Studies show visible light contributes to 25-30% of melasma cases.
So what sunscreen should you use? Mineral-based ones with zinc oxide or titanium dioxide are good. But you need something extra: iron oxides. These pigments block visible light. Look for sunscreens labeled as “tinted” or “with iron oxide.” They’re not just for hiding redness-they’re medical-grade protection.
And don’t forget reapplication. Most people use less than half the amount they should. You need about a quarter-teaspoon just for your face. And if you’re outside, reapply every two hours-even on cloudy days. Indoors? If you sit near a window, you’re still getting exposed. Visible light passes through glass.
Topical Treatments: What Actually Works
There’s no magic cream that erases pigmentation overnight. But the right combination, used consistently, can make a real difference.Hydroquinone is still the gold standard. At 4% concentration, it blocks the enzyme tyrosinase, which your skin uses to make melanin. It’s effective-especially when combined with other ingredients. But it’s not for long-term use. Using it for more than three months carries a 2-5% risk of ochronosis, a condition where the skin turns a strange brownish-gray. That’s why dermatologists prescribe it in cycles: 12 weeks on, then off for a few months.
Tretinoin (a retinoid) doesn’t lighten pigment directly. Instead, it speeds up skin cell turnover. Think of it like a gentle exfoliator that pushes out old, pigmented cells faster. It’s usually used at 0.025% to 0.1%. The catch? It can irritate your skin. Start slow-every other night-and build up over weeks. Don’t rush it.
Vitamin C (L-ascorbic acid at 10-20%) is an antioxidant that neutralizes free radicals from UV and visible light. It also helps fade existing pigment by reducing oxidized melanin. Use it in the morning, under your sunscreen. It’s gentle, stable, and works well with other treatments.
The most effective approach? Triple therapy. That’s hydroquinone + tretinoin + a corticosteroid (like hydrocortisone). This combo reduces inflammation, boosts penetration, and speeds up results. Studies show it improves melasma by 50-70% in 12 weeks. That’s why 75% of dermatologists now prescribe it as a first-line treatment-up from just 45% in 2018.
For those who can’t use hydroquinone, alternatives like tranexamic acid (5% topical) and cysteamine cream (10%) are showing promise. Tranexamic acid, originally used to reduce heavy bleeding, also blocks pigment-stimulating signals in the skin. In trials, it reduced melasma by 45% in 12 weeks-with almost no side effects. Cysteamine improved melasma by 60% in 16 weeks, and it’s less irritating than hydroquinone.

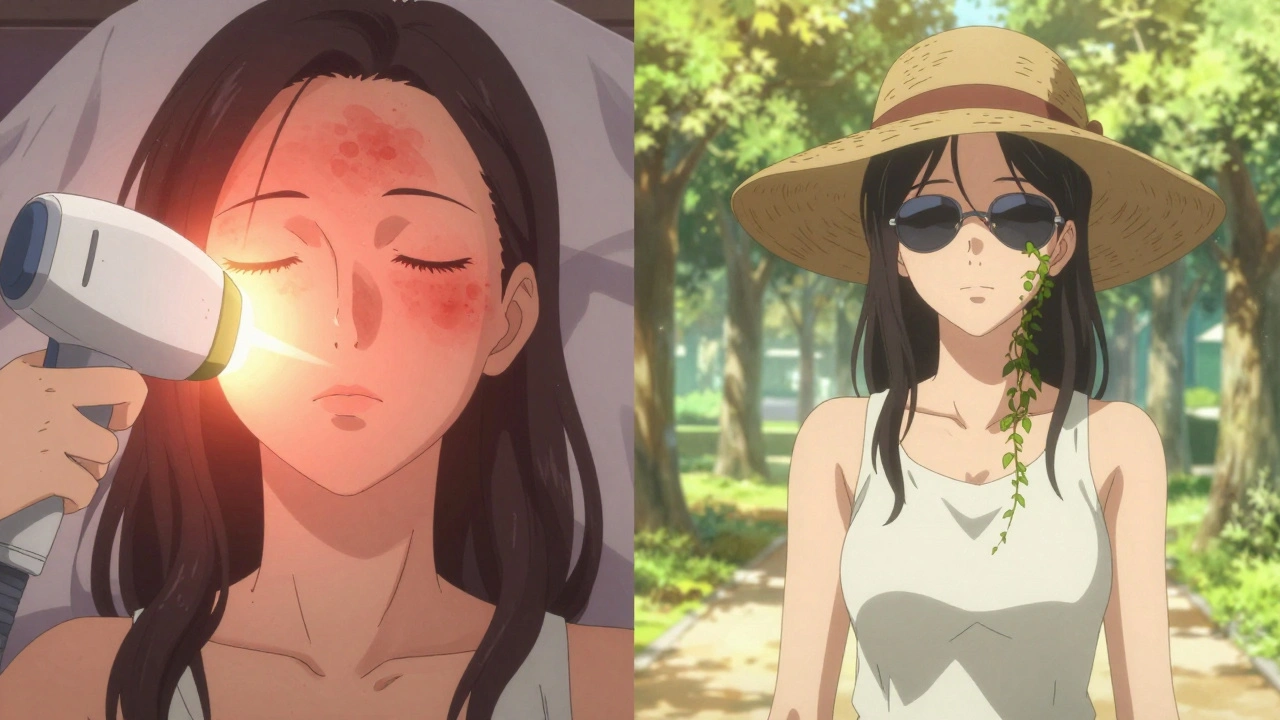
Laser and Light Therapies: Use With Caution
If you’ve been to a spa or clinic, you’ve probably heard about IPL (Intense Pulsed Light) or laser treatments. They sound like quick fixes. But for melasma? They’re risky.IPL works well for sun damage. It targets the pigment, heats it up, and the body naturally sheds it. Within days, the spots darken and flake off. Success rate? 75-90% in 2-3 sessions.
But for melasma? That same heat can trigger more pigment production. Studies show 30-40% of melasma patients get worse after IPL. That’s why dermatologists won’t even consider it until the skin has been “rested” with 8-12 weeks of topical treatment. Only then, when melanocytes are calmed down, do they consider light therapy.
And forget about chemical peels unless you’re under a dermatologist’s care. They can help-but if done too aggressively on darker skin, they can cause post-inflammatory hyperpigmentation (PIH), which is even harder to treat.
How Long Until You See Results?
Sun damage? You might see improvement in 4-8 weeks with topical treatments. Laser treatments often work in one or two sessions.Melasma? Patience is everything. Most people don’t see noticeable change until week 8-12. And even then, improvement is usually 40-60%-not total clearance. That’s because melasma is a chronic condition. It doesn’t go away. It goes into remission.
Here’s the hard truth: 95% of people who stop treatment get melasma back within six months. That’s not failure. That’s biology. The triggers-hormones, sun, heat-are still there. So maintenance is non-negotiable. You don’t treat melasma. You manage it.
The Biggest Mistake People Make
It’s not using the wrong product. It’s not skipping sunscreen. It’s inconsistency.Studies show only 35% of patients stick with their topical regimen for the full recommended time. Why? Irritation. Confusion. Too many steps. You’re applying vitamin C in the morning, hydroquinone at night, sunscreen every two hours, and you’re tired.
Here’s a simple routine that works:
- Morning: Vitamin C serum → tinted mineral sunscreen with iron oxide (SPF 50+)
- Evening: Alternate nights-hydroquinone one night, tretinoin the next. Skip both nights if skin is irritated.
That’s it. No complicated 10-step routines. No need to buy 10 different serums. Just two key products, used right, with strict sun protection.
And if your skin stings or flakes? Slow down. Start with tretinoin every third night. Wait two weeks. Then increase. Don’t push through irritation. That’s how you trigger PIH.
What About Over-the-Counter Products?
Eighty-five percent of people with melasma try OTC creams first. Niacinamide, kojic acid, licorice extract-they sound gentle, and they are. But they’re weak. Most contain less than 2% active ingredients. They might brighten skin slightly, but they won’t touch melasma.And don’t be fooled by “natural” or “organic” labels. Many contain unregulated ingredients that can irritate or even worsen pigmentation.
If you’re going the OTC route, look for products with at least 10% vitamin C, 5% niacinamide, or 2% tranexamic acid. But if you’ve tried for 3 months with no change? See a dermatologist. Prescription treatments are worth it.
Cost, Access, and the Future
Prescription topicals cost $50-$150 a month. Laser sessions? $300-$600 each. That’s a barrier for many.Hydroquinone is still the most prescribed agent worldwide, but it’s banned in the EU and Japan over safety concerns. The FDA is now considering reclassifying it as an over-the-counter product-with strict labeling and monitoring. That could make it more accessible, but also riskier if people misuse it.
Looking ahead, dermatologists are moving toward personalized treatment. Genetic testing might soon tell you whether your melasma is hormone-driven, UV-driven, or heat-sensitive. That means treatments could be tailored to your biology, not just your skin tone.
For now, the best advice is simple: protect your skin every day, use proven topicals consistently, and don’t rush to lasers. Melasma isn’t a flaw to be erased. It’s a signal your body is giving you. Listen to it. Treat it with patience. And never underestimate the power of sunscreen.
Is melasma the same as sun spots?
No. Melasma appears as large, symmetrical patches on the face and is triggered by hormones, heat, and visible light-not just sun. Sun spots (solar lentigines) are smaller, irregular, and caused by cumulative UV exposure. They respond better to lasers, while melasma can worsen with them.
Can I treat melasma with over-the-counter products?
Some OTC products with vitamin C, niacinamide, or tranexamic acid may help mildly, but they won’t match prescription strength. Most melasma cases need hydroquinone, tretinoin, or a combination therapy to see real results. If OTC products haven’t worked after 3 months, see a dermatologist.
Why does my sunscreen not stop my melasma from getting worse?
Standard sunscreens only block UV rays. Melasma is also triggered by visible light and heat, which pass through regular sunscreen. You need a tinted mineral sunscreen with iron oxide to block visible light. Even indoors, sitting near a window can trigger flare-ups.
How long does it take to see results from topical treatments?
For melasma, it usually takes 8-12 weeks to see any improvement. Sun spots can improve in 4-8 weeks. Don’t stop treatment early. Consistency over months matters more than speed. Stopping too soon leads to recurrence.
Are lasers safe for melasma?
Lasers like IPL carry a 30-40% risk of making melasma worse because heat activates pigment cells. They’re only considered after 8-12 weeks of topical treatment have calmed the skin. Even then, results are mixed. For most people, topical care and sun protection are safer and more effective long-term.
Will melasma go away on its own?
Sometimes, like after pregnancy, melasma fades slightly. But in most cases, it doesn’t disappear completely without treatment. Even if it seems better, stopping sun protection or skincare leads to recurrence in 95% of people within six months. It’s a chronic condition that needs ongoing management.
If you’ve been struggling with dark patches and feel like nothing works, you’re not alone. The key isn’t finding the perfect product-it’s understanding what’s causing it and sticking with a simple, smart plan. Your skin doesn’t need more products. It needs consistency, protection, and patience.




Rich Paul
December 10, 2025 AT 09:53Delaine Kiara
December 10, 2025 AT 15:54Ruth Witte
December 11, 2025 AT 13:13Katherine Rodgers
December 13, 2025 AT 03:16Lauren Dare
December 14, 2025 AT 19:28Gilbert Lacasandile
December 16, 2025 AT 12:12Lola Bchoudi
December 17, 2025 AT 21:17Morgan Tait
December 19, 2025 AT 14:30Darcie Streeter-Oxland
December 20, 2025 AT 21:15Christian Landry
December 21, 2025 AT 05:44Maria Elisha
December 21, 2025 AT 10:39Angela R. Cartes
December 22, 2025 AT 18:05Lisa Whitesel
December 24, 2025 AT 08:20Larry Lieberman
December 26, 2025 AT 04:46Courtney Black
December 27, 2025 AT 21:58