
Every year, Americans fill over 3.9 billion prescriptions for generic drugs. That’s 9 out of every 10 prescriptions written. But here’s the part most people don’t realize: those 3.9 billion prescriptions cost just $98 billion. Meanwhile, the 435 million brand-name prescriptions-less than 10% of the total-cost $700 billion. That’s not a typo. You’re paying nearly seven times more for the same medicine, just because of the label.
Generic drugs aren’t cheaper because they’re weaker. They’re cheaper because the system lets them be. The FDA requires them to have the same active ingredients, strength, dosage form, and performance as the brand-name version. That means your generic lisinopril for high blood pressure works the same as the brand-name Zestril. Your generic metformin for diabetes? Exactly the same as Glucophage. The only differences? The color, shape, or filler ingredients-none of which affect how the drug works in your body.
How Much Money Are You Actually Saving?
In 2024, the average out-of-pocket cost for a generic prescription was $6.95. For a brand-name drug? $28.69. That’s a difference of over $21 per fill. If you take three prescriptions a month, that’s $63 saved every 30 days. Over a year? That’s $756 in your pocket. Multiply that across millions of patients, and you start to see why generics are the single biggest cost-saving tool in U.S. healthcare.
Since 2015, the amount spent on all generic drugs in the U.S. has actually gone down-by $6.4 billion-even as more generics hit the market and prescriptions rose. How? Because prices keep falling. When a new generic enters the market, competition kicks in. Sometimes, dozens of companies start making the same drug. That drives prices down fast. For example, when the generic version of the cholesterol drug Lipitor came out, the price dropped from $120 per month to under $10. That’s not inflation. That’s market power.
The Real Impact: $445 Billion Saved in One Year
In 2023 alone, generic and biosimilar drugs saved the U.S. healthcare system $445 billion. That’s more than the entire annual budget of the Department of Education. Think about that for a second. If you removed generics from the system tomorrow, drug spending would jump from $798 billion to over $1.2 trillion. That’s a $400+ billion increase in one year.
Biosimilars-the generic versions of complex biologic drugs-are adding even more savings. Since their introduction, they’ve saved $56.2 billion. In 2024 alone, they saved $20.2 billion. One of the biggest wins? The biosimilars for Stelara, a drug used for psoriasis and Crohn’s disease. Before biosimilars, Stelara cost over $10,000 per year. Now, with nine biosimilar options on the market, the price has dropped by as much as 90%. That’s not just savings. That’s access.

Why Do Brand Drugs Cost So Much?
Brand-name companies don’t charge more because they’re better. They charge more because they can. When a drug is first approved, the manufacturer gets a 20-year patent. That’s supposed to give them time to recoup research costs. But many companies use legal tricks to extend that monopoly long after the patent expires.
One common tactic is called “patent thickets.” Instead of one patent, companies file dozens-sometimes over 75-on minor changes like coating, pill shape, or delivery method. One drug had its patent protection stretched from 2016 all the way to 2034. That’s nearly 20 extra years of monopoly pricing. Another trick? “Product hopping.” A company slightly reformulates a drug, pushes patients to the new version, then stops making the old one. Suddenly, generics can’t be substituted, even though the medicine is the same.
These practices aren’t just unfair-they’re expensive. Blue Cross Blue Shield estimates that “pay-for-delay” deals-where brand companies pay generic makers to stay off the market-cost consumers $3 billion a year and the system $12 billion.
Who’s Using Generics-and Who’s Not?
Eighty-seven percent of commercial health plans now require patients to try generics first. Medicare and Medicaid are the same. But not everyone has access. Uninsured patients still pay full list price for brand drugs-sometimes over $130 per prescription. That’s up 50% since 2019. Meanwhile, generic prices for the same drugs have gone down by 6% over the same period.
Some patients worry generics don’t work as well. There’s a myth that generics are “weaker.” But the FDA tracks adverse events. Since 2019, less than 1% of reports about generic drug problems involve effectiveness. Most complaints come from people switching between different generic manufacturers-especially for drugs with a narrow therapeutic index, like warfarin or levothyroxine. Even then, the differences are tiny and usually fixable with a dose adjustment.

What’s Next? The 2025 Patent Cliff
Three blockbuster drugs are losing patent protection in late 2025: Entresto (heart failure), Tradjenta (diabetes), and Opsumit (pulmonary hypertension). Together, they brought in $8.6 billion in sales last year. Once generics arrive, prices will likely drop by 80-90%. That could mean savings of $7 billion in just 12 months.
The FDA approved 745 generic drugs in 2024-a 12% jump from 2023. That’s the fastest pace in over a decade. More are coming. But there’s a catch. The Inflation Reduction Act now lets the government set price caps on brand drugs before generics even hit the market. That’s a problem. Why? Because price caps remove the incentive for generic manufacturers to enter the market. If the brand drug is already capped at $50, why spend millions to get FDA approval for a generic that will sell for $45?
What You Can Do
If you’re paying for prescriptions out of pocket, always ask your pharmacist: “Is there a generic version?” Even if your doctor doesn’t mention it, pharmacists are trained to spot substitutions. In 42 states, pharmacists can legally switch a brand drug for a generic without calling the doctor-unless the doctor specifically says “dispense as written.” If you live in one of the other eight states, you might need to ask your doctor to change the prescription.
Use tools like GoodRx or SingleCare. They show you the lowest cash price for generics at nearby pharmacies. Sometimes, the cash price is lower than your insurance copay.
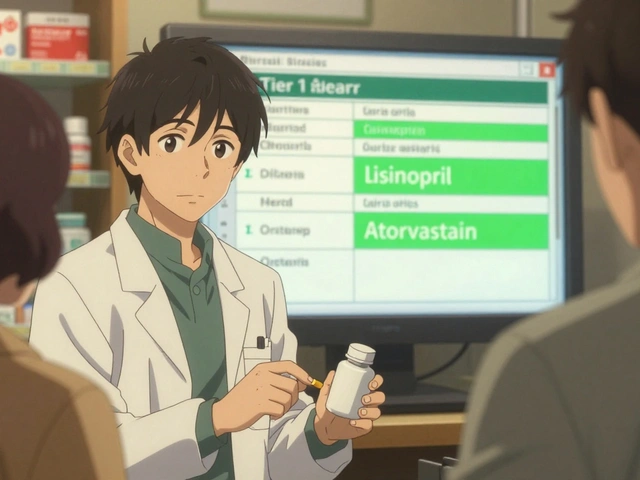
And if you’re on Medicare, check your plan’s formulary. Some plans have tiers. Generics are almost always Tier 1-the cheapest. Brand drugs? Tier 3 or 4. You’re paying more because your plan lets you.
The bottom line? Generics aren’t a compromise. They’re the smart choice. They’re just as safe. Just as effective. And they save you hundreds-or thousands-of dollars a year. The system works. It just needs you to use it.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and bioavailability as the brand-name version. That means they work the same way in your body. The FDA tests them rigorously before approval. Over 90% of prescriptions in the U.S. are for generics, and adverse event reports show less than 1% involve effectiveness issues.
Why do generic drugs cost so much less?
Generic manufacturers don’t have to repeat expensive clinical trials. Thanks to the Hatch-Waxman Act of 1984, they only need to prove their drug is bioequivalent to the brand. That cuts development costs by up to 80%. Plus, once multiple companies start making the same drug, competition drives prices down-sometimes to pennies per pill.
Can I trust generics if they look different from the brand?
Absolutely. The appearance-color, shape, or size-has no effect on how the drug works. Those differences are just to avoid trademark infringement. The active ingredient is identical. If you’re concerned, ask your pharmacist to confirm the generic is FDA-approved and has the same active ingredient as your brand.
Do insurance plans favor generics?
Yes. Most insurance plans put generics on the lowest cost tier-Tier 1. That means your copay is usually $5-$10. Brand-name drugs are often Tier 3 or 4, costing $40-$100. Many plans require you to try the generic first before covering the brand. This isn’t just policy-it’s savings for everyone.
What if my doctor says only the brand works for me?
If your doctor writes “dispense as written” or “no substitution” on the prescription, the pharmacist can’t switch it. But ask why. For most medications, generics work just as well. For a small number of drugs with a narrow therapeutic index-like warfarin or seizure meds-switching between generics might need monitoring. But even then, switching between brands and generics is usually safe with proper oversight.
Are there any drugs that don’t have generics?
Yes, but they’re rare. Newer drugs still under patent, complex biologics (like some cancer or autoimmune drugs), and some older drugs with low demand may not have generics yet. But the FDA approves hundreds of new generics every year. If your drug doesn’t have a generic today, it likely will in the next 1-3 years.
How do I find the cheapest generic?
Use apps like GoodRx, SingleCare, or Blink Health. They compare prices across local pharmacies and often offer coupons that beat your insurance copay. Some pharmacies like Walmart and Costco offer $4 generic lists for common medications. Always ask your pharmacist for the cash price-it’s often lower than the insured price.




stephanie Hill
November 23, 2025 AT 21:51Okay but have you ever seen the inside of a generic pill factory? I swear they use the same machines that make cheap glitter and birthday candles. I took a generic version of my anxiety med and woke up feeling like my soul had been swapped for a TikTok algorithm. Not saying it doesn’t work… just saying my dreams were weirder. 🤨
Akash Chopda
November 24, 2025 AT 15:35Big pharma owns the FDA and the FDA owns your doctor
Nikki C
November 25, 2025 AT 19:56Generics are the quiet heroes of American healthcare. Nobody throws them parades but they’re the reason my grandma can afford her blood pressure meds. I grew up watching my mom choose generics because she had to. Not because she was cheap. Because she was smart. And now I do the same. The system is rigged but this one little choice? It’s ours to make. And we should make it every time.
Alex Dubrovin
November 26, 2025 AT 21:03Just asked my pharmacist for a generic and saved $42 this month. I’m putting that money toward tacos. Not a metaphor. Actual tacos. Three of them. With extra cilantro. The system works if you just ask
Victoria Stanley
November 27, 2025 AT 12:04If you're worried about switching to generics especially for things like thyroid or seizure meds talk to your pharmacist first. They can check the bioequivalence data and even help you stick with the same generic manufacturer if you notice small changes. Most people never have an issue but if you do it's not the drug it's the filler. And that's fixable.
Andy Louis-Charles
November 28, 2025 AT 14:50Just got my first biosimilar for my autoimmune thing. Cost $80 instead of $1200. 😍 I didn’t even know these existed until last month. The FDA didn’t hide it. I just didn’t ask. Don’t be afraid to ask your doc or pharmacist. They’re not trying to hide anything. Just busy.
Douglas cardoza
November 29, 2025 AT 15:19My insurance won’t cover the brand even if I want it. So I take the generic. And guess what I’m alive. And my blood pressure is fine. And I didn’t turn into a zombie. The system isn’t perfect but this part? It’s working. Stop overthinking it.
Adam Hainsfurther
November 29, 2025 AT 23:41What’s wild is that the same people who scream about government overreach are the ones who don’t realize that without generics they’d be paying $500 a month for a pill that’s chemically identical to one that costs $6. The market isn’t broken. The rules are. And the rules were written by people who profit when you don’t know the difference between a pill and a price tag.