
When you can’t speak for yourself, who decides which medicines you get, stop, or adjust? A Medical Power of Attorney lets you pick a trusted person to answer that exact question, keeping your values front‑and‑center during a health crisis.
What is a Medical Power of Attorney?
Medical Power of Attorney is a legal document that designates a health‑care agent to make medical choices on your behalf when you lack capacity. It only activates when you cannot communicate your wishes, so it works side‑by‑side with other advance‑care tools like a living will.
The agent’s authority can cover hospital admission, surgery consent, and, most importantly, medication decisions-whether a drug is started, paused, or stopped.
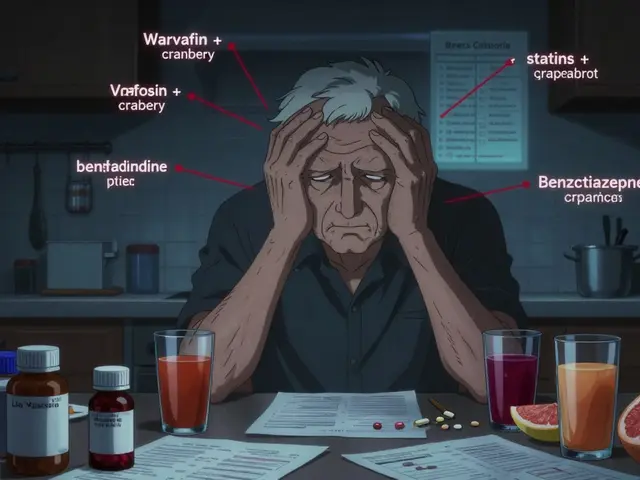
Why Focus on Medication Decisions?
Medication choices are often the flashpoint in intensive‑care units. A 2023 study in the Journal of Pain and Symptom Management showed that patients with a designated health‑care proxy experienced 32% fewer medication‑related conflicts. Without clear guidance, families can argue over antibiotics, pain meds, or blood thinners, leading to delays that cost lives.
Doctors trust written instructions. The American Medical Association’s Code of Medical Ethics (Opinion E‑2.225) explicitly recommends that clinicians encourage patients to name a proxy and discuss medication preferences beforehand.

Step‑by‑Step: Creating a Medical Power of Attorney
- Choose the right agent. Pick someone who knows your health values, can handle stressful conversations, and lives nearby or can be reached quickly.
- Gather existing documents. Pull any living will, POLST, or psychiatric advance directive you already have.
- Download a state‑specific form. Most states offer free PDFs through LawHelp DC or local health‑law clinics.
- Fill out the form while you’re still mentally competent. Include:
- Agent’s full name and contact info.
- Specific medication scenarios you anticipate (e.g., "If I develop sepsis, give IV antibiotics unless I have a documented allergy.")
- Limits on the agent’s power, if any (e.g., "Agent may not authorize blood transfusions").
- Sign in front of required witnesses or a notary. Requirements differ: California needs only your signature; New York demands two adult witnesses.
- Distribute copies. Give one to your agent, one to your primary physician, and file a copy in your medical record.
- Many hospitals now store the document electronically, thanks to the 21st Century Cures Act.
- Review annually. Life changes-new diagnoses, medication changes, or a shift in relationship dynamics-should trigger an update.
Medical Power of Attorney vs. Living Will vs. POLST
| Feature | Medical Power of Attorney | Living Will | POLST (Physician Orders for Life‑Sustaining Treatment) |
|---|---|---|---|
| Primary purpose | Appoints a trusted agent to make real‑time decisions | Provides written wishes for specific scenarios | Translates wishes into medical orders for clinicians |
| Scope for medication decisions | Agent can start, modify, or stop any medication per your goals | Typically generic (e.g., "no extraordinary measures") | Specifies orders like "IV antibiotics: yes" or "no" |
| When it takes effect | Only when you lack decision‑making capacity | Only when you are incapacitated and the document is referenced | Immediately, as a standing medical order |
| Legal standing across states | Recognized in all 50 states, but authority limits vary | Universal, but may be overridden by state law | Adopted in 47 states, often tied to emergency services |
| Typical creation time | 20-45 minutes (plus discussion) | 15-30 minutes | Completed with a physician during a serious‑illness visit |

Common Pitfalls and How to Avoid Them
1. Vague medication instructions. Saying "no pain meds" without specifying dosage thresholds leads to confusion. Write concrete numbers (e.g., "No opioids over 10 mg morphine‑equivalent per day").
2. Choosing an agent without clear communication. Agents who haven’t heard your values may interpret wishes incorrectly. Schedule a sit‑down, or use a video tool like PREPARE to record your preferences.
3. Ignoring state‑specific limits. Some states restrict agents from ordering psychiatric meds. Check with a local attorney or the American Bar Association’s multi‑state form for those nuances.
4. Not updating after major health events. A new diagnosis of diabetes changes medication priorities. Review your directive within 30 days of any major change.
5. Forgetting to share the document. An agent without a copy can’t act. Store it in a secure digital vault, and give the hospital’s intake desk a printed copy at admission.
Resources, Tools, and Next Steps
Several free resources can jump‑start the process:
- National Institute on Aging offers a simple checklist for medication preferences.
- State health‑department websites (e.g., LawHelp DC) provide downloadable forms.
- Digital platforms like Everplans (one‑time fee) guide you through each step and store the document securely.
- For tech‑savvy users, the PREPARE app lets you record video explanations that your agent can replay later.
After you’ve completed the form, take these three actions:
- Confirm that your primary care doctor has a copy in the electronic health record.
- Discuss at least two realistic medication scenarios with your agent (e.g., antibiotics for infection, pain control for a fracture).
- Schedule a yearly “advance‑care check‑in” with a trusted family member or legal advisor.
Planning ahead removes guesswork, reduces family stress, and gives clinicians clear guidance when minutes matter.
Can I change my Medical Power of Attorney after it’s signed?
Yes. As long as you retain decision‑making capacity, you can revoke or amend the document by signing a new form and notifying your agent, doctor, and any institutions that hold a copy.
Do I need a lawyer to create a Medical Power of Attorney?
It’s not required, but a lawyer can help tailor the document to complex situations-like combining it with a psychiatric advance directive or ensuring it meets strict state witness rules.
How does a Medical Power of Attorney differ from a Living Will?
A Living Will states specific treatments you want or don’t want, but it cannot adapt to unforeseen circumstances. A Medical Power of Attorney gives a living agent the flexibility to interpret your values in real time, especially for medication choices that weren’t anticipated.
Is a Medical Power of Attorney recognized across state lines?
All 50 states honor a health‑care proxy, but the exact powers can vary. The TREAT Act (2023) aims to standardize recognition, but until it’s law, you should check the destination state’s rules before traveling.
What should I tell my agent about medication preferences?
Share concrete scenarios (e.g., infections, chronic pain), your thresholds for pain‑relief medication, any allergies, and your stance on life‑sustaining drugs like anticoagulants or antibiotics. Written notes plus a brief video can reduce misunderstandings.



Deborah Galloway
October 25, 2025 AT 15:46Thanks for putting this together, it's such a crucial yet overlooked step. I’ve seen families tear apart over meds when there’s no clear guidance. Having a clear MPA means the person you trust can honor your pain thresholds and avoid unwanted treatments. It also gives doctors a concrete reference, which speeds up care when minutes matter.
I always make a point to sit down with my sister and walk through a few realistic scenarios, like infections or post‑surgical pain, so she knows exactly what I’d want.
Charlie Stillwell
October 25, 2025 AT 18:33Wow, another glorified legal form that pretends to solve the chaos of bedside decision‑making – lol 🤦♂️.
Ken Dany Poquiz Bocanegra
October 25, 2025 AT 22:43Setting up a medical POA isn’t as scary as it sounds. Start with a quick chat, list the meds you care about, and let the agent know your pain‑limit numbers. It’s a simple safety net that can spare loved ones from agonizing indecision.
krishna chegireddy
October 26, 2025 AT 00:06The whole system of advance directives is a circus orchestrated by bureaucrats who want to keep us dependent on their paperwork.
They sell us glossy brochures while the real power lies hidden in the fine print that only a handful of lawyers can decipher.
When a hospital receives a Medical Power of Attorney, they often treat it as a suggestion, not a command, unless you have the right form stamped by a notary they recognize.
That is why a doctor’s bedside decision can be swayed by insurance policies that are written in a language no layperson understands.
If you think the TREAT Act will magically standardize everything, think again – the act is still a draft that a few lobbyists are pushing through the Senate.
Meanwhile, pharmaceutical companies are busy promoting new drugs that come with clauses forcing you to sign away your autonomy.
The most dangerous part is that families are often caught in a tug‑of‑war between the proxy’s interpretation and the hospital’s protocol.
Imagine a scenario where a loved one needs IV antibiotics but the proxy, fearing side‑effects, refuses, and the doctor is forced to wait for a court order.
That delay can turn a simple infection into a fatal sepsis, and nobody blames the paperwork.
The only way to cut through this maze is to create multiple copies, store them in both digital vaults and on a USB drive, and ensure the primary care physician has a scanned copy in the EHR.
You should also record a short video explaining your choices, because a human face can sometimes outrank a sterile signature.
Do not rely on a single witness; get two independent witnesses who are not family, because many states invalidate documents if the witnesses have a conflict of interest.
When you travel, double‑check the destination state’s specific rules, as some will not honor a proxy unless it’s notarized in that jurisdiction.
In summary, treat your Medical Power of Attorney like a living document, not a static piece of paper, and keep updating it after every major health event.
Only then can you hope to stay a step ahead of the endless red tape that threatens to strip you of control.
Tamara Schäfer
October 26, 2025 AT 02:53I totally agree with the idea that a personal agent can help us avoid the fight over meds. Its super importent to write down exact dosage limits, like no opioids over 10mg.
I have shared my vidoe with my brother and it made him feel more confiident. Updating the doc every yea is a good habit. Thanks for the clear step‑by‑step!
Tamara Tioran-Harrison
October 26, 2025 AT 03:16It is truly astonishing how a few lines on a form can purportedly safeguard one’s autonomy, despite the myriad ways institutions circumvent such documents.
One might almost commend the legal profession for inventing yet another bureaucratic instrument that the layperson must navigate with a lawyer’s assistance.
Nevertheless, I shall applaud the authors for reminding us that, in theory, a Medical Power of Attorney could prevent the unsavory spectacle of families bickering over antibiotics. 😊
kevin burton
October 26, 2025 AT 06:03From a practical standpoint, after you’ve signed the POA, upload a PDF to the patient portal and hand a printed copy to the primary care office. Most hospitals now request the document during admission, so having it on a thumb drive can speed up the process. Also, remind your agent to keep the contact info for your PCP updated.
Max Lilleyman
October 26, 2025 AT 07:26If you skip the step of discussing concrete medication thresholds, you’re basically signing away your loved ones’ peace of mind 🙄. A good proxy needs clear parameters, otherwise you’re just inviting conflict. 📋
Buddy Bryan
October 26, 2025 AT 08:50Don’t wait for a health crisis to figure out your medication wishes – the paperwork is cheap and the peace of mind is priceless. Get the state form, fill it out while you’re still sharp, and schedule a quick debrief with your agent. Anything less is reckless.
Jonah O
October 26, 2025 AT 10:13They want you to think a POA gives control, but the system always finds a loophole to override it.