Every year, millions of Americans face a brutal choice: pay for their medicine or pay for rent. It’s not a hypothetical. It’s real life. In the U.S., the same pill you can buy for $50 in Canada or $12 in Germany costs $300-or more. And it’s not just insulin or cancer drugs. Even routine medications for high blood pressure or cholesterol have become unaffordable. Why? The answer isn’t simple, but it’s not mysterious either. It’s built into the system.
The System Was Designed This Way
The U.S. doesn’t have high drug prices because of bad luck. It’s because the rules were written to let drugmakers charge whatever they want. Unlike every other developed country, the U.S. government doesn’t negotiate drug prices for Medicare, the largest health program in the nation. That changed in 2003 with the Medicare Modernization Act. Lawmakers specifically banned Medicare from bargaining. The result? Pharmaceutical companies set prices with no real check on them. This isn’t just about Medicare. It’s the foundation of how every other insurer, pharmacy, and patient pays. Private insurers are stuck negotiating with the same companies that set sky-high list prices. And because Medicare can’t negotiate, those list prices become the baseline for everyone else.Who Really Controls the Price?
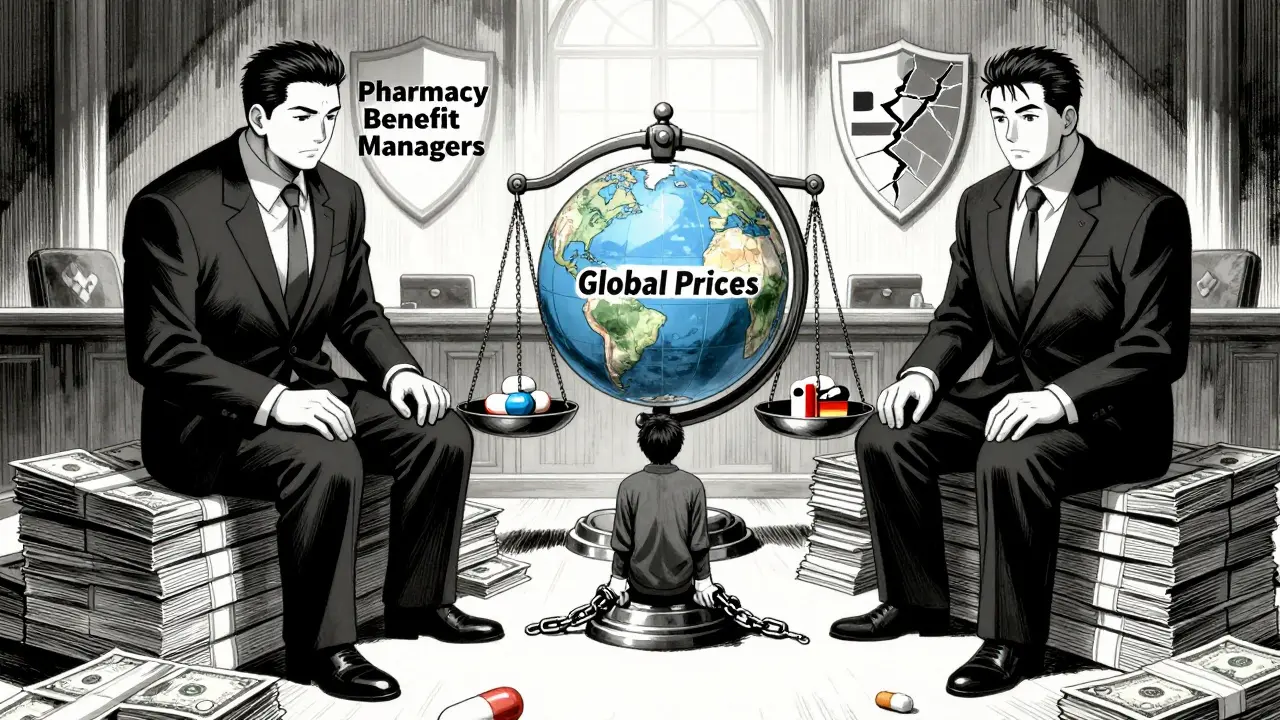
You might think the drugmaker sets the final price. But the real story is messier. Between the manufacturer and the patient, there are middlemen: Pharmacy Benefit Managers, or PBMs. Originally created to cut costs, PBMs now control how drugs are priced and who gets what discount. They’re paid based on rebates-meaning the higher the list price, the bigger their cut. So they push for expensive drugs, even if cheaper alternatives exist. For example, a drug might have a $1,000 list price. The manufacturer gives the PBM a $300 rebate. The PBM keeps $150 and passes $150 to the insurer. The patient still pays $1,000 out of pocket if they haven’t met their deductible. The manufacturer made a profit. The PBM made a profit. The patient? They’re stuck paying the full price. This isn’t a bug. It’s the design.The Numbers Don’t Lie
The U.S. makes up less than 5% of the world’s population-but accounts for nearly 75% of global pharmaceutical profits. That’s not because Americans are sicker. It’s because they’re paying more. For the same exact drug, made in the same factory:- Galzin (Wilson’s disease treatment): $88,800 in the U.S. vs. $1,400 in the U.K.
- Ozempic: $1,000 per month before deals, now $350 after negotiation
- Wegovy: $1,350 per month before, now $350
Specialty Drugs Are Breaking the Bank
The biggest price spikes aren’t coming from old pills. They’re from new, high-tech drugs-especially for obesity, diabetes, cancer, and rare diseases. These are called specialty drugs. They cost tens of thousands a year. In 2024, the U.S. drug market saw net prices jump 11.4%, up from 4.9% the year before. Most of that growth came from just a handful of these drugs. Manufacturers justify these prices by saying they need to recoup R&D costs. But here’s the twist: most of that research was publicly funded. The NIH poured billions into the science behind drugs like Ozempic. The private companies then took that science, patented it, and slapped on a price tag that’s 100x the cost of production.What’s Been Done to Fix It?
The Inflation Reduction Act of 2022 was the first real attempt to change things. Starting in 2026, Medicare can negotiate prices for 10 drugs. By 2029, that number will rise to 20. So far, it’s saved money on 64 drugs by forcing companies to pay rebates if they raise prices faster than inflation. The results? A $2,000 annual cap on out-of-pocket drug costs for Medicare beneficiaries. That’s huge. For someone paying $10,000 a year for insulin, that’s life-changing. But here’s the catch: the 2025 budget bill weakened the negotiation program. Experts estimate it will cost Medicare at least $5 billion more than planned. And the 10 drugs being negotiated? They’re just a drop in the ocean. There are over 10,000 prescription drugs on the market.Why Don’t Other Countries Have This Problem?
Germany, Canada, France, and the U.K. all have systems that set fair prices. They don’t ask manufacturers what they think a drug is worth. They look at what it costs to make, how effective it is, and what other countries pay. Then they negotiate a price. If the company won’t agree, they don’t sell there. In the U.S., no such rule exists. Companies can charge $100,000 for a year of treatment-and there’s no legal limit. No country with universal healthcare lets drugmakers run wild like this.
The Political Divide
Politicians talk a lot about lowering drug prices. But the results are mixed. President Trump promised to bring prices down in 2025. Yet, according to Senator Bernie Sanders’ report, 688 drugs went up in price after he took office. Even after announcing deals on Ozempic and Wegovy, 87 other drugs increased by an average of 8%. The White House says the Inflation Reduction Act is working. Critics say it’s too little, too late. The truth? The system is still rigged. Until Congress removes the ban on Medicare negotiation and forces PBMs to be transparent, prices will keep rising.What’s Next?
The pressure is growing. Patients are angry. Lawmakers are hearing them. But change moves slowly. The next big fight will be over patent laws. Right now, companies extend patents by making tiny tweaks to old drugs-called “evergreening.” That keeps generics off the market for years. Another push is for international reference pricing: making U.S. prices match those in other wealthy countries. Senator Sanders’ Prescription Drug Price Relief Act would do exactly that. It’s not radical. It’s what every other developed nation already does. For now, the system stays broken. Drugmakers profit. PBMs profit. Insurers profit. Patients? They’re the ones skipping doses, splitting pills, or going without.It’s Not About Cost-It’s About Power
At its core, this isn’t a pricing problem. It’s a power problem. The pharmaceutical industry spends over $100 million a year lobbying Congress. They’ve turned a public health issue into a profit machine. And they’ve done it with the full backing of the law. The solution isn’t harder to find. It’s harder to fight. We need Medicare to negotiate. We need PBMs to be transparent. We need to stop letting a handful of companies decide what’s affordable for 330 million people. Until then, the same question will keep coming up: Why do Americans pay so much more-for the same medicine, made in the same place, for the same disease?The answer is simple: because they can.
Why are prescription drugs more expensive in the U.S. than in other countries?
The U.S. is the only developed country that doesn’t let its government negotiate drug prices. Other nations set fair prices based on what the drug costs to make and how effective it is. In the U.S., drugmakers set their own prices with no legal limits. This system lets them charge up to 10 times more than countries like Canada or Germany-even for the exact same pills made in the same factories.
What role do Pharmacy Benefit Managers (PBMs) play in high drug prices?
PBMs were meant to lower costs, but now they profit from high list prices. They get paid based on rebates-so the higher the price, the bigger their cut. They push insurers to favor expensive drugs because those bring bigger rebates, even if cheaper options exist. This creates a perverse incentive: the system rewards higher prices, not lower ones.
Can Medicare negotiate drug prices now?
Yes, but only for 10 drugs starting in 2026, and the number will slowly rise to 20 by 2029. This is the first time Medicare has been allowed to negotiate, thanks to the Inflation Reduction Act. But it’s a small step. With over 10,000 prescription drugs on the market, this covers less than 1% of what Americans take.
Are drug companies justified in charging high prices because of research costs?
Not really. Most of the foundational research for new drugs comes from government-funded science-like the NIH. Companies then patent the results and charge high prices. For example, the science behind Ozempic was largely developed with public money. The company that markets it didn’t pay for the early research but still charges $1,000 a month. That’s not innovation-it’s extraction.
What’s the impact of the $2,000 out-of-pocket cap for Medicare?
It’s a major win for seniors. Before the cap, some Medicare beneficiaries paid over $10,000 a year for just one drug. Now, they won’t pay more than $2,000 annually, no matter how expensive their meds are. This will prevent people from skipping doses or rationing medicine just to afford food or rent.
Why haven’t more drugs been negotiated yet?
The negotiation program is slow and limited. It only started in 2026, and each year only a few drugs are added. Also, the 2025 budget bill weakened the law, reducing its potential savings. Plus, drug companies are fighting back with lawsuits and delays. Real change will take years-and stronger political will.
Do drug prices keep going up even after deals are announced?
Yes. Even after the White House announced deals to lower prices on Ozempic and Wegovy, over 80 other drugs increased in price. In fact, since 2020, hundreds of drugs have seen price hikes despite political promises to lower costs. The system rewards companies for raising prices, not lowering them.
What can patients do right now to lower their drug costs?
Ask your pharmacist about generic alternatives. Use drug discount cards like GoodRx. Compare prices at different pharmacies-some charge far less than others. If you’re on Medicare, check if your drug is part of the new negotiation program. And if you’re struggling to pay, ask your doctor about patient assistance programs from drugmakers. These won’t fix the system, but they can help you survive it.
Is the U.S. the only country where drug prices are unregulated?
Yes. Every other wealthy country has some form of price control-whether it’s direct negotiation, reference pricing, or public health agencies setting limits. The U.S. is the outlier. It’s the only one that lets corporations set prices with no government oversight. That’s why Americans pay more for the same drugs than anyone else.
Will the Inflation Reduction Act fix high drug prices?
It helps, but it’s not a full fix. The $2,000 cap and inflation rebates are important wins. But with only 10 drugs being negotiated in 2026, and the program weakened by Congress, it won’t stop the overall rise in drug spending. Real change requires ending the ban on Medicare negotiation, cracking down on PBMs, and stopping patent abuses. The Inflation Reduction Act is a start-but only a start.




Mike Rose
January 31, 2026 AT 04:38bro why is everything so expensive like i just wanna take my pill and not go broke
Natasha Plebani
January 31, 2026 AT 04:46The structural asymmetry in pharmaceutical pricing mechanisms reflects a captured regulatory regime where rent-seeking behavior is institutionalized via legislative capture-specifically, the Medicare Modernization Act’s explicit prohibition on price negotiation. This isn’t market failure; it’s market design. The PBM-rebate architecture functions as a perverse incentive system that externalizes cost onto the patient while internalizing profit across the supply chain. The result is a classic principal-agent problem where the agent (PBM) maximizes revenue at the expense of the principal (patient).
Moreover, the illusion of innovation is perpetuated by patent evergreening, where trivial modifications to molecular structures extend monopolies beyond the scope of original R&D investment. Publicly funded NIH research is effectively privatized through intellectual property capture, transforming socialized risk into privatized gain. The $100M annual lobbying expenditure isn’t lobbying-it’s tax-funded subsidy extraction.
The Inflation Reduction Act’s incremental negotiation framework is a Band-Aid on a hemorrhage. Twenty drugs out of 10,000? That’s not reform-it’s theater. Until we dismantle the PBM-rebate model and adopt international reference pricing, we’re just rearranging deck chairs on the Titanic of American healthcare.
The real question isn’t why prices are high-it’s why we tolerate a system that commodifies life-saving biology as a speculative asset class.
Adarsh Uttral
February 1, 2026 AT 23:57honestly i dont get why us is like this. in india we get generic meds for like 10 bucks even for cancer stuff. the system is just broken and no one wants to fix it because the rich keep getting richer
April Allen
February 2, 2026 AT 19:25Let’s not forget the role of patent thickets and data exclusivity-these are the real gatekeepers preventing generic entry. The FDA’s fast-track approvals for specialty drugs often come with 12 years of exclusivity under the Biologics Price Competition and Innovation Act, which is longer than most tech products have market relevance.
And while the $2,000 cap is meaningful, it doesn’t touch the 70% of Americans who aren’t on Medicare. Out-of-pocket costs for privately insured patients still operate under the same broken list-price model. PBMs still control formularies based on rebate size, not clinical value.
International reference pricing isn’t radical-it’s rational. Countries like Germany use HTA (Health Technology Assessment) to determine cost-effectiveness thresholds. If a drug doesn’t meet them, it doesn’t get reimbursed. Simple. Transparent. No lobbying needed.
The real scandal? We’re paying for the R&D of drugs that were built on publicly funded science, then paying again for the marketing campaigns that convince doctors to prescribe them. That’s not capitalism-it’s corporate welfare with a side of moral bankruptcy.