
Switching from a brand-name drug to a generic version is supposed to save money-without sacrificing effectiveness. For most people, it works exactly like that. But for some, it doesn’t. And when it doesn’t, the signs can be subtle at first, then suddenly serious. You might feel off, but not sick enough to panic. That’s exactly when you should call your doctor.
Not All Generics Are Created Equal
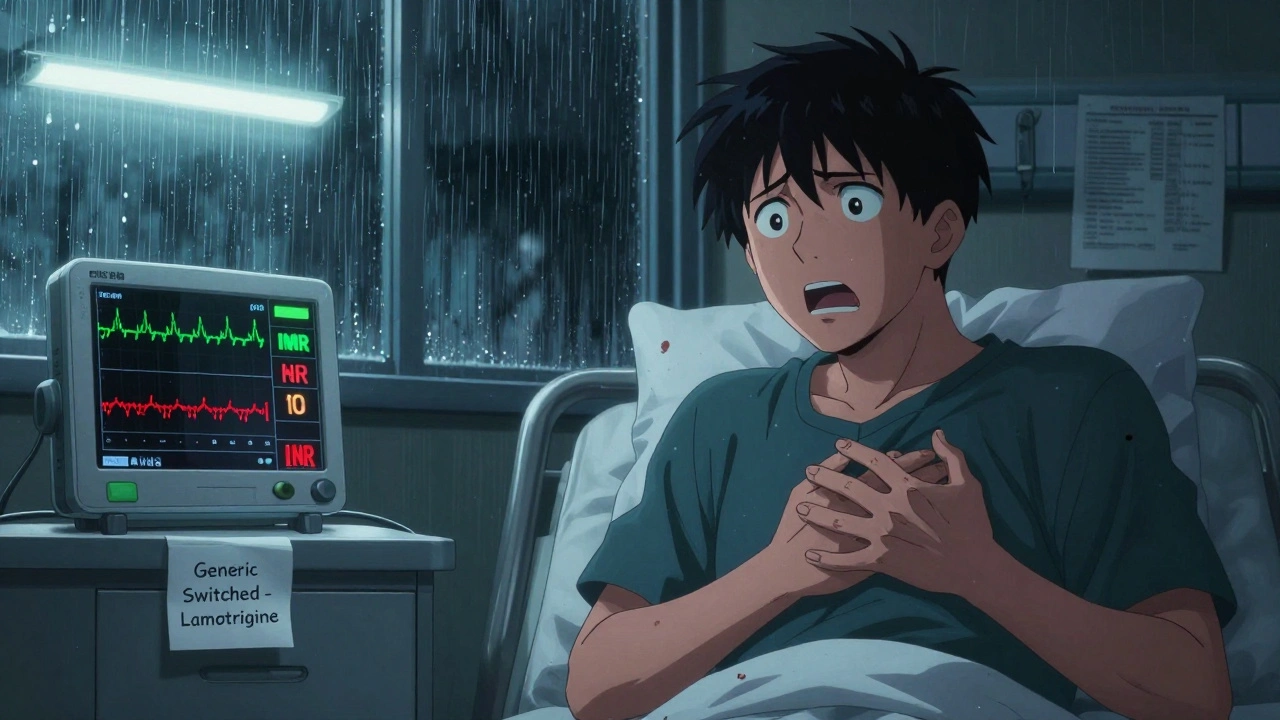
Generic drugs must contain the same active ingredient as the brand-name version, in the same strength and dosage form. The FDA requires them to deliver the same amount of medicine into your bloodstream within a tight range-80% to 125% of the brand-name drug. That sounds precise, right? But here’s the catch: that 45% window allows for real differences in how your body responds, especially with certain drugs.For medications like levothyroxine (for thyroid), warfarin (a blood thinner), or lamotrigine (for seizures or bipolar disorder), even small changes in how much drug gets into your system can throw your whole treatment off balance. These are called narrow therapeutic index drugs. A tiny shift in dosage can mean the difference between control and crisis.
One study found that 15.3% of patients stabilized on brand-name levothyroxine saw their TSH levels jump out of the safe range after switching to a generic. Another showed that patients with epilepsy had a 25% higher chance of having a seizure after switching between different generic versions of lamotrigine. That’s not rare. That’s a pattern.
Warning Signs That Mean You Need to Call Your Doctor
If you’ve recently switched to a generic and you notice any of these, don’t wait. Don’t assume it’s just stress, bad sleep, or aging. Call your doctor within 24 hours:
- Unexplained skin rash, hives, or itching-especially if it spreads or gets worse. This is one of the most common reactions, reported in over 14% of adverse events tied to generic switches. It could mean your body is reacting to a new filler or dye in the pill.
- Persistent nausea, vomiting, or diarrhea-not just a bad stomach bug. If it lasts more than two days and you can’t keep food or water down, it’s not normal. Some generics use different binders or coatings that irritate the gut.
- Sudden fatigue or dizziness-especially if you used to feel fine on the brand-name version. This can signal that your drug levels are dropping too low, or your body isn’t absorbing it properly.
- Changes in how well your medication works-your blood pressure is higher again, your migraines are back, your depression symptoms returned, or your seizures are worsening. If your condition, which was stable for months, suddenly flares up after the switch, that’s a red flag.
- Heart palpitations or chest tightness-this is serious. For people on blood thinners like warfarin or heart meds like valsartan, switching generics has been linked to higher hospitalization rates. Don’t brush this off.
If you experience throat swelling, trouble breathing, or a sudden drop in blood pressure (feeling faint, cold skin, confusion), go to the emergency room immediately. These are signs of anaphylaxis-a rare but life-threatening allergic reaction to an inactive ingredient.
Which Drugs Are Most Likely to Cause Problems?
Not every medication has issues. Most people switch to generic metformin for diabetes or generic sertraline for depression with zero problems. But some drugs have a history of triggering reactions:
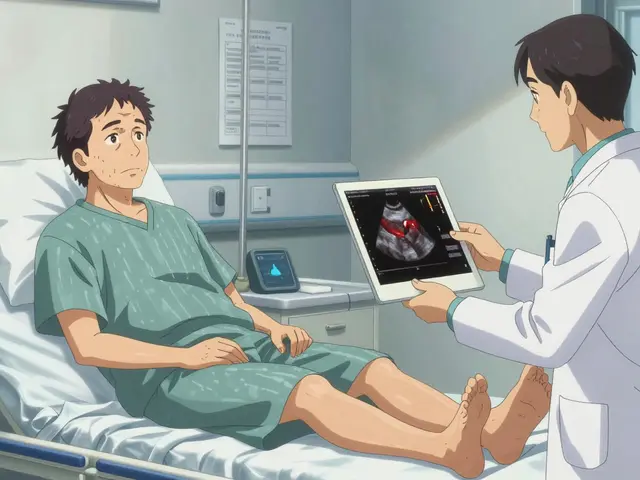
- Levothyroxine (for hypothyroidism): Even small changes in absorption can cause weight gain, fatigue, or heart rhythm issues. TSH levels should be checked 6-8 weeks after switching.
- Lamotrigine (for epilepsy or bipolar disorder): The risk of seizure recurrence or mood episodes spikes after switching between generics. The American Academy of Neurology advises against automatic substitution.
- Warfarin: INR levels must be monitored closely. A shift of just 0.5 can increase stroke or bleeding risk.
- Phenytoin (another seizure drug): Blood levels need to be checked after any switch. The therapeutic range is narrow-10 to 20 mcg/mL.
- Sumatriptan (for migraines): One documented case showed a woman’s migraines returned after switching to generic-until she went back to the brand, and they vanished.
- Clopidogrel (Plavix alternative): Some studies link generic versions to higher rates of heart attacks and hospitalizations, though the reason is still debated.
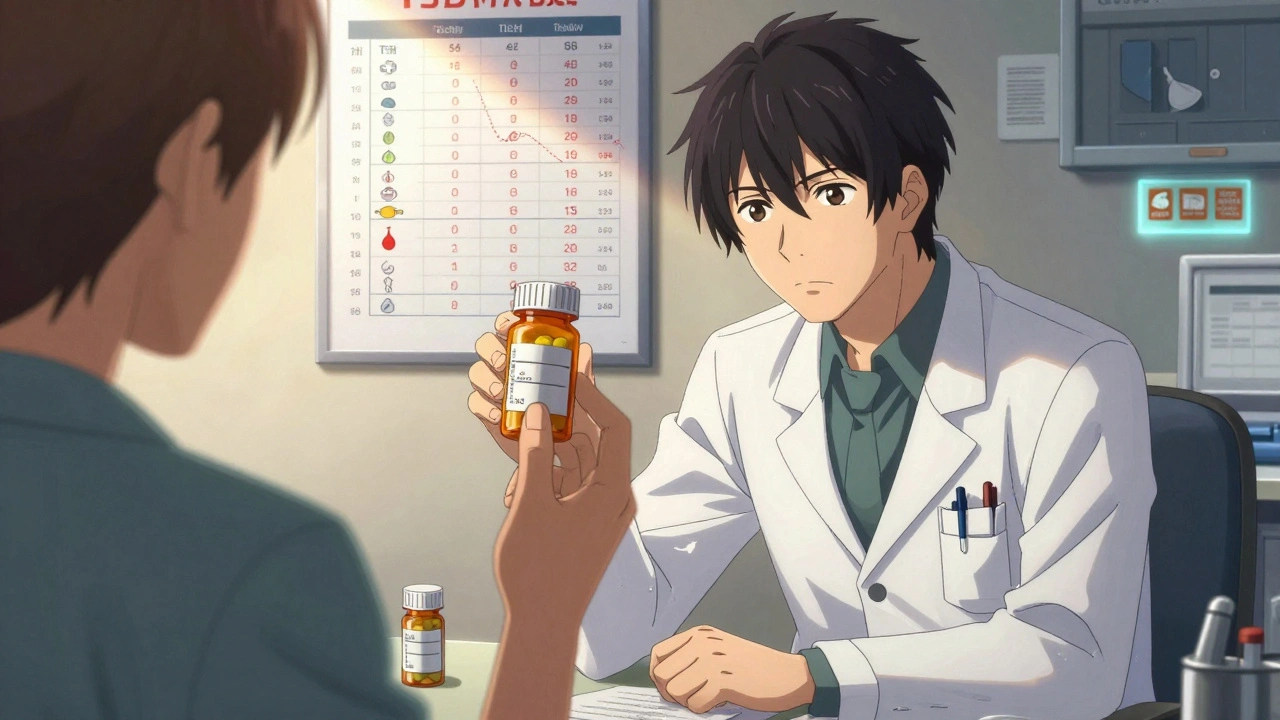
Check the FDA’s Orange Book. If your drug has an “A” rating, it’s considered therapeutically equivalent. A “B” rating means there’s uncertainty. Ask your pharmacist to show you the rating.
What to Do When You Suspect a Problem
Don’t stop your medication on your own. That’s dangerous. Instead:
- Write down your symptoms-when they started, how bad they are, what you were doing when they appeared.
- Check your pill. Look at the shape, color, and imprint. Compare it to your old brand-name pill. If it looks completely different, that’s normal-but still worth noting.
- Call your doctor. Say: “I switched to a generic and I’m having [symptoms]. I’m concerned it’s related.” Don’t wait for your next appointment.
- Ask for a lab test. For thyroid, ask for TSH. For blood thinners, ask for INR. For seizure meds, ask for drug levels. These tests can prove whether the generic is working the same way.
- Request your old brand if needed. Your doctor can write “Dispense as written” or “Do not substitute” on the prescription. Pharmacists must honor this.
In California and 27 other states, pharmacists are required to notify your doctor if they switch you on an NTID drug. If you live in one of those states, you should get a call from your prescriber. If you don’t, ask why.
Why This Happens-And Why It’s Not Just in Your Head
Many people think if the active ingredient is the same, the pill must work the same. But inactive ingredients matter. A generic might use a different filler-like lactose, cornstarch, or a dye-that your body reacts to. Or the coating might dissolve too fast or too slow, changing how your body absorbs the drug.
And yes, some generics are made in factories with lower quality control. In 2023, 18% more generic drugs were recalled than in 2021, mostly because of impurities or inconsistent potency. That’s not common-but it’s not rare either.
It’s not about trusting generics. It’s about trusting your body. If you feel different, you probably are. Science says most people are fine. But science doesn’t know how your body reacts. Only you do.
What You Can Do to Stay Safe
- Always ask your pharmacist: “Is this the same generic I’ve been taking?” If it’s changed, ask why.
- Keep a log of your symptoms and medication changes. Use a notes app or a small notebook.
- Don’t let your doctor assume you’re fine just because you’re on a generic. Push for follow-up tests if you’re on a high-risk drug.
- If you’ve had a bad reaction before, tell your doctor before any future switches.
- For chronic conditions like thyroid disease, epilepsy, or heart failure, consider sticking with the brand if you can afford it. Your health is worth the extra cost.
There’s no shame in asking for the brand-name version. If your insurance won’t cover it, ask your doctor for a prior authorization. Many times, they’ll approve it if you’ve had a documented reaction to a generic.
Can generic drugs really be less effective than brand-name drugs?
For most drugs, yes-they’re equally effective. But for narrow therapeutic index drugs like levothyroxine, warfarin, and lamotrigine, even small differences in absorption can reduce effectiveness or cause side effects. Studies show measurable changes in blood levels and clinical outcomes after switching.
I switched to a generic and feel worse. Should I go back to the brand?
If you notice new or worsening symptoms after switching, contact your doctor. Don’t stop the medication, but ask whether returning to the brand-name version is safe and appropriate. Many patients find their symptoms disappear once they switch back.
Are generic drugs more likely to cause allergies?
Not the active ingredient-but the inactive ingredients (fillers, dyes, preservatives) can trigger allergic reactions. If you’ve never had a rash or swelling before and it started after switching to a generic, that’s a likely cause. Your doctor can test for allergies to common excipients.
How long should I wait before deciding if the generic is working?
For most medications, give it 2-4 weeks. But for drugs like thyroid, blood thinners, or seizure meds, symptoms can appear within days. If you feel worse in the first week, don’t wait-call your doctor. Don’t assume it’ll get better.
Can I ask my pharmacist to give me the same generic I had before?
Yes. You have the right to request the same manufacturer or formulation. Pharmacists can often order a specific generic if you’ve had issues with another. Ask them to check the lot number or manufacturer name on the bottle.
Is it true that some states ban automatic generic substitution for certain drugs?
Yes. In California, New York, and 26 other states, pharmacists must notify your doctor before substituting generics for 12+ high-risk drugs like levothyroxine, warfarin, and phenytoin. If you live in one of these states and weren’t notified, ask why.
Final Thought: Your Body Knows
Generics are a good thing. They save billions every year. But they’re not magic. They’re still drugs. And your body is still you.
If something feels off after a switch, it probably is. Don’t let fear of being "difficult" or "wasting the doctor’s time" stop you from speaking up. The right medication for you isn’t about cost-it’s about safety, stability, and feeling like yourself again.

Constantine Vigderman
December 13, 2025 AT 11:49OMG I switched to generic levothyroxine last month and started feeling like a zombie 😵💫 my hair was falling out, I couldn’t wake up, and my brain felt like mush… I called my doc and they were like ‘it’s just generics’ - NOPE. Got my brand back and I’m human again. If you feel off, TRUST YOURSELF.
Cole Newman
December 15, 2025 AT 06:51LMAO people still act surprised generics can mess them up? Bro, the FDA lets companies use different fillers - cornstarch, lactose, dye, even talc. If you’re allergic to any of that? Congrats, you’re now a human guinea pig. And yeah, some generics are made in India or China with sketchy QA. I’ve seen pills that crumble in your hand. Not a joke.
Casey Mellish
December 15, 2025 AT 07:08As an Aussie who’s had to navigate both our PBS system and the US market, I can confirm: this isn’t just an American issue. We’ve had similar cases with warfarin and lamotrigine here. The science is solid - narrow therapeutic index drugs are a minefield. The problem isn’t generics per se, it’s the lack of mandatory monitoring after substitution. We need better protocols.
Tyrone Marshall
December 15, 2025 AT 15:38There’s a quiet dignity in listening to your body. We’ve been trained to trust systems - insurance, pharmacies, even doctors - but your body doesn’t lie. If you’ve been stable for years and suddenly feel like you’re underwater, that’s not ‘stress’ or ‘aging.’ It’s your physiology screaming. Don’t apologize for asking for your old med. Your health isn’t a line item on a balance sheet.
Emily Haworth
December 16, 2025 AT 21:07EVERY GENERIC IS A LAB EXPERIMENT ON YOU. 😳 I swear the FDA is in cahoots with Big Pharma to keep you hooked on brand names. They know generics cause side effects but let it slide because they get kickbacks from the big pharma companies. I read a whistleblower report once - they test generics on rats but not humans. I’m not taking any more chances. 🚫💊
Tom Zerkoff
December 18, 2025 AT 18:49It is imperative to recognize that therapeutic equivalence, as defined by the FDA’s AB rating system, does not equate to clinical equivalence in all individuals. While the bioequivalence criteria are statistically sound, they are population-based and do not account for inter-individual pharmacokinetic variability. For patients on narrow therapeutic index medications, individualized monitoring is not optional - it is essential.
Yatendra S
December 19, 2025 AT 17:09Life is like a pill - same active ingredient, different coating. Some dissolve fast, some slow. Some make you feel alive, others make you want to disappear. Maybe the problem isn’t the drug… but the system that forces you to swallow it without asking. 🤔
Himmat Singh
December 21, 2025 AT 05:06The premise of this article is fundamentally flawed. The FDA’s bioequivalence standards are robust, peer-reviewed, and validated across decades. The anecdotal reports of adverse effects are confounded by placebo/nocebo effects, poor adherence, and regression to the mean. To suggest that generics are inherently less safe is scientifically indefensible and dangerously misleading.
kevin moranga
December 22, 2025 AT 12:25Hey, I get it - switching generics feels like swapping your favorite coffee for a store-brand version that tastes kinda off. But here’s the thing: most people are fine. I switched to generic sertraline and felt nothing. BUT - if you’re on warfarin or thyroid meds? Yeah, pay attention. I’ve got a buddy who went from 2.5 INR to 6.2 after a switch - nearly bled out. So don’t panic, but don’t ignore it either. Keep a journal, check in with your doc, and if something feels weird? Speak up. You’ve got this 💪
Alvin Montanez
December 23, 2025 AT 09:57Let’s be brutally honest: this isn’t about safety. It’s about privilege. People who can afford brand-name meds are the ones complaining. Meanwhile, millions rely on generics to survive. You want to keep your expensive thyroid med? Fine. But don’t act like your personal discomfort is a public health crisis. The system works for 95% of people. Stop being entitled and start being grateful you’re not choosing between insulin and rent.
Lara Tobin
December 25, 2025 AT 05:03I switched to generic lamotrigine and started crying for no reason… like, sobbing in the grocery store. I felt so guilty, like I was being dramatic. But I called my doctor and she said, ‘thank you for telling me.’ I didn’t know I was allowed to say that. I’m not weak for needing the brand. I’m brave for speaking up. 🫂
Jamie Clark
December 26, 2025 AT 03:29You’re all missing the point. This isn’t about generics. It’s about a broken healthcare system that treats patients like data points. Doctors don’t monitor you. Pharmacists don’t care. Insurance companies push the cheapest option. And when you get sick? You’re blamed for ‘not following instructions.’ The real villain isn’t the pill - it’s the indifference.
Keasha Trawick
December 27, 2025 AT 00:16Imagine your brain as a symphony. Levothyroxine? The conductor. Switch the baton - even slightly - and suddenly the violins are screeching, the timpani’s off-beat, and the whole damn orchestra collapses. That’s what happens with NTID drugs. The active ingredient is the same, but the *delivery*? That’s where the magic - and the mayhem - lives. I’ve seen patients go from ‘normal’ to ‘intensive care’ because a pharmacist swapped a tablet without a whisper. This isn’t paranoia. It’s pharmacology.
Webster Bull
December 28, 2025 AT 02:05Trust your gut. Check your pill. Ask your doc. Simple. 🤝