
Many people don’t realize that common prescriptions can quietly damage their hearing-sometimes permanently. If you’re on long-term antibiotics, chemotherapy, or even certain antidepressants, you might be at risk for ototoxic medications without even knowing it. The damage doesn’t always show up right away. It starts with a faint ringing in your ears, or difficulty hearing high-pitched sounds like birds chirping or children’s voices. By the time you notice it, the harm is often irreversible.
What Exactly Is Ototoxicity?
Ototoxicity means poison to the ear. It happens when certain drugs attack the delicate hair cells inside your inner ear. These cells don’t regenerate. Once they’re gone, your hearing doesn’t come back. The cochlea, which turns sound into electrical signals for your brain, is especially vulnerable. So is the vestibular system, which controls balance. That’s why some people on ototoxic drugs don’t just lose hearing-they also feel dizzy, unsteady, or nauseous. This isn’t rare. Around 600 prescription drugs are known to carry this risk, according to the American Speech-Language-Hearing Association. Some are life-saving. Cisplatin, for example, treats testicular, ovarian, and lung cancers. Gentamicin saves lives in severe infections. But they come with a hidden cost: up to 60% of patients on cisplatin develop hearing loss. For gentamicin, the rate can hit 63% after more than a week of use.Which Medications Are the Worst Offenders?
Not all ototoxic drugs are created equal. Some are more dangerous than others, and the risk depends on how much you take and how long you’re on them.- Aminoglycoside antibiotics - Gentamicin, tobramycin, amikacin, and streptomycin are the big ones. Used for serious infections like sepsis or drug-resistant TB, they can cause permanent hearing loss in 20-63% of patients. Damage usually starts at high frequencies (8,000-12,000 Hz), which is why standard hearing tests often miss it-they only go up to 4,000 Hz.
- Cisplatin chemotherapy - This drug is a major cause of hearing loss in cancer patients. Between 30% and 60% of adults and up to 80% of children develop hearing damage. What makes cisplatin worse is that it sticks around in the inner ear for months after treatment ends, slowly killing more cells. Kids are especially at risk-undetected hearing loss can delay speech and language development by 35%.
- Loop diuretics - Furosemide (Lasix) and bumetanide, used for heart failure or kidney issues, can cause temporary or permanent hearing loss, especially at high doses or when combined with aminoglycosides.
- Some antidepressants - Tricyclics like amitriptyline and SSRIs like sertraline and fluoxetine have been linked to tinnitus and hearing changes. The risk is lower, but it’s real. Patients often report ringing that started after beginning these meds.
- High-dose aspirin and NSAIDs - These can cause temporary hearing loss or tinnitus. It usually goes away when you stop taking them, but long-term heavy use may lead to lasting damage.
How Do These Drugs Actually Damage Your Ears?
It’s not just one mechanism. Different drugs attack in different ways:- Oxidative stress - Cisplatin and aminoglycosides flood the inner ear with free radicals. These unstable molecules tear apart the hair cells’ DNA and mitochondria, causing them to die.
- Reduced blood flow - Some drugs narrow blood vessels feeding the cochlea, starving the cells of oxygen.
- Direct toxicity - Aminoglycosides bind directly to hair cell receptors, triggering cell death.
- Neurotransmitter disruption - Certain drugs interfere with the chemical signals between hair cells and the auditory nerve.
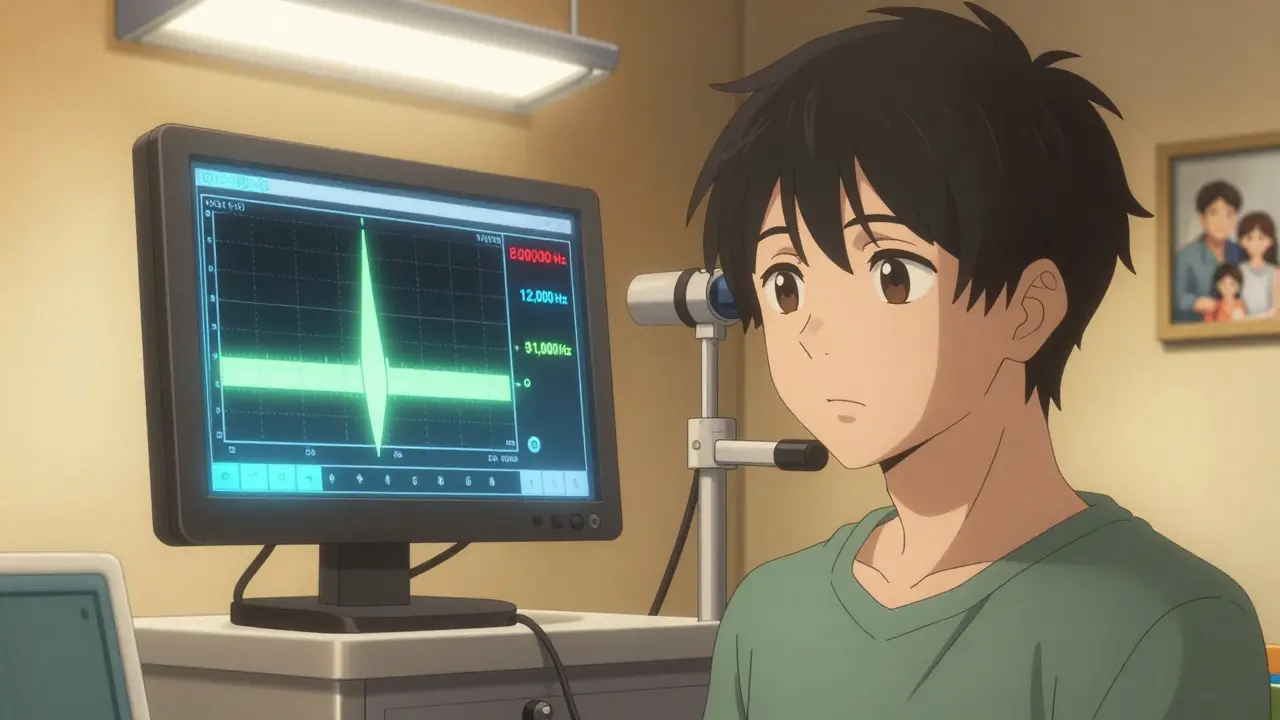
Why Standard Hearing Tests Often Miss the Problem
Most clinics test hearing only up to 4,000 Hz. That’s not enough. Ototoxic damage shows up first at 8,000 Hz and beyond. A patient on cisplatin might lose 40 dB of hearing at 8,000 Hz after their third treatment cycle-but their doctor won’t know unless they specifically test those frequencies. One Reddit user shared their story: after their third cisplatin cycle, they suddenly couldn’t hear their alarm clock. A standard audiogram showed nothing wrong. Only a high-frequency test revealed severe loss at 6,000 Hz. Their oncologist had never heard of the need for extended-range testing. This is a gap in care. Only 45% of U.S. cancer centers follow recommended ototoxicity monitoring guidelines. Patients are being left in the dark.How to Monitor for Ototoxicity-And What Works
Early detection saves hearing. Here’s what real monitoring looks like:- Baseline audiogram - Before starting cisplatin, gentamicin, or other high-risk drugs, get a full hearing test that includes 8,000-12,000 Hz. If you’re getting cisplatin, this is non-negotiable.
- Serial high-frequency testing - For cisplatin: test after each cycle. For aminoglycosides: test after every 3-5 doses. Look for changes at 8,000 Hz and above.
- Otoacoustic emissions (OAE) - This test measures sound produced by healthy hair cells. If those sounds weaken, it means damage is happening-even before you lose hearing on a standard test. OAE is 25% more sensitive than regular audiometry.
- Vestibular testing - If you’re dizzy or unsteady, a balance test (like VNG or ENG) can detect inner ear damage before it affects hearing.
- Genetic screening - Some people have a mitochondrial DNA mutation (m.1555A>G) that makes them 100 times more likely to go deaf from aminoglycosides. Testing isn’t routine yet, but if you or a family member had sudden deafness after antibiotics, ask about it.
What Can Be Done If Hearing Loss Starts?
Once hair cells die, they’re gone. But you can stop the damage before it spreads.- Adjust the dose - Sometimes lowering the amount or spacing out doses helps.
- Switch medications - For cancer, carboplatin is less ototoxic than cisplatin (though not always as effective). For infections, vancomycin is a safer alternative to gentamicin in many cases.
- Use otoprotective agents - In November 2022, the FDA approved sodium thiosulfate (Pedmark) for children with liver cancer on cisplatin. It reduced hearing loss by 48%. Trials are ongoing for N-acetylcysteine to protect against aminoglycoside damage.
- Stop the drug - If hearing loss is detected early, stopping the medication may prevent further damage.
The Bigger Picture: Why This Matters
About 15 million Americans take ototoxic drugs each year. Cisplatin alone is given to over 500,000 cancer patients annually. The economic cost of medication-induced hearing loss? Over $1 billion in the U.S. each year-due to hearing aids, therapy, lost work, and social isolation. Children with cancer who develop hearing loss are more likely to fall behind in school. Adults lose jobs, relationships, and independence. Tinnitus alone can ruin sleep, concentration, and mental health. And the problem is growing. The WHO predicts a 22% rise in aminoglycoside use for drug-resistant TB by 2027. That could mean 300,000 more cases of preventable hearing loss each year.What You Should Do
If you’re prescribed any of these drugs:- Ask: “Is this medication known to affect hearing?”
- Ask: “Will you be monitoring my hearing with high-frequency tests?”
- Ask: “Is there a less ototoxic alternative?”
- Keep a journal: Note any ringing, fullness in ears, dizziness, or trouble hearing high voices.
- Insist on a baseline hearing test before starting treatment.




Lawrence Jung
January 12, 2026 AT 13:34People think doctors have it all figured out but half the time they’re just guessing and hoping you don’t notice the ringing until it’s too late
Alice Elanora Shepherd
January 13, 2026 AT 05:08Thank you for this incredibly detailed and necessary post. I’ve seen too many patients dismissed when they report tinnitus after chemotherapy-doctors often assume it’s ‘just stress.’ High-frequency audiometry should be standard, not optional. Please share this with your oncologist, and if they don’t know about OAE testing, ask for a referral to an audiologist who specializes in ototoxicity.
Christina Widodo
January 13, 2026 AT 20:11Wait so you’re telling me my weird hearing issues after starting Zoloft weren’t just in my head? I’ve been too embarrassed to mention the ringing to my therapist, but now I’m going to bring it up. Also-can anyone recommend a good audiologist who does 12k Hz tests? My local clinic only does the basic stuff.
Prachi Chauhan
January 15, 2026 AT 10:38Doctors in India also ignore this. My uncle got gentamicin for pneumonia and lost his hearing in weeks. No one warned him. No one tested him. Now he sits in silence and thinks he’s going crazy. Why is this not taught in med school? Why is money more important than ears?
Katherine Carlock
January 17, 2026 AT 02:11My mom is on cisplatin right now and we just got her baseline test done last week. I had no idea this was even a thing until I read your post. We’re going to push for the high-frequency tests after every cycle. Also, I just found out about Pedmark-my oncologist didn’t mention it. I’m going to ask about it tomorrow. Thank you for giving me the words to ask.
Sona Chandra
January 18, 2026 AT 05:29THIS IS WHY MEDICINE IS A SCAM. THEY DON’T CARE IF YOU GO DEAF AS LONG AS YOU SURVIVE. YOUR HEARING IS A LUXURY. YOUR LIFE IS THE ONLY THING THAT MATTERS. BUT WHAT KIND OF LIFE IS SILENCE? THEY’RE KILLING US SLOWLY AND CALLING IT TREATMENT
Jennifer Phelps
January 18, 2026 AT 20:57I had tinnitus after a month of ibuprofen. Thought it was stress. Stopped taking it. Two weeks later it was gone. But now I’m paranoid about every pill I take. Is aspirin safe at 81mg? Should I avoid Advil forever?
beth cordell
January 19, 2026 AT 07:14Just shared this with my whole family 🥺🙏 My cousin’s kid got cisplatin and now needs hearing aids at age 7. No one knew this could happen. We’re all going to push for testing now. Also-anyone know if there’s a phone app that tests 8k Hz? I want to track mine at home 😅
Lauren Warner
January 19, 2026 AT 17:59Let’s be real. The pharmaceutical industry doesn’t want you to know this. They profit from treating the side effects-hearing aids, tinnitus meds, therapy-more than they do from preventing them. They’ll keep pushing cisplatin because it works. They’ll keep ignoring the 60% loss rate because it’s easier than changing the protocol. This isn’t negligence. It’s economics.
Konika Choudhury
January 19, 2026 AT 20:23Why are we listening to Americans talk about hearing loss? In India we have real problems like clean water and electricity. This is first world whining. Take your pills and stop complaining
Darryl Perry
January 20, 2026 AT 14:49Source? 60% hearing loss from cisplatin? Cite the study. Also, why is this not in the FDA label? If it’s so common, why isn’t it mandated?
Windie Wilson
January 22, 2026 AT 14:02So… you’re saying my grandma’s hearing loss after her chemo wasn’t just ‘old age’? 😳 I’ve been calling her ‘dear’ too loudly for years. I thought she was just being dramatic. Turns out she was just… deafened by medicine. Thanks for the guilt, post. 🙃