Steroid Insulin Adjustment Calculator
Steroid Insulin Adjustment Calculator
Calculate your insulin adjustment needs when taking steroids. This tool helps you safely manage steroid-induced hyperglycemia based on your specific treatment plan.
Your Current Information
Steroid Half-Life Guide
- Prednisone 18-36 hours
- Hydrocortisone 8-12 hours
- Dexamethasone 36-72 hours
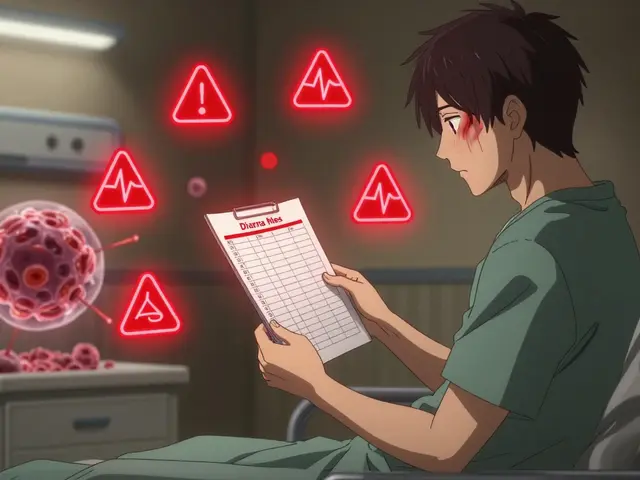
When you start taking steroids - whether it’s prednisone for an autoimmune flare, hydrocortisone after surgery, or dexamethasone for inflammation - your blood sugar can spike overnight. For someone with diabetes, this isn’t just inconvenient. It’s dangerous. Steroid hyperglycemia is real, common, and often misunderstood. Up to 86% of patients on high-dose steroids will have at least one episode of high blood sugar, and nearly half stay above 140 mg/dL for days. The problem? Most doctors don’t adjust insulin right away. And that’s where things go wrong.
Why Steroids Raise Blood Sugar So Fast
Steroids don’t just make you retain water or gain weight. They mess with your body’s entire glucose system. Glucocorticoids - the active type in steroids like prednisone and methylprednisolone - block insulin from doing its job. Your muscles and fat cells stop absorbing glucose. Your liver starts pumping out more sugar. And your pancreas? It gets confused. Insulin production drops, even when blood sugar is sky-high. This isn’t like regular type 2 diabetes. In type 2, insulin resistance builds slowly over years. With steroids, it happens in hours. And the biggest spike? Not in the morning. It’s after breakfast and lunch. That’s because most steroids are taken once daily in the morning. Their peak effect hits 4 to 8 hours later - right when you’re digesting your biggest meals.Who’s at Highest Risk?
Not everyone on steroids gets hyperglycemia. But some people are far more likely to. If you already have type 2 diabetes, your risk jumps to over 70%. Even if you’ve never had diabetes before, you could develop steroid-induced diabetes if you’re:- Over 65 years old
- Overweight (BMI 30 or higher)
- Have a family history of diabetes
- Been on steroids for more than 5 days
- Taking high doses - 20 mg or more of prednisone daily
- Also on tacrolimus or other transplant drugs
How Much More Insulin Do You Need?
There’s no one-size-fits-all answer. But the numbers don’t lie. If you’re on 20 mg of prednisone a day, your insulin needs will likely go up by 30-50%. At 50 mg? Expect a 100% increase. At 100 mg or more? Some patients need triple their usual dose. The key is knowing where to add it. Most of the extra insulin isn’t for your background (basal) rate - it’s for meals. That’s because steroids cause post-meal spikes, not all-day highs. So if you normally take 10 units of rapid-acting insulin before breakfast, you might need 15-20 units. Before lunch? Maybe 25. Dinner? Often unchanged, because steroid levels are dropping by then. For people on long-acting insulin like glargine or detemir, the increase is smaller - usually 10-20%. But if you’re on a pump, you’ll need to raise your basal rate for 4-8 hours after your steroid dose. That’s something most people miss.What About Oral Diabetes Medications?
Most oral drugs don’t cut it when steroids are in the picture. Metformin? It helps a little with insulin resistance, but it won’t stop a 300 mg/dL spike. Sulfonylureas like glimepiride? Risky. They force your pancreas to release insulin - but steroids are already shutting that down. You could end up with low blood sugar when the steroid wears off. GLP-1 agonists like semaglutide? They’re great for weight loss and long-term control, but they don’t work fast enough for acute steroid spikes. SGLT2 inhibitors? Avoid them. Steroids raise your risk of dehydration and ketoacidosis. Add an SGLT2 inhibitor, and you’re playing with fire. Bottom line: insulin is the only reliable tool during steroid therapy. Everything else is a backup - or a hazard.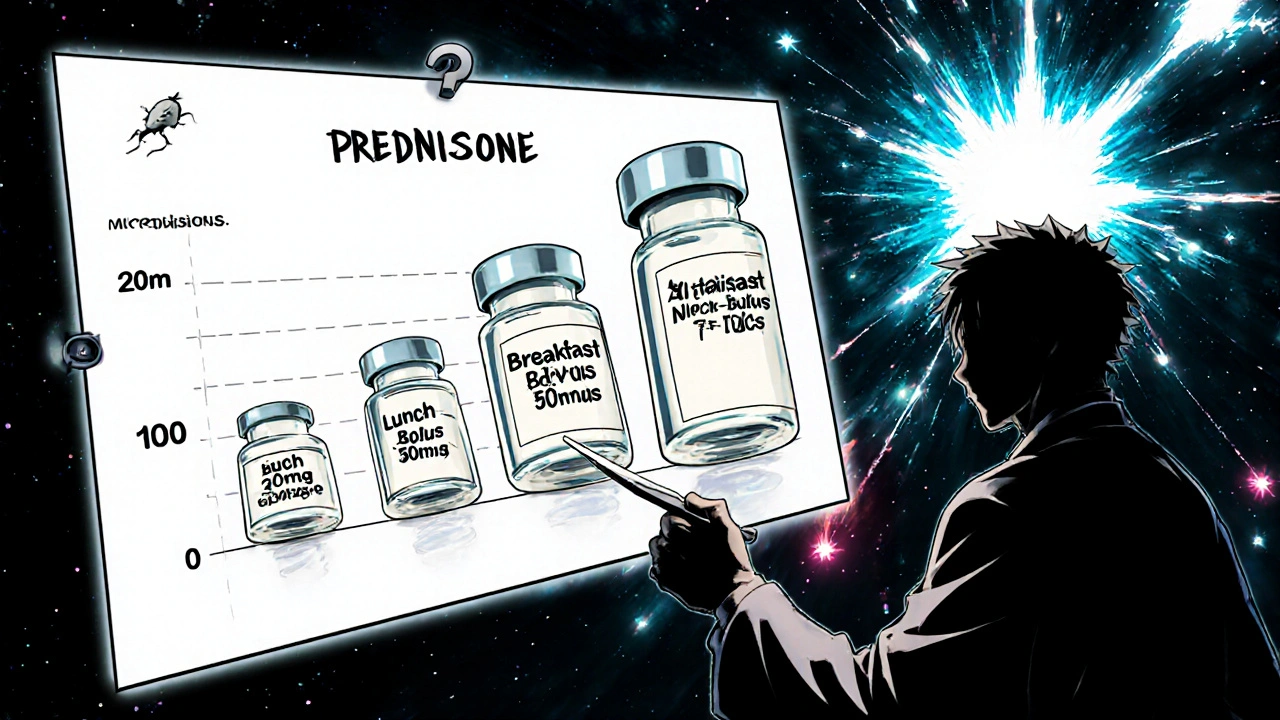
When to Monitor - And How Often
Fasting glucose? Useless. You’ll miss 15-20% of the spikes. You need to check your blood sugar after meals. Specifically:- Before breakfast
- 2 hours after breakfast
- Before lunch
- 2 hours after lunch
- Before dinner (optional, but helpful)
- At bedtime
The Tapering Trap
This is where most people get hurt. When the steroid dose starts coming down - say, from 40 mg to 30 mg to 20 mg - your body starts recovering. Insulin sensitivity comes back. But your insulin dose? It’s still at the high level from earlier. Result? Severe hypoglycemia. In one study, 22% of patients had dangerous low blood sugar episodes during steroid tapering - because their insulin wasn’t reduced. At Johns Hopkins, 18% of hospital readmissions within 30 days of steroid discharge were due to this exact mistake. Here’s the rule: for every 10 mg you reduce in prednisone equivalent, cut your total daily insulin by 10-20%. Don’t wait for a low to happen. Be proactive. If you’re on 80 units a day during peak steroid use, and your dose drops from 30 mg to 20 mg, you might need to cut 10-15 units right away.Real-Life Scenarios
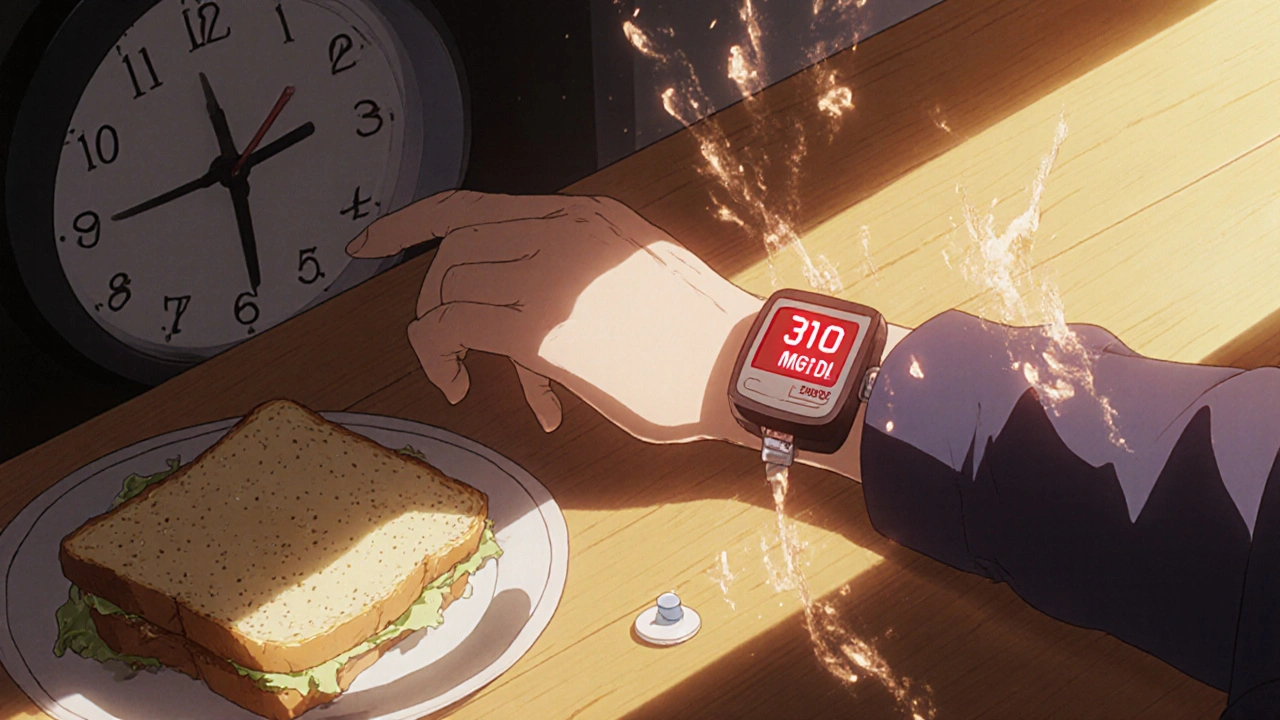
Sarah, 58, has type 2 diabetes. She takes 20 units of Lantus and 8 units of Humalog before breakfast. She’s prescribed 40 mg of prednisone for a severe asthma attack. Within 48 hours, her morning glucose jumps to 220. Her lunch glucose hits 310. Her doctor tells her to “just take more insulin.” She doubles her Humalog to 16 units. Her blood sugar drops to 180 at lunch - but then crashes to 52 at 4 p.m. Why? Because the steroid hadn’t peaked yet, and she didn’t adjust her basal dose. A better plan: increase Lantus by 20% (to 24 units), increase Humalog before breakfast to 14, and add 12 units before lunch. Check glucose at 2 hours after each meal. Don’t touch dinner insulin yet. When the prednisone drops to 20 mg, reduce total insulin by 15% - and keep watching. Another case: Mark, 42, post-kidney transplant. On tacrolimus and 25 mg prednisone. His glucose hits 280. His endocrinologist adds a basal-bolus insulin plan - 20 units Lantus, 8 units Humalog with breakfast, 10 with lunch. He checks his glucose every 2 hours. His CGM shows a 140 mg/dL spike at 11 a.m. - right when the prednisone peaks. He adjusts his lunch insulin to 14 units. Within 3 days, his time-in-range improves from 45% to 78%.
What Hospitals Are Doing Right
Top hospitals now use protocols built into their electronic systems. The EndoTool system, used in over 280 U.S. hospitals, automatically suggests insulin doses based on steroid type, dose, and current glucose. One study showed a 27% drop in hyperglycemia rates. Glytec’s app, used in major academic centers, cuts hypoglycemia during tapering by 33%. The Joint Commission now requires hospitals to have a written plan for managing steroid-induced hyperglycemia. If you’re admitted and on steroids, you should get a glucose monitoring plan before your first dose.What You Can Do Today
If you’re starting steroids:- Ask your doctor for a glucose monitoring plan before you start.
- Know your steroid’s half-life: hydrocortisone (8-12 hrs), prednisone (18-36 hrs), dexamethasone (36-72 hrs). Shorter half-life = more frequent adjustments.
- Switch to a basal-bolus insulin plan if you’re not already on one.
- Use a CGM if you can - even temporarily.
- Check blood sugar 2 hours after every meal - not just fasting.
- Write down your steroid dose and insulin doses daily.
- When tapering, reduce insulin by 10-20% for every 10 mg drop in prednisone equivalent.
- Never stop insulin without talking to your doctor - even if your sugar seems normal.
The Bottom Line
Steroid hyperglycemia isn’t a glitch. It’s a predictable, well-documented effect. And it’s treatable - if you act early. Waiting until your glucose hits 400 mg/dL is too late. Adjusting insulin the same way you would for regular diabetes will fail. You need to think in terms of timing, peak effects, and tapering risks. The goal isn’t to get your sugar to 90. It’s to stay in range while you heal. And that means being smarter than the numbers - not just reacting to them.Can steroids cause diabetes in people who never had it before?
Yes. Steroids can trigger new-onset diabetes, known as steroid-induced diabetes mellitus (SIDM). This happens in up to 40% of people on high-dose or long-term steroid therapy, especially if they have risk factors like obesity, older age, or a family history of diabetes. It’s not always permanent - many people return to normal glucose levels after stopping steroids - but some develop lasting type 2 diabetes.
Why is my blood sugar high only after meals on steroids?
Steroids cause insulin resistance mainly after eating, because they interfere with how your body uses glucose from food. They also spike liver glucose production right when you’re digesting. Since most steroids are taken in the morning, the peak effect hits 4-8 hours later - right after breakfast and lunch. That’s why fasting glucose can look normal while your post-meal numbers are sky-high.
Should I stop my oral diabetes meds when I start steroids?
Don’t stop them without talking to your doctor. But most oral medications won’t control steroid-induced spikes. Metformin may help a little, but insulin is the only reliable tool. Sulfonylureas and SGLT2 inhibitors can be dangerous during steroid use - they increase risks of low blood sugar or ketoacidosis. Insulin is safer and more effective during this time.
How do I know when to reduce my insulin during steroid tapering?
Reduce your total daily insulin by 10-20% for every 10 mg drop in prednisone (or equivalent). For example, if you’re going from 30 mg to 20 mg of prednisone, cut insulin by 10-20%. Monitor glucose closely - especially at night and before meals. If you’re using a CGM, look for falling trends. Never wait for a low to happen before reducing insulin.
Do I need a continuous glucose monitor (CGM) if I’m on steroids?
It’s not required, but it’s highly recommended. CGMs show you real-time trends and hidden spikes - especially after meals when steroids hit hardest. People using CGMs during steroid therapy adjust insulin 37% more accurately than those using fingersticks alone. If you’re on high-dose steroids for more than 5 days, a CGM can prevent dangerous highs and lows.
Can I use insulin pumps during steroid therapy?
Yes, and many people find them helpful. Pumps let you adjust basal rates in real time. If you take prednisone in the morning, you can increase your basal rate for the next 6-8 hours to match the steroid’s peak effect. You can also program temporary bolus increases for meals. Just make sure your care team helps you set up the right profiles - and remembers to dial them back when the steroid tapers.
Are there any natural ways to lower blood sugar while on steroids?
Diet and exercise help - but they won’t override the effects of steroids. Eating low-carb meals can reduce post-meal spikes. Staying hydrated and checking magnesium levels (if low, supplement under medical supervision) can help too. But no supplement, herb, or diet trick replaces insulin when steroids are driving your blood sugar up. Trying to manage it without insulin can lead to dangerous complications like DKA.
How long does steroid-induced hyperglycemia last?
It lasts as long as the steroid is active in your system - and sometimes a few days after. For short courses (5-7 days), blood sugar usually returns to normal within 1-2 weeks after stopping. For long-term users, it can take months. Some people never fully recover and end up with permanent type 2 diabetes. The key is managing it well during treatment to protect your pancreas and insulin sensitivity.


Shirou Spade
November 24, 2025 AT 04:29Steroids are like a nuclear option for inflammation - brilliant when you need them, catastrophic if you don’t plan for the fallout. It’s not just about insulin numbers. It’s about timing, rhythm, the body’s silent language. We treat glucose like a dial to turn, but it’s a tide. And steroids? They’re the moon pulling it out of sync. You don’t just dose more insulin - you learn to dance with the rhythm of a broken clock.
And yet, we still act like this is a patient failure. No. It’s a system failure. Doctors don’t get trained in this. Nurses aren’t equipped. Pharmacies don’t warn. We’re throwing people into a storm with a paper umbrella and calling it ‘self-management.’
Lisa Odence
November 26, 2025 AT 03:15It is absolutely imperative to underscore, with the utmost scientific rigor and clinical precision, that the pathophysiology of steroid-induced hyperglycemia is not merely a transient perturbation of glucose homeostasis - it is, in fact, a profound, multi-systemic dysregulation of insulin signaling cascades, gluconeogenic enzyme upregulation, and peripheral insulin resistance mediated via glucocorticoid receptor binding in hepatic, adipose, and skeletal muscle tissues. Furthermore, the pharmacokinetic half-life of the administered corticosteroid (e.g., prednisone at 18–36 hours versus dexamethasone’s 36–72 hours) directly correlates with the duration and magnitude of metabolic derangement, necessitating a tiered, algorithm-driven insulin titration protocol that accounts for peak serum concentration timelines, meal timing, and glycemic variability indices. Failure to implement such a protocol constitutes a breach of standard-of-care guidelines as delineated by the American Diabetes Association (ADA) and the Endocrine Society, and may result in iatrogenic harm, including but not limited to diabetic ketoacidosis, hyperosmolar hyperglycemic state, and increased hospital readmission rates. 📊🩸📉
Patricia McElhinney
November 27, 2025 AT 09:35Ugh. Another post full of half-truths and lazy advice. You say 'insulin is the only reliable tool' - well DUH. But you don't mention that 70% of these patients are obese, sedentary, and eating donuts while on prednisone. No wonder their sugars spike. You're blaming the drug, not the lifestyle. And don't even get me started on CGMs - if you can't afford a $1000 device, maybe you shouldn't be managing diabetes in the first place. And where's the warning about SGLT2 inhibitors? Oh right - because you're too busy being 'nice' to tell people they're playing Russian roulette with DKA. 🤦♀️
Dolapo Eniola
November 28, 2025 AT 23:25Man, this whole thing is so American. You people treat diabetes like it’s a software bug you can patch with insulin. In Nigeria, we don’t have CGMs, we don’t have pumps, we don’t have endocrinologists on speed dial. We use what we got - bitter leaf tea, neem, and prayer. And guess what? We survive. You’re overcomplicating it. Steroids spike sugar? Then eat less carbs. Simple. No fancy math. No 6 checks a day. Just eat clean, move, and trust God. Why do you need a machine to tell you your blood is sweet? Your body already knows. 🇳🇬🙏
Agastya Shukla
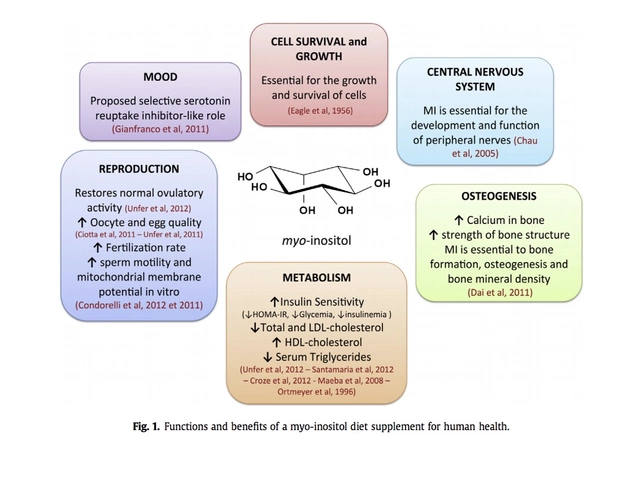
November 29, 2025 AT 12:49Interesting breakdown. I’d like to add a nuance: magnesium’s role is understated. A 2021 study in *Diabetes Care* showed that patients with serum Mg <0.8 mmol/L had 2.3x higher odds of steroid-induced hyperglycemia, independent of BMI or dose. And in populations with high processed food intake - like urban India - this is rampant. Supplementing with 300–400 mg elemental magnesium daily, under supervision, may blunt the spike by 15–20%. Not a replacement for insulin, but a metabolic stabilizer. Also, cortisol’s diurnal rhythm matters - morning dosing aligns with natural peaks, but the 4–8h lag is the real killer. Timing meals to avoid the steroid surge window is critical. 🧬
Pallab Dasgupta
November 29, 2025 AT 23:26YOOOO. I just got prescribed 40mg prednisone for my eczema and I’m already at 310 after lunch. I thought I was doing great on metformin. Turns out I’m just a walking glucose bomb. This post is FIRE. I’m printing it out and handing it to my doc tomorrow. I’ve been checking my sugar after every meal like a maniac - and yeah, the spike hits right after lunch. I’m adding 10 units of Humalog to lunch and upping my Lantus by 15%. I’m scared as hell, but at least I’m not flying blind anymore. If you’re on steroids and reading this - you’re not alone. We got this. 💪🩸🔥
Ellen Sales
December 1, 2025 AT 06:57When you’re on steroids, your body isn’t broken - it’s just doing what it’s told. The liver isn’t being rebellious. The pancreas isn’t lazy. The muscles aren’t stubborn. They’re just responding to a chemical signal that says: ‘Flood the system. Now.’ So why do we pathologize it? Why do we call it ‘poor control’? It’s not control. It’s chemistry. And if your doctor doesn’t get that - find a new one. I’ve seen people get blamed for their numbers while the steroid dose stays unchanged. That’s not medicine. That’s punishment. And the tapering? That’s the quiet killer. You’re not ‘getting better’ - you’re in a metabolic minefield. Slow down. Watch. Adjust. Don’t celebrate the drop - you’re not done yet.
...and yes, CGMs are lifesavers. I’ve seen people cry when they see the spike coming before it happens. That’s not tech - that’s peace.
...and no, you don’t need to be perfect. You just need to be aware.
...and yes, you’re not failing. The system is.
...and yes, I’m still crying.
...and yes, I’m still checking.
...and yes, I’m still here.
...and yes, you can too.
...and yes, I believe in you.
Josh Zubkoff
December 1, 2025 AT 21:56Okay, let’s be real - this whole post is just a 10,000-word ad for insulin pumps and CGMs. Who even has access to that? I’m guessing the author is a pharma rep in disguise. And don’t get me started on the ‘basal-bolus’ nonsense - if you’re on steroids for a week, you don’t need a PhD in endocrinology. Just eat less bread, walk after meals, and don’t be a zombie on the couch. And the ‘tapering trap’? That’s not a trap - that’s just bad follow-up care. Blame the system, not the patient. And why is every example a white American? What about the rest of us? This feels less like medicine and more like a Silicon Valley wellness fantasy. 🤡
fiona collins
December 3, 2025 AT 05:07Thank you for this. Clear, accurate, and compassionate. I’m a nurse in a rural clinic, and this is exactly what I wish every provider had read before sending patients home on steroids. The tapering advice alone could save lives. I’ve seen too many come back with lows because no one told them to reduce insulin. I’m sharing this with my team tomorrow. You’ve made a difference.
And yes - CGMs aren’t luxury. They’re a bridge. Even a borrowed one.
Grateful.
Rachel Villegas
December 4, 2025 AT 02:27This is the most practical, no-nonsense guide I’ve ever read on steroid hyperglycemia. I’ve been on prednisone twice now - once for lupus, once for a bad allergic reaction. The first time, I winged it and ended up in the ER. The second time, I followed this exactly. No drama. No panic. Just checks, adjustments, and communication with my endo. It’s not about perfection. It’s about awareness. And that’s what this post gives you. Thank you.
giselle kate
December 4, 2025 AT 02:54Let me guess - you’re one of those people who thinks diabetes is just a ‘lifestyle disease’ and steroids are the villain? Wake up. The real villain is the pharmaceutical industry pushing insulin as a profit engine. You’re scared of natural healing. You’re scared of fasting. You’re scared of the body’s innate ability to heal. This whole post is just fear-mongering wrapped in medical jargon. Steroids are natural - your body makes cortisol. Why are you afraid of a little extra? Just eat keto, stop sugar, and trust your body. Insulin is poison. I’ve seen people become dependent on it after steroids - it’s a trap. Don’t fall for it.
Emily Craig
December 5, 2025 AT 18:12So let me get this straight - you’re telling me I have to check my blood sugar 6 times a day, adjust insulin like a mad scientist, and then cut it again when I’m finally feeling better… all because some pill made my pancreas throw a tantrum? And you’re surprised people give up? Honey. I don’t need a spreadsheet. I need a nap. And maybe a hug. And a cookie. But definitely not more insulin. 😴🍪
Karen Willie
December 7, 2025 AT 00:19I’ve been managing steroid-induced hyperglycemia for my mom since she started on high-dose prednisone for her rheumatoid arthritis. This post is spot-on. We started with a CGM, adjusted insulin slowly, and kept a daily log. The biggest win? When we reduced her dose from 30mg to 20mg, we cut insulin by 15% - and she didn’t crash. She slept through the night for the first time in weeks. It’s not about being perfect. It’s about being consistent. And you’re not alone. We’re all learning as we go.
Thank you for writing this. It’s a lifeline.
Leisha Haynes
December 7, 2025 AT 03:13Y’all are overthinking this. You want to know the secret? Just take your insulin like you’re supposed to - not when you feel like it, not when you’re tired, not when your phone dies. And when the steroid tapers? Cut the insulin before you feel low. Not after. That’s it. No fancy apps. No 37% accuracy stats. Just do the thing. I’ve been on steroids twice. I didn’t cry. I didn’t panic. I just did the math. And I’m still here. You can too.
Also - stop blaming the system. The system doesn’t care. You do. So care.
And yes - I ate a croissant yesterday. And I took my insulin. And I’m fine.