TZD Heart Failure Risk Assessment Tool
How Risky Is Your TZD Medication?
This tool helps you understand your risk of heart failure complications from thiazolidinediones (TZDs) based on your health factors. TZDs can cause fluid retention that may worsen or trigger heart failure in at-risk individuals.
Risk Factors
Your Risk Assessment
When you’re managing type 2 diabetes, finding a medication that lowers blood sugar without causing low blood sugar episodes is a win. That’s why thiazolidinediones-like pioglitazone (Actos) and rosiglitazone (Avandia)-were once popular. They make your body more sensitive to insulin, helping it use glucose more efficiently. But there’s a hidden risk that many patients and even some doctors don’t fully understand: fluid retention that can lead to or worsen heart failure.
How Thiazolidinediones Work-and Why They Cause Fluid Retention
Thiazolidinediones (TZDs) activate a protein called PPAR-γ, found in fat, blood vessel, and kidney cells. This boosts insulin sensitivity, which is great for blood sugar control. But that same mechanism triggers changes in the kidneys that cause the body to hold onto sodium and water. It’s not just a minor side effect-it’s a measurable shift in fluid balance. Studies show TZDs can increase blood volume by 6-7% in healthy people. That extra fluid doesn’t just sit in your ankles; it can flood your lungs and strain your heart.
Up to 15% of people taking TZDs with insulin develop noticeable swelling in their legs or feet. Even when used alone, about 7% of users get peripheral edema. That number climbs even higher in older adults, women, and those already on diuretics or with kidney issues. The fluid doesn’t always go away with over-the-counter remedies. Loop diuretics like furosemide often don’t work well against TZD-induced retention because the problem isn’t just volume overload-it’s how the kidneys are reabsorbing sodium at a cellular level.
The Link Between Fluid Retention and Heart Failure
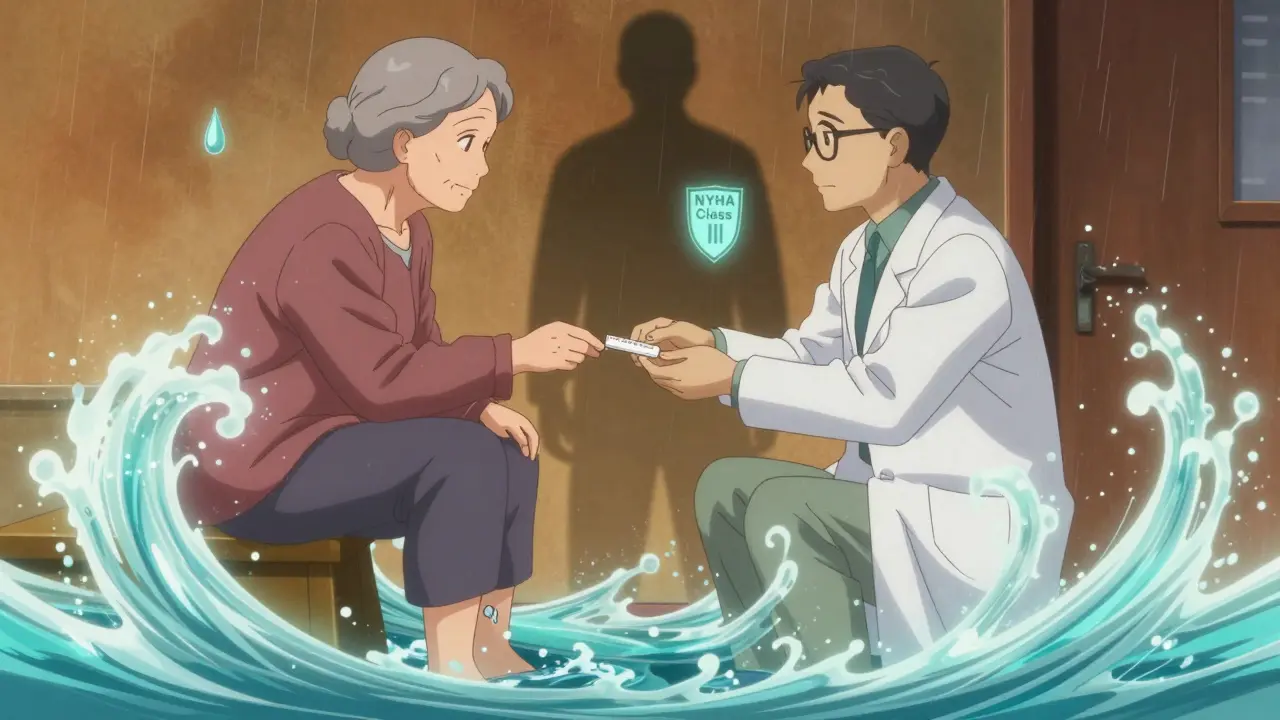
Here’s where it gets dangerous: if your heart is already weak, adding extra fluid can push it over the edge. The American Heart Association and American Diabetes Association agree: TZDs are not safe for people with moderate to severe heart failure (NYHA Class III or IV). But the bigger problem? Many patients who are taking them shouldn’t be.
A 2018 analysis of over 424,000 U.S. adults with diabetes found that 40.3% of those on TZDs already had signs of heart failure-either a diagnosis, an ejection fraction under 40%, or were taking loop diuretics. That means nearly half the people using these drugs had conditions that made them high-risk. And yet, they were still being prescribed.
In one study of 111 diabetic patients with existing heart failure, 17% developed new or worsening fluid retention within two years. Six of them showed signs of worsening heart function, like increased jugular vein pressure. Two developed pulmonary edema-fluid in the lungs-requiring hospitalization. These weren’t rare events. They happened in a group already considered high-risk.
Who Should Avoid Thiazolidinediones?
If you have any of these, you should not be on a TZD:
- Diagnosed heart failure, especially NYHA Class III or IV
- Current or recent history of pulmonary edema
- Severe kidney disease (eGFR below 30)
- Already taking insulin and showing signs of swelling
- History of fluid retention with other diabetes meds
Even if you don’t have heart failure yet, if you’re over 65, female, obese, or have coronary artery disease, your risk goes up. The Diabetes Collaborative Registry showed that TZD users were typically older (average age 69), with 62% having heart disease. That’s not a coincidence. These are the very people who should be avoiding these drugs.
What If You’re Already Taking a TZD?
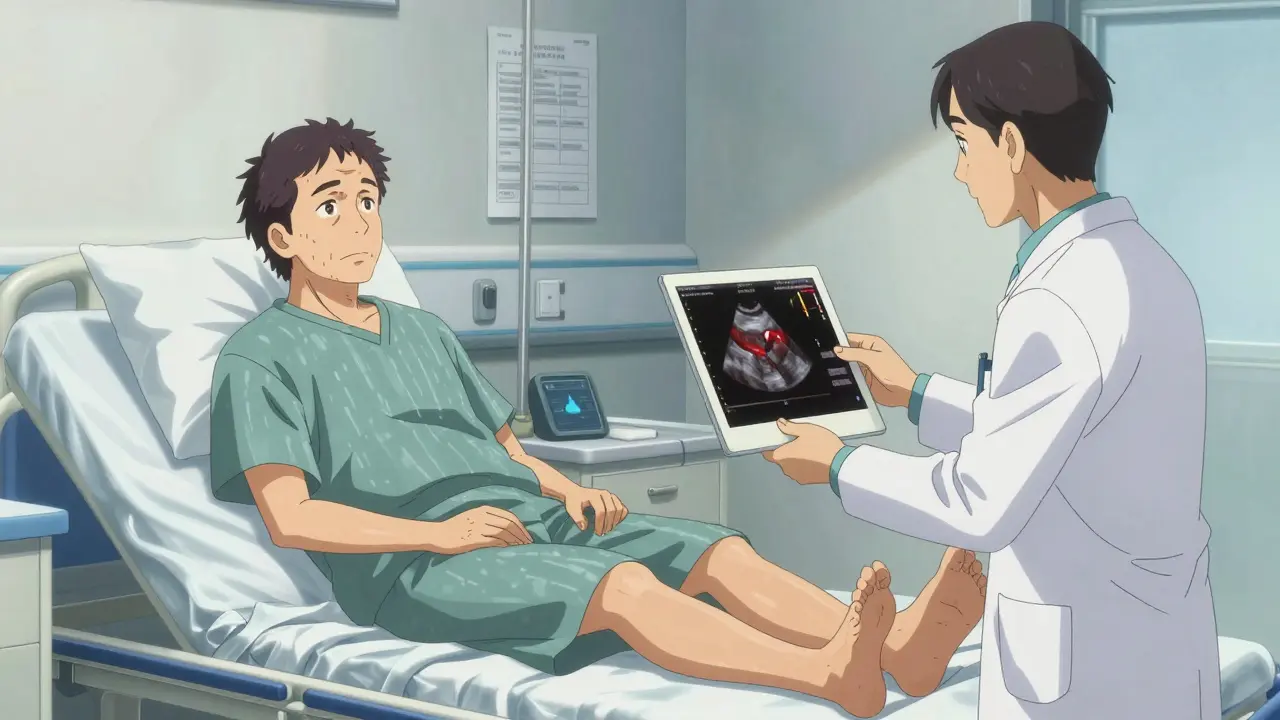
If you’re currently on pioglitazone or rosiglitazone and haven’t been screened for heart failure, talk to your doctor. Don’t wait for swelling to appear. Ask for:
- A recent echocardiogram to check your ejection fraction
- Review of your weight trends over the last 3-6 months
- Assessment of any leg swelling, shortness of breath during normal activity, or waking up gasping for air
If you’ve gained more than 5-10 pounds in a few weeks without changing diet or activity, that’s a red flag. So is needing to prop up with extra pillows to sleep. These aren’t normal aging changes-they’re signs your body is holding too much fluid.
Many patients assume their doctor is monitoring them closely. But studies show TZD use in heart failure patients is under-recognized in clinics. You may need to be your own advocate.
What Are the Alternatives?
There are plenty of other diabetes medications that don’t cause fluid retention:
- Metformin: First-line for most patients. No weight gain, no fluid retention.
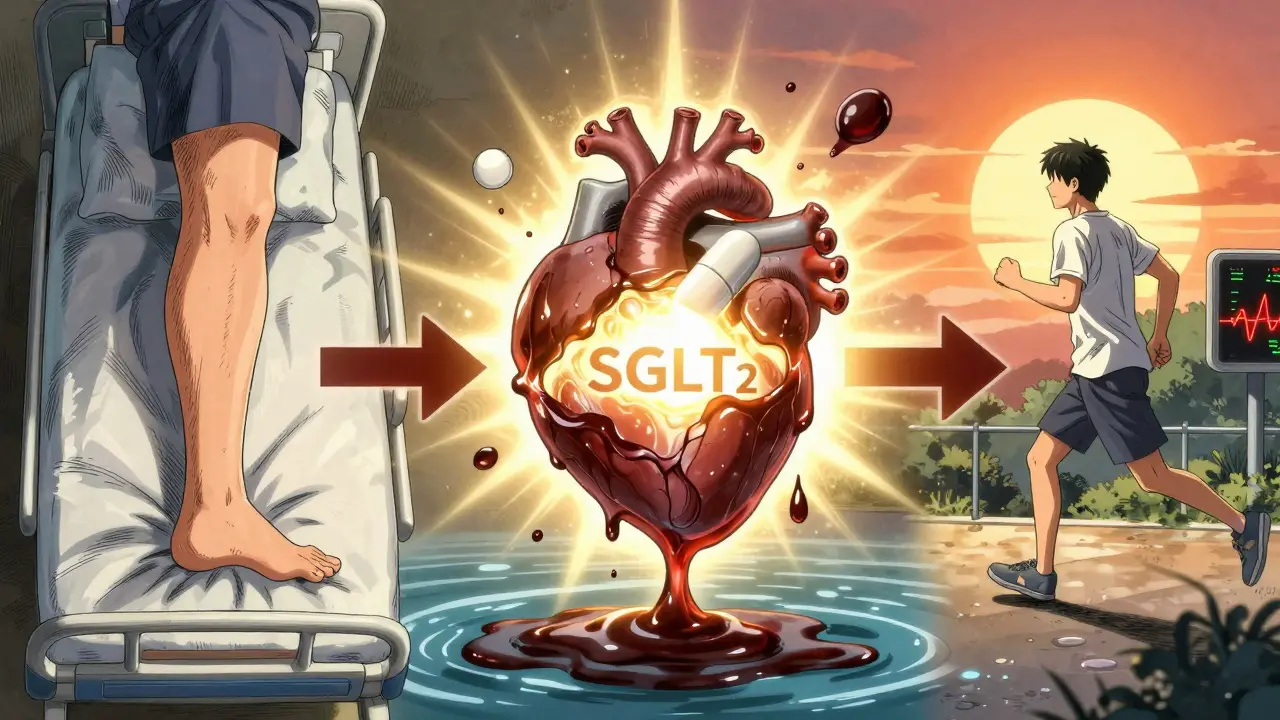
- SGLT2 inhibitors (like empagliflozin, dapagliflozin): Lower blood sugar, help the kidneys flush out extra salt and water, and actually reduce heart failure hospitalizations.
- GLP-1 receptor agonists (like semaglutide, liraglutide): Improve blood sugar, promote weight loss, and protect the heart.
These newer drugs don’t just avoid the risks of TZDs-they actively reduce cardiovascular events. In fact, SGLT2 inhibitors are now recommended as first-line for patients with diabetes and heart failure, regardless of their A1C level.
Why Are TZDs Still on the Market?
Despite the risks, TZDs haven’t disappeared. Pioglitazone is still sold under the brand Actos and costs around $300 for a 30-day supply. Rosiglitazone is available only through a restricted program due to past concerns about heart attacks, but it’s still an option in rare cases.
Why? Because for some people-especially those with severe insulin resistance who haven’t responded to anything else-TZDs work. They don’t cause hypoglycemia. They improve insulin sensitivity better than most other drugs. And in people without heart disease, they may even reduce plaque buildup in arteries.
But those benefits only matter if you’re not at risk for heart failure. And that’s the catch: many patients don’t know they’re at risk until it’s too late.
What Doctors Should Be Doing
Current guidelines from the American Diabetes Association say TZDs can be used cautiously in patients with mild heart failure (NYHA Class I-II), but only with close monitoring. That means:
- Check weight weekly for the first month
- Ask about swelling, shortness of breath, or fatigue
- Get a baseline echocardiogram before starting
- Stop the drug immediately if fluid retention develops
The American Association of Clinical Endocrinologists is even clearer: avoid TZDs entirely in patients with heart failure or at high risk. And with nearly half of current users already showing signs of heart problems, that advice needs to be taken seriously.
The truth is, we have better tools now. You don’t need to gamble with fluid retention when drugs like SGLT2 inhibitors not only lower blood sugar but also protect your heart.
Bottom Line
Thiazolidinediones can help control blood sugar-but at a cost. The fluid retention they cause isn’t just a nuisance. It’s a trigger for heart failure in vulnerable people. If you’re taking one of these drugs, ask yourself: Do I know my heart health status? Have I been checked for swelling or shortness of breath? Is there a safer option for me?
For most people with diabetes and heart disease, the answer is yes. The risks of TZDs outweigh the benefits. And if you’re still on one, it’s time to have a serious conversation with your doctor about switching.




Dikshita Mehta
December 18, 2025 AT 22:47Just wanted to say this post is one of the clearest summaries I’ve read on TZDs and heart failure risks. I’m a nurse in Mumbai and see this all the time - older patients on pioglitazone with unexplained weight gain, then suddenly admitted for pulmonary edema. No one connects the dots until it’s too late. Seriously, every diabetic patient should get a baseline echo before starting these drugs. It’s not optional anymore.
Kathryn Featherstone
December 19, 2025 AT 00:26This is so important. My mom was on Actos for years and didn’t realize her swelling wasn’t just ‘getting older.’ She gained 12 pounds in 6 weeks and thought it was her diet. Turned out her EF dropped to 38%. Thank you for writing this - I’m sharing it with every diabetic friend I have.
Chris Clark
December 20, 2025 AT 01:22Man I remember when Avandia was the hype drug. Everyone was like ‘oh wow it fixes insulin resistance!’ and then boom - lawsuits, black box warnings, and suddenly no one talks about it. But Actos? Still hanging around like a ghost. I got prescribed it last year and asked my doc why not an SGLT2i. He said ‘it’s cheaper.’ I said ‘but my heart isn’t.’ He shut up.
Nina Stacey
December 20, 2025 AT 10:19I think people forget that diabetes meds aren’t one size fits all and that fluid retention isn’t just puffy ankles it’s your lungs slowly drowning and you don’t even notice until you can’t sleep without three pillows and your socks leave imprints like you’re in a prison camp and yeah I know I sound dramatic but I’ve seen it happen to my aunt and now I’m scared to even take metformin because what if that’s next
Aadil Munshi
December 21, 2025 AT 22:46Let’s be real - TZDs are still around because Big Pharma doesn’t want you switching to cheaper generics. SGLT2 inhibitors? Patent protected. Glucophage? $4 at Walmart. Who profits when you stop Actos? Not the guy in the white coat. Also, did you know pioglitazone was originally developed as an anti-cancer drug? That’s why it’s so good at making fat cells behave - it’s literally reprogramming your body. But your heart? Not part of the plan.
Mark Able
December 22, 2025 AT 05:34Bro I’m on Actos and I’m 72 and my knees hurt and I’m tired but I’m not in heart failure so why are you telling me to quit? My doctor says I’m fine. You’re just scaring people. I’ve been on this for 8 years and I’m still walking. Don’t ruin my life because you read a study.
mark shortus
December 23, 2025 AT 00:20THIS IS A MASSIVE COVER-UP. I’ve been saying this for YEARS. TZDs are not just risky - they’re a slow-motion murder weapon disguised as a miracle drug. The FDA knew. The AMA knew. But they let it slide because doctors get kickbacks from pharma reps. I’ve got a cousin who died of pulmonary edema at 64 - prescribed Actos after his third heart scare. No one asked about his ejection fraction. No one. And now? His widow’s stuck with $800/month in medical bills. This isn’t medicine. It’s corporate manslaughter.
James Stearns
December 23, 2025 AT 12:20While I appreciate the clinical precision of this exposition, I must register my profound concern regarding the casual tone adopted throughout. The use of colloquialisms such as ‘flood your lungs’ and ‘red flag’ undermines the gravitas of a medical condition that, when unmanaged, results in mortality. One must approach such matters with the solemnity befitting the sanctity of human physiology. Furthermore, the omission of any reference to the PPAR-γ receptor’s role in adipogenesis is a glaring scholarly deficiency.
Danielle Stewart
December 23, 2025 AT 14:19Thank you for this. I’m a diabetes educator and I wish every patient got this info before starting TZDs. I’ve had patients cry because they didn’t know their swelling was dangerous. We need mandatory screening before prescribing. Not optional. Not ‘if you feel like it.’ Mandatory. And insurance should cover the echo - it’s cheaper than ICU.
Carolyn Benson
December 23, 2025 AT 14:56You all are missing the point. This isn’t about drugs. It’s about control. Who controls your body? The doctor? The FDA? The pharma execs in New Jersey? You think you’re choosing your meds? No. You’re being guided. The system wants you dependent. Fluid retention? It’s not a side effect - it’s a feature. Keeps you coming back. Keeps you on the treadmill. Wake up.
jessica .
December 25, 2025 AT 12:17THIS IS A DEEP STATE TACTIC. TZDs were never about diabetes. They were about population control. The fluid retention? That’s how they thin out the elderly. You think they care about your heart? They care about Medicare costs. That’s why they pushed SGLT2 inhibitors - they’re expensive. But Actos? Cheap. And if you die from it? Well… the system wins. Read the documents. The FDA emails. It’s all there.
Ryan van Leent
December 26, 2025 AT 21:01Why are we even talking about this? Just stop eating sugar. Problem solved. No drug needed. But nope gotta keep popping pills and blaming the medicine. I’ve been off sugar for 5 years. My A1C is 5.1. No meds. No swelling. Just discipline. You people need to take responsibility.
Chris porto
December 27, 2025 AT 23:19It’s funny how we treat medicine like a tool when it’s really a conversation between body and science. TZDs work - they really do - but they ask for something in return. Maybe the real question isn’t ‘should we stop them?’ but ‘how do we listen better to what our bodies are telling us?’ Swelling isn’t just water. It’s a whisper. And we’ve been screaming over it with prescriptions.