Polypharmacy Risk Checker
Check Your Medication Risk
Enter the medications you're currently taking to identify potential dangerous combinations and polypharmacy risks. This tool is designed for adults over 60, but can be used by anyone taking multiple medications.
Your Medication Risk Assessment
More than 1 in 3 adults over 60 are taking five or more prescription drugs. It’s not unusual. It’s not even rare. But it’s dangerous. Not because the medications themselves are bad - many are lifesavers. But when they’re stacked together without a clear plan, they can turn into a silent ticking bomb. Dizziness. Confusion. Falls. Hospital trips. Even death. And most of the time, it’s avoidable.
What Exactly Is Polypharmacy, and Why Should You Care?
Polypharmacy isn’t just taking a lot of pills. It’s taking five or more medications regularly - including prescriptions, over-the-counter drugs, and supplements - and not having a clear reason for each one. The problem isn’t the number. It’s the combinations.
Each extra pill you take increases your chance of a serious drug interaction by nearly 40%. That’s not a guess. That’s from a study of over 700 cancer patients. And it’s worse if you’re older. Your body doesn’t process drugs the same way it did at 30. Liver and kidney function slow down. Brain sensitivity goes up. A dose that was fine last year might now make you fall.
And here’s the kicker: many of these pills are prescribed to fix side effects from other pills. That’s called a prescribing cascade. You take a blood pressure med and get dizzy. Your doctor gives you a sedative to help you sleep. That makes you even more unsteady. Then you get a laxative because the sedative causes constipation. Now you’re on six meds just to manage the side effects of one. It’s a spiral.
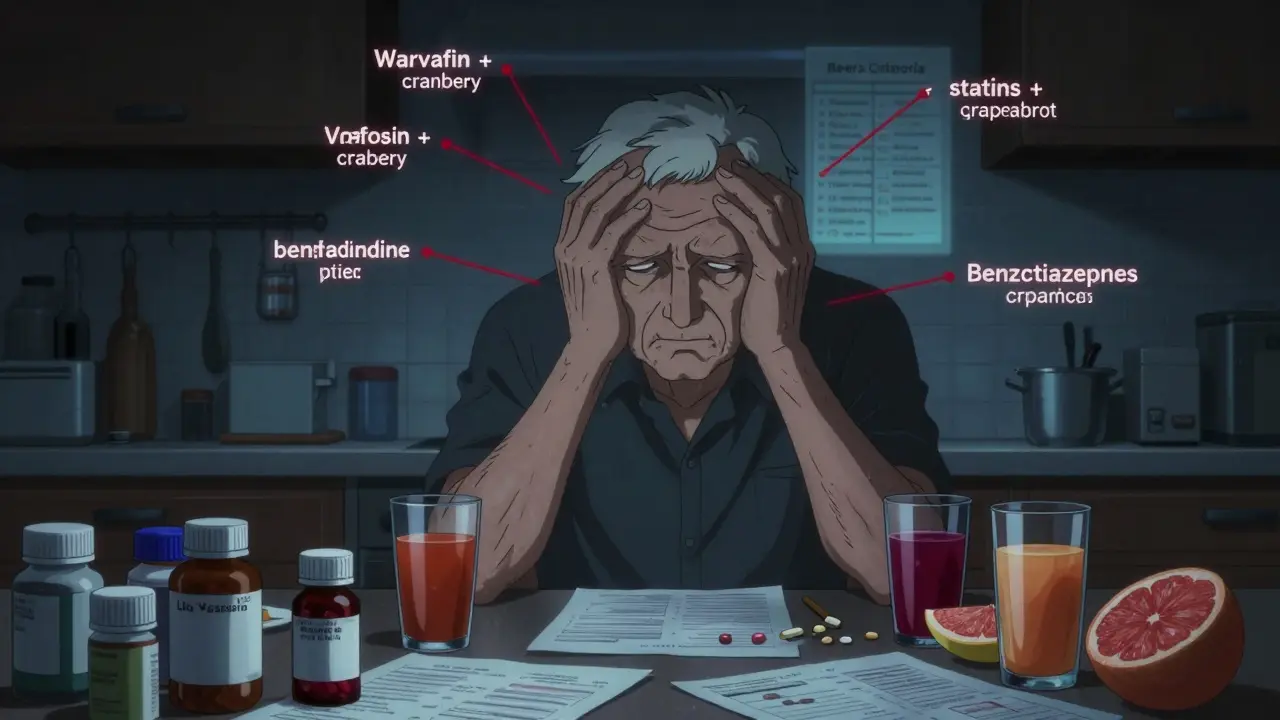
The Top 5 Dangerous Combinations You Need to Know
Not all drug mixes are equal. Some are deadly. Here are the five most common and dangerous ones you’ll see in clinics and ERs across Australia and the U.S.:
- Warfarin + cranberry juice - Warfarin thins your blood. Cranberry juice makes it thinner - way too thin. This combo can cause internal bleeding without warning. Even a glass a day can be risky.
- Statins + grapefruit juice - Statins like atorvastatin or simvastatin help lower cholesterol. Grapefruit juice blocks how your body breaks them down. That means too much drug builds up. Result? Muscle breakdown (rhabdomyolysis), kidney failure, and in rare cases, death.
- Blood pressure meds + decongestants (like pseudoephedrine) - Decongestants in cold meds raise blood pressure. If you’re already on meds to lower it, this can spike your BP to dangerous levels - especially if you have heart disease.
- Acetaminophen + oxycodone + prochlorperazine - This trio is often found in patients who end up in the ER. Acetaminophen and oxycodone are painkillers. Prochlorperazine treats nausea. But together, they cause extreme drowsiness, low breathing, and confusion. It’s a classic case of stacking sedatives.
- Benzodiazepines (like diazepam) + opioids (like oxycodone or morphine) - This combo is one of the most lethal. Both depress the central nervous system. Together, they can shut down breathing. The CDC lists this as a top cause of opioid-related deaths.
These aren’t hypotheticals. They’re real. A 72-year-old man in Sydney ended up in hospital after taking his blood pressure pill with a cold tablet he grabbed off the shelf. He didn’t know the label said “contains pseudoephedrine.” He didn’t think it mattered.
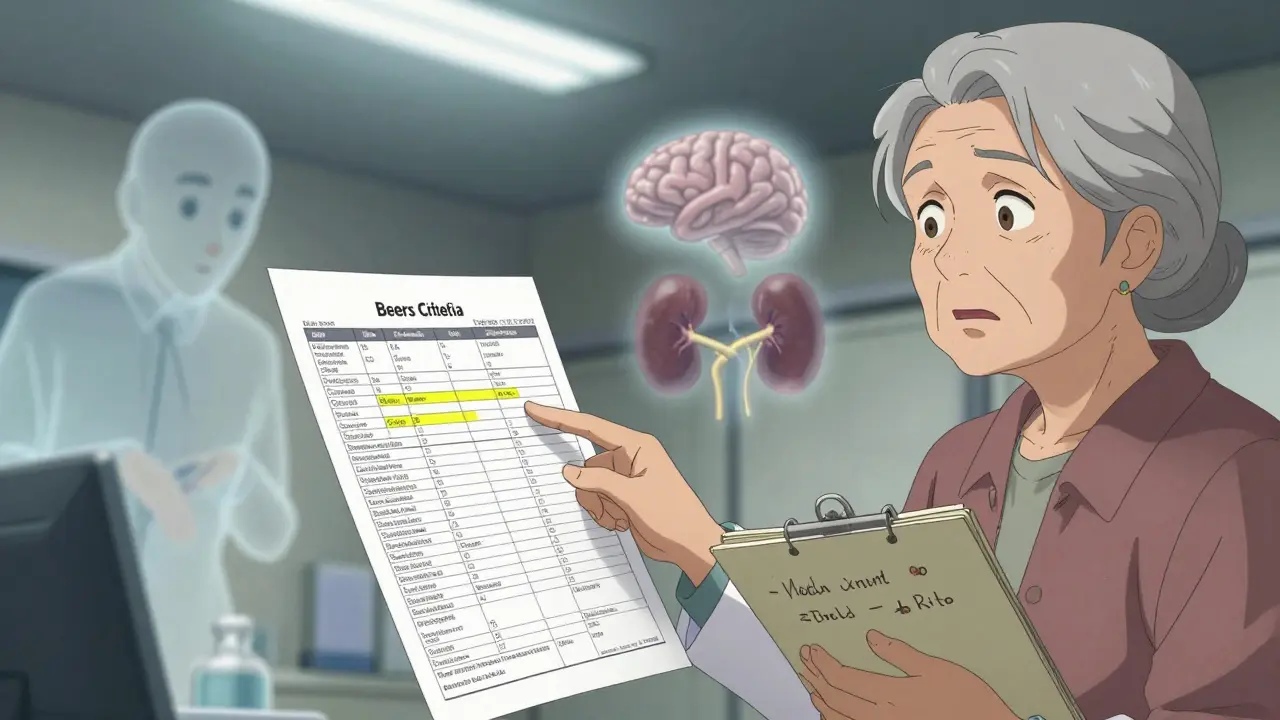
The Beers Criteria: Your Secret Weapon Against Bad Prescriptions
Doctors don’t always know which drugs are risky for older adults. That’s why the Beers Criteria exists. It’s a list - updated in 2019 - of medications that are often inappropriate for people over 65 because of their side effects.
Here’s what the Beers list flags:
- Anticholinergic drugs - like diphenhydramine (Benadryl), oxybutynin, and some antidepressants. These cause brain fog, memory loss, and constipation.
- Benzodiazepines - like lorazepam and alprazolam. They increase fall risk by up to 50%.
- α1-blockers - like doxazosin and terazosin. Used for prostate issues, but they cause sudden drops in blood pressure when standing.
- Nonsteroidal anti-inflammatories (NSAIDs) - like ibuprofen and naproxen. Can cause kidney damage and stomach bleeds, especially when mixed with blood thinners.
Just because a drug is on the Beers list doesn’t mean it’s always wrong. But it means you need to ask: Is this still necessary? Is there a safer alternative? Can we try lowering the dose?
Your Polypharmacy Risk Checklist: 7 Steps to Stay Safe
You don’t need a PhD to protect yourself. Just a notebook, a pharmacist, and the courage to ask questions. Here’s your practical checklist:
- Make a complete list - Write down every pill, patch, cream, vitamin, and herbal supplement you take. Include dosages and why you take them. Don’t leave anything out. Even the “harmless” ones like melatonin or turmeric.
- Bring it to every appointment - Don’t rely on memory. Don’t assume your doctor knows what’s on your list. Bring it in person. Or take a photo of the bottles.
- Ask: “Why am I taking this?” - If your doctor can’t give you a clear reason, question it. If it’s “just in case,” that’s not enough.
- Check for food interactions - Grapefruit juice, cranberry juice, alcohol, and even dairy can change how drugs work. Ask your pharmacist, not just your doctor.
- Look for prescribing cascades - Are you taking a new drug to fix a side effect of another? That’s a red flag. Ask: “Can we stop the first one and see what happens?”
- Use the ARMOR method - Assess your meds. Review them with a pharmacist. Minimize what’s not needed. Optimize the ones you keep. Reassess every 3-6 months.
- Know your emergency signs - If you feel suddenly dizzy, confused, weak, or have trouble breathing, stop taking everything except your most critical meds and call your doctor or go to the ER.
Who Should Be on Your Team?
You can’t do this alone. You need allies.
Your pharmacist is your best friend. They see your full prescription history. They know which drugs clash. Most pharmacies in Australia now offer free medication reviews. Use them.
Your GP should be your quarterback - the one person coordinating all your care. If you see multiple specialists, make sure they’re talking to each other. Ask your GP to run a “medication reconciliation” every six months.
Your family - if you live alone, get someone you trust to help you track your pills. Set alarms. Use a pill organizer. Take photos of your pill box each week.

What Happens When You Reduce Your Meds?
Some people think fewer pills means worse health. That’s not true. A 72-year-old cancer patient in Melbourne went from 12 medications down to 7 after a pharmacist-led review. Her energy improved. Her confusion cleared. She stopped falling.
One woman in Brisbane stopped her sleeping pill after her doctor suggested it. She was worried she’d never sleep again. Instead, she started walking every morning. Her sleep got better. Her anxiety dropped. Her blood pressure improved. She didn’t need the beta-blocker anymore.
Deprescribing isn’t about stopping meds because they’re “old.” It’s about removing what’s no longer helping - or what’s doing more harm than good.
The Bigger Picture: Why This Isn’t Just Your Problem
Polypharmacy isn’t just a personal risk. It’s a system failure. In Australia, over 27% of hospital admissions in seniors are linked to medications. That’s 1 in 4. And the cost? Over $37 billion a year in the U.S. alone - and rising fast.
Electronic alerts in hospitals flag dangerous combos - but doctors override them 96% of the time. Why? Too many alerts. Too many false alarms. The system is broken.
But you don’t have to wait for the system to fix itself. You can act now. You can ask the questions. You can bring the list. You can say, “I think this might be too much.”
Because your life isn’t a spreadsheet. It’s not a statistic. It’s your body. And you deserve to feel clear-headed, steady on your feet, and in control.
What is the safest way to reduce my medications?
Never stop a medication suddenly - especially blood pressure, antidepressants, or seizure drugs. Work with your doctor or pharmacist to create a slow, step-by-step plan. They’ll help you taper one drug at a time, monitor for withdrawal symptoms, and track how you feel. The goal is to reduce harm, not create new problems.
Can over-the-counter meds really be dangerous?
Absolutely. Many people think “natural” or “non-prescription” means safe. But drugs like diphenhydramine (in sleep aids and cold meds), ibuprofen, and even high-dose vitamin E can interact badly with prescription drugs. A single bottle of Benadryl can cause confusion, dry mouth, and falls in older adults - especially when mixed with heart or anxiety meds.
How often should I get my meds reviewed?
At least every 6 months - or anytime you start or stop a medication, go to the hospital, or notice new side effects like dizziness, memory lapses, or fatigue. Many pharmacies offer free medication reviews. Ask for one.
Is it normal to take 10+ medications as you get older?
It’s common - but not normal. Taking 10+ pills often means you’re treating side effects of other drugs, not just your conditions. That’s a sign your care needs a reset. The goal isn’t to take more - it’s to take only what’s truly necessary.
What if my doctor says I need all these meds?
Ask for evidence. Say: “Can you show me the research that says this drug still helps me right now?” or “What happens if I try stopping this for a few weeks?” A good doctor will welcome that question. If they get defensive, consider getting a second opinion - especially from a geriatrician or clinical pharmacist.
Are there apps or tools that can help me track my meds?
Yes. Apps like Medisafe, MyTherapy, or even your pharmacy’s app can remind you when to take pills and flag potential interactions. Some smart pill dispensers even alert family members if you miss a dose. But no app replaces a human review. Use them as helpers, not replacements for talking to your pharmacist.
Next Steps: What to Do Today
Don’t wait for a fall. Don’t wait for a hospital visit. Here’s what to do right now:
- Grab a pen and paper. Write down every single thing you take - including supplements and vitamins.
- Call your pharmacy. Ask for a free medication review. They’ll check for interactions you didn’t know about.
- Write down one question to ask your doctor: “Is there a pill here I can safely stop?”
- Share your list with a family member or friend. Make sure someone else knows what you’re taking.
Medications are tools. Not magic. And like any tool, they can hurt you if you don’t use them right. You’re not being difficult by asking questions. You’re being smart. And that’s the best protection you’ve got.




Lynsey Tyson
December 20, 2025 AT 16:04I’ve been helping my mom sort through her meds after she nearly fell last month. She was on 14 pills. Now she’s down to 7 after a pharmacist review. Her energy’s back, and she’s actually laughing again. No magic-just asking the right questions.
Jedidiah Massey
December 21, 2025 AT 09:27It’s not merely polypharmacy-it’s pharmacological entropy. The system lacks orthogonal optimization; each prescriber operates in a siloed, non-integrated cognitive space. The Beers Criteria are a crude heuristic, but even they’re underutilized due to institutional inertia. We need AI-driven pharmacokinetic modeling integrated into EHRs-not just another checklist.
Alana Koerts
December 21, 2025 AT 22:18Wow. Another fear-mongering article. People die from falling off ladders too. Should we ban stairs? You’re ignoring that most of these meds are life-saving. The real problem? Patients who don’t take them as prescribed. Stop blaming doctors.
Dikshita Mehta
December 22, 2025 AT 15:02As a pharmacist in Delhi, I see this daily. One man took 12 pills, including turmeric + warfarin. He bled internally. No one told him turmeric thins blood. Education matters. Pharmacists aren’t just pill counters-we’re safety nets. Ask for a med review. It’s free.
Chris Clark
December 24, 2025 AT 13:47My abuela took 11 pills. We sat down with her pharmacy. Turned out 4 were for side effects of other pills. One was for ‘anxiety’-but she was just lonely. We cut the meds, started daily walks with her grandkids. She’s happier. And no more dizziness. Sometimes the cure isn’t another pill.
Allison Pannabekcer
December 24, 2025 AT 15:15My dad’s on a bunch of meds after his stroke. I didn’t realize how many were just ‘because we’ve always given them.’ We did the ARMOR method. Cut two, lowered doses on three. He’s not ‘weaker’-he’s clearer. I wish more families knew this was possible. You don’t need to be a doctor to ask, ‘Is this still helping?’
It’s not about being anti-med. It’s about being pro-wellness.
Sarah McQuillan
December 26, 2025 AT 07:20Oh great, another ‘Americans are dumb’ article. In Australia they do this better? Please. Our doctors are trained. If you don’t understand your meds, maybe you shouldn’t be in charge of your own health. Stop blaming the system-take responsibility.
James Stearns
December 26, 2025 AT 20:53It is imperative to underscore, with the utmost gravity, that the confluence of polypharmacy and geriatric physiological decline constitutes a non-trivial public health exigency. The regulatory architecture of pharmaceutical prescribing remains woefully antiquated. One must invoke the Hippocratic Oath in its purest form: Primum non nocere. Yet, the medical-industrial complex persists in its profit-driven over-prescribing. This is not a personal failure-it is a systemic atrocity.
Alisa Silvia Bila
December 27, 2025 AT 00:18My grandma’s on one less pill now. She sleeps better. No drama. Just a conversation with her pharmacist. You don’t need a PhD to ask, ‘Can we try cutting this?’
Dominic Suyo
December 27, 2025 AT 13:00Let’s be brutally honest: this is what happens when you let geriatricians and pharmacists be heard. The real issue? The medical system treats seniors like walking pill dispensers. Doctors get paid for prescribing, not for deprescribing. It’s capitalism in a white coat. And you? You’re the collateral damage.
anthony funes gomez
December 28, 2025 AT 15:34It’s not the number of drugs-it’s the lack of integration. Pharmacokinetic synergy isn’t accounted for in clinical workflows. The Beers Criteria are a band-aid. What we need is a dynamic, real-time, AI-augmented polypharmacy risk engine-trained on longitudinal EHR data, with pharmacogenomic overlays-that auto-suggests deprescribing pathways. We’re still using paper lists in 2024. This is medieval.
Nicole Rutherford
December 29, 2025 AT 04:27Of course you’re going to have side effects if you take 10 pills. You’re not a lab rat. Why do you think you need all of them? Probably because your doctor doesn’t care enough to audit your regimen. And you let them. Weak.
Mark Able
December 29, 2025 AT 11:00Hey I just read this and I had to comment. My uncle took 14 pills. He didn’t even know what half of them were for. We called his pharmacist, they found 5 that were useless. He stopped them. Now he’s walking his dog every morning. I’m telling everyone I know. You need to do this.
Marsha Jentzsch
December 30, 2025 AT 07:32So now we’re supposed to trust pharmacists more than doctors? What’s next? Letting TikTok influencers prescribe beta-blockers? You’re encouraging people to stop life-saving meds because some article says so. This is dangerous. And irresponsible.
Edington Renwick
January 1, 2026 AT 06:47They’re all just going to die anyway. Why bother? You think cutting a few pills is going to save someone? It’s not a cure. It’s a delay. And the system? It’s broken. We’re all just waiting for the next fall, the next ER visit, the next obituary. Might as well keep taking the pills. At least they feel something.