
When you pick up a generic pill at the pharmacy, you’re not getting a cheaper version of a drug-you’re getting the same drug, scientifically proven to work just like the brand-name version. But how does the FDA make sure that’s true? The answer lies in a tightly controlled set of standards for generic drug approval that focus on three non-negotiable pillars: safety, quality, and strength.
What Makes a Generic Drug the Same as the Brand-Name Version?
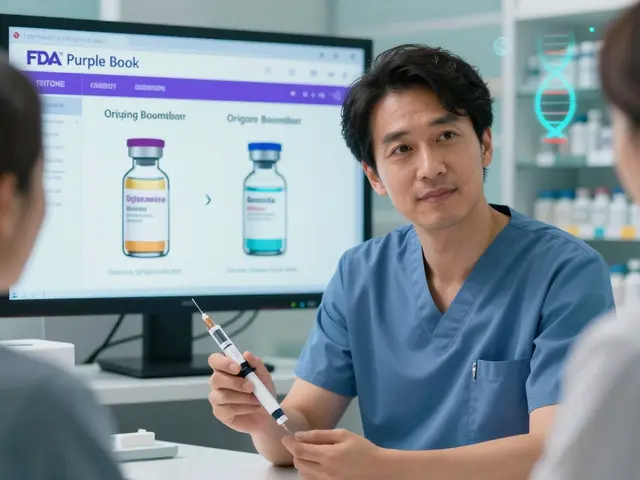
A generic drug isn’t just a copy. It has to contain the exact same active ingredient, in the same strength, and delivered the same way-whether it’s a pill, injection, or inhaler. The FDA calls this the Reference Listed Drug, or RLD. If the brand-name drug is 10 mg of lisinopril in a tablet taken by mouth, the generic must be identical in those details. No exceptions. This isn’t about marketing. It’s about biology.
But here’s where most people get confused: the inactive ingredients-like fillers, dyes, or coatings-can be different. That’s okay. What matters is that the active ingredient behaves the same way in your body. That’s where bioequivalence comes in.
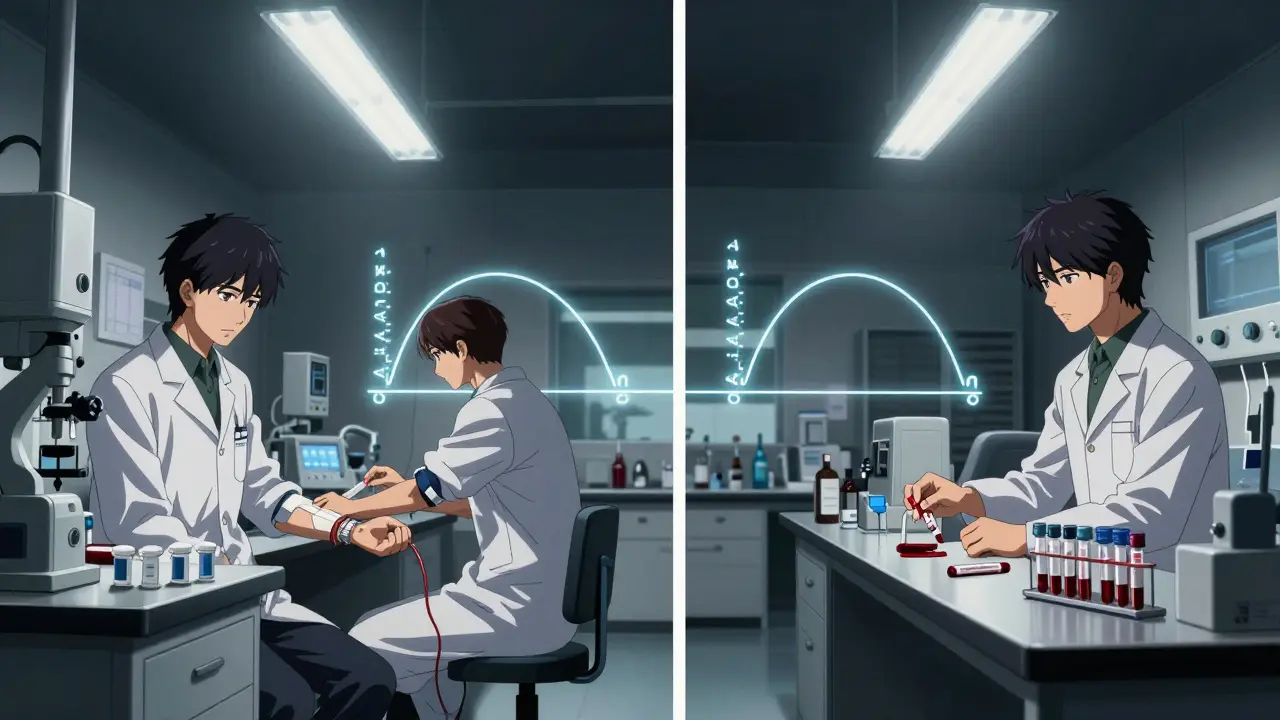
Bioequivalence: The Science Behind the Match
Bioequivalence is the core of generic approval. It’s not guesswork. It’s hard science. The FDA requires that a generic drug’s absorption rate in the bloodstream falls within 80% to 125% of the brand-name drug’s rate. This isn’t a broad range-it’s a narrow window designed to ensure no clinically meaningful difference in how the drug works.
For a standard tablet, this is tested in 24 to 36 healthy volunteers. They take the brand-name drug one day, then the generic another, with blood samples taken over hours to track how much of the drug enters the bloodstream and how fast. Two key measurements are used: Cmax (peak concentration) and AUC (total exposure over time). Both must stay within that 80%-125% range. If they don’t, the application is rejected.
For more complex drugs-like extended-release pills, inhalers, or topical creams-the rules get stricter. Take methylphenidate extended-release (Ritalin LA). The FDA doesn’t just look at total exposure. It breaks the absorption into time blocks: 0-3 hours, 3-7 hours, and 7-12 hours. The generic must match the brand’s release pattern in each segment. Otherwise, the drug might hit too fast or too slow, changing its effect.
Strength and Purity: No Room for Error
Strength isn’t just about how much active ingredient is in the pill. It’s about consistency across every batch. One tablet can’t be 9 mg, another 11 mg. The FDA requires manufacturers to prove their production process is stable and precise. This means testing every batch for identity, strength, purity, and stability under different conditions-heat, humidity, light.
Purity matters too. Contaminants-even tiny amounts of heavy metals or leftover solvents from manufacturing-are strictly limited. The FDA’s Current Good Manufacturing Practices (cGMP), outlined in 21 CFR Parts 210 and 211, set the bar. Facilities must be inspected before approval. In 2022, the FDA conducted about 1,200 pre-approval inspections. If a lab has inconsistent records, unclean equipment, or poor documentation, the application gets delayed until fixes are verified.
Quality Control: From Lab to Shelf
Manufacturing a generic isn’t like baking cookies. It’s a precision engineering task. The FDA uses its Question-Based Review (QbR) system to dig into every step. They ask: What are the Critical Quality Attributes (CQAs)? How do you control them? How do you know each batch is identical?
Successful applicants don’t just submit paperwork-they submit data. Three consecutive commercial-scale batches must show consistent results. Teva Pharmaceuticals’ regulatory team says new companies are often shocked by how deep the scrutiny goes. It’s not enough to say, “We followed the formula.” You have to prove, with data, that you can do it every time, in a controlled environment.
And it’s expensive. While a brand-name drug can cost $2.6 billion to develop, a generic averages $1.3 million. But for complex products-like auto-injectors or injectable suspensions-that number can jump to $25 million. That’s why only 3 out of 27 generic EpiPen applications were approved between 2015 and 2020. The device, not just the drug, had to meet exacting standards.
Narrow Therapeutic Index Drugs: Extra Caution
Some drugs have a razor-thin line between effective and dangerous. Warfarin, levothyroxine, and digoxin fall into this category. A 20% variation in blood levels could mean a clot or a stroke. For these, the FDA tightens the bioequivalence range to 90%-111%. For levothyroxine, the limit is even stricter: 95%-105%.
These aren’t theoretical rules. They’re based on decades of clinical data. A 2021 American Medical Association report reviewed 15 years of post-market data and found that 98.7% of generic drugs performed identically to brand-name versions in real-world use. But for narrow index drugs, the FDA doesn’t take chances. Each application gets extra scrutiny, additional testing, and sometimes, a longer review time.
Why Do So Many Generic Applications Get Rejected?
Despite the streamlined process, fewer than 10% of generic applications get approved on the first try. Why? Because the bar is high, and many applicants underestimate the complexity.
Common reasons for rejection: incomplete bioequivalence data, inconsistent manufacturing, unclear labeling, or failure to match the RLD’s dissolution profile. In 2021, Hetero Labs got a Complete Response Letter for its generic version of Jardiance because tablet hardness varied too much between batches. That’s a quality control failure-not a scientific one.
Complex generics-like inhalers, injectables, or topical gels-are especially tough. Only 58% of complex applications are approved within three review cycles, compared to 76% for simple pills. The FDA’s 2023 draft guidance aims to fix this by giving clearer expectations upfront.
The Real-World Impact
These standards aren’t just bureaucratic hoops. They save lives and money. In 2022, generics made up 90.3% of U.S. prescriptions but only 22.8% of drug spending. That’s $373 billion saved in one year. Without these strict rules, that savings wouldn’t be possible. Patients wouldn’t trust generics. Insurers wouldn’t cover them. Pharmacies wouldn’t stock them.
The FDA’s Office of Generic Drugs holds over 1,200 pre-submission meetings each year to help companies get it right before they apply. Nearly 85% of applicants say these meetings helped them avoid costly mistakes. That’s not luck. That’s good regulation.
What’s Next for Generic Drugs?
The pipeline is full. In 2023, the FDA approved 90 new generics, including the first version of Humira, a blockbuster drug for autoimmune diseases. The agency is targeting 50% of complex generics to be approved within two review cycles by 2027. That’s ambitious, but necessary. There are 127 complex brand-name drugs with no generic alternatives, worth $52 billion in annual sales.
Patent delays still slow things down. The FTC found that even after approval, generics wait an average of 2.4 years before hitting the market due to legal battles. But the science is solid. The standards work. And as long as manufacturers meet them, patients get the same medicine at a fraction of the cost.
So next time you see “generic” on your prescription label, know this: it’s not a compromise. It’s the result of one of the most rigorously tested systems in modern medicine.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires every generic drug to meet the same safety standards as the brand-name version. They must contain the same active ingredient, work the same way in the body, and have the same risks and benefits. Post-market surveillance over 15 years shows that 98.7% of generic drugs perform identically to their brand-name counterparts in real-world use.
Why do some generic drugs look different from the brand-name version?
The active ingredient is identical, but the inactive ingredients-like color, shape, or flavor-can differ. These don’t affect how the drug works. FDA rules require generics to look different to avoid confusion with brand-name products. This is purely for identification, not performance.
How long does it take to get a generic drug approved?
The average time from application to approval is about 32.7 months. Simple pills take around 28.5 months. Complex products like inhalers or injectables can take up to 47.2 months because they require more testing and manufacturing validation. The FDA aims to complete 95% of standard reviews within 10 months after submission.
Can a generic drug be less effective than the brand-name version?
No. If a generic is approved by the FDA, it must be bioequivalent to the brand-name drug. That means it delivers the same amount of active ingredient into your bloodstream at the same rate. Studies show no meaningful difference in effectiveness or safety. If a patient feels a difference, it’s likely due to psychological factors or changes in inactive ingredients-not the active drug.
What happens if a generic drug fails inspection?
If a manufacturing facility fails an FDA inspection, the application is put on hold until the issues are fixed. The company must submit a detailed corrective action plan, and the FDA will re-inspect. If problems are serious or repeated, the application can be denied. In 2021, over 15% of inspections found major cGMP violations, leading to delays or rejections.
Generic drugs are one of the most successful public health innovations of the last 40 years. They’re not second-rate-they’re science-backed, cost-effective, and rigorously tested. The system isn’t perfect, but the standards for safety, quality, and strength are as strict as they’ve ever been.




Donny Airlangga
January 8, 2026 AT 04:45I used to be skeptical about generics until my dad needed heart meds. He was paying $400 a month for the brand, then switched to generic-same script, same results, $15 a month. No side effects, no weird feelings. Just saved his life and our bank account.
Molly Silvernale
January 9, 2026 AT 00:48It’s not just science-it’s poetry, really. The way a molecule, identical in every measurable way, dances the same jig in your bloodstream whether it’s wrapped in a fancy logo or a plain white tablet… it’s almost romantic. The FDA? The silent poet of pharmacology, ensuring that biology doesn’t care about branding. And yet-we still pay for the label.
Aubrey Mallory
January 10, 2026 AT 11:24If you’re still doubting generics, you’re either rich enough not to care or you’ve been fed misinformation by Big Pharma’s marketing machine. The data is overwhelming. The science is ironclad. Stop letting corporate branding fool you into overpaying for the same damn pill.
christy lianto
January 10, 2026 AT 18:12My niece has epilepsy and takes levothyroxine. We switched generics twice-both times, the FDA-approved ones-and her seizures didn’t change. One time, the pill looked different-brighter color, smaller-so she panicked. We had to sit her down and explain: ‘It’s the same medicine, honey. Just a new wrapper.’ She cried. Then took it. That’s the real story-not the science, but the fear people carry. We need more education, not just regulation.
swati Thounaojam
January 11, 2026 AT 17:06Manish Kumar
January 12, 2026 AT 06:31You know, in the grand metaphysical scheme of things, the pill is just a vessel-a temporary container for molecular intent. The brand name? That’s the ego of capitalism. The generic? The soul of medicine, stripped bare of logos and shareholder expectations. When you swallow a generic, you’re not taking a drug-you’re rejecting the myth that value is tied to packaging. The body doesn’t read labels. It only knows chemistry. And chemistry? It’s the only truth we have.
Dave Old-Wolf
January 12, 2026 AT 18:58So if the generic has to match the brand’s absorption rate exactly, why do some people say they feel different on it? Like, I know someone who swears the generic for their anxiety meds made them feel ‘numb’-but the science says it’s the same. What’s going on there?
Prakash Sharma
January 13, 2026 AT 02:29India makes 60% of the world’s generics. And you Americans still act like they’re sketchy? We’ve been doing this right for decades. Your FDA checks our labs. We pass. You buy. You live. Stop acting like we’re selling fake medicine. We’re saving your lives-and you still treat us like second-class suppliers?
Kristina Felixita
January 14, 2026 AT 12:36Just had to share-my mom switched to generic insulin last year. She was terrified. We watched YouTube videos together about how it’s tested. Now she calls it ‘her little white hero.’ She even made a little sticker for her pillbox that says ‘FDA Approved & Loved.’ 😊 I cried. This stuff matters. Real people. Real savings. Real trust.
Joanna Brancewicz
January 15, 2026 AT 21:53Bioequivalence thresholds are non-negotiable. Cmax and AUC must converge within 80–125%. Dissolution profiles must mirror RLD. cGMP compliance is baseline, not aspiration. If you’re not meeting these, you’re not a generic-you’re a liability.
Evan Smith
January 16, 2026 AT 17:33So let me get this straight-you’re telling me I can pay $15 for the same drug that costs $400… and the FDA made sure it’s not a scam? I feel like I’ve been lied to my whole life. Who’s the real villain here? The generic makers? Or the pharmaceutical CEOs sipping champagne on their yachts?
Lois Li
January 17, 2026 AT 07:23I work in pharmacy and see this every day. People panic when the pill looks different. We explain the science. We show them the FDA paperwork. But it’s the quiet ones-the elderly, the anxious, the uninsured-who need the most reassurance. It’s not just about chemistry. It’s about dignity. They deserve to feel safe, even if the pill’s color changed.
Ken Porter
January 17, 2026 AT 21:05Generic drugs? Yeah, sure. Until someone dies because their ‘equivalent’ didn’t work. Then you’ll see how fast the lawyers come out. This whole system is a gamble with human lives. And we’re supposed to cheer?
Annette Robinson
January 17, 2026 AT 21:18I’ve worked with generic manufacturers for over 15 years. The level of detail required-batch records, dissolution curves, stability testing-it’s insane. These aren’t corner stores making pills. They’re high-tech labs with clean rooms and chemists working 12-hour shifts. The cost isn’t low because it’s cheap. It’s low because the patent expired. The work? Still world-class.
Luke Crump
January 19, 2026 AT 15:46Oh, so now the FDA is the hero? The same agency that approved OxyContin? The same one that let Purdue Pharma laugh all the way to the bank while thousands died? You think they care about your ‘science-backed’ generic? They care about paperwork. And lawsuits. And PR. Don’t mistake bureaucracy for benevolence.