
When a patient walks into the pharmacy with a prescription for a biologic drug like Neulasta or Humira, they’re not just getting a pill-they’re getting a complex therapy that can cost thousands of dollars per month. That’s where pharmacists step in-not just to fill the script, but to guide the patient through one of the biggest shifts in modern medicine: the move from originator biologics to biosimilars.
What Makes Biosimilars Different from Generics?
People often assume biosimilars are just like generic drugs. They’re not. Generics are exact chemical copies of small-molecule drugs like atorvastatin or metformin. Biosimilars, on the other hand, are made from living cells-yeast, bacteria, or mammalian cells-and are highly similar to their reference biologic, but not identical. Even tiny differences in how they’re manufactured can affect structure, which is why the FDA requires extensive testing to prove they’re safe and effective. The FDA’s approval process for biosimilars is stricter than for generics. While generics only need to show bioequivalence, biosimilars must prove no clinically meaningful differences in safety, purity, or potency. That’s why a biosimilar for insulin or a monoclonal antibody isn’t just a cheaper version-it’s a scientifically validated alternative backed by real-world data.Interchangeable vs. Non-Interchangeable: What Pharmacists Need to Know
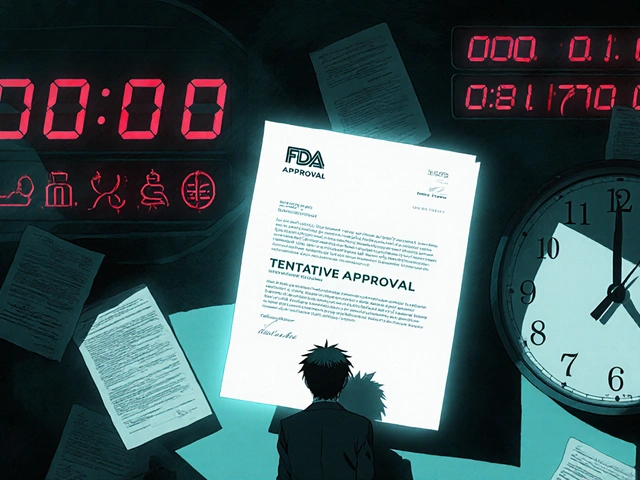
Not all biosimilars are created equal when it comes to substitution. The FDA has a special designation: interchangeable. An interchangeable biosimilar has met additional requirements, meaning a pharmacist can substitute it for the reference product without needing the prescriber’s approval-just like generics. As of late 2023, only a handful of biosimilars have received this status. For example, the pegfilgrastim biosimilar (a Neulasta alternative) became interchangeable in 2022. But most biosimilars on the market today are non-interchangeable. That means the prescriber must explicitly allow substitution, or the pharmacist must get permission before switching. This distinction matters. If a pharmacist substitutes a non-interchangeable biosimilar without consent, they could be breaking state law. Each state has its own rules. Some require the prescriber to sign off. Others let pharmacists switch automatically if the patient agrees. Pharmacists must know their state’s laws cold.Why Pharmacists Are the Key to Biosimilar Adoption
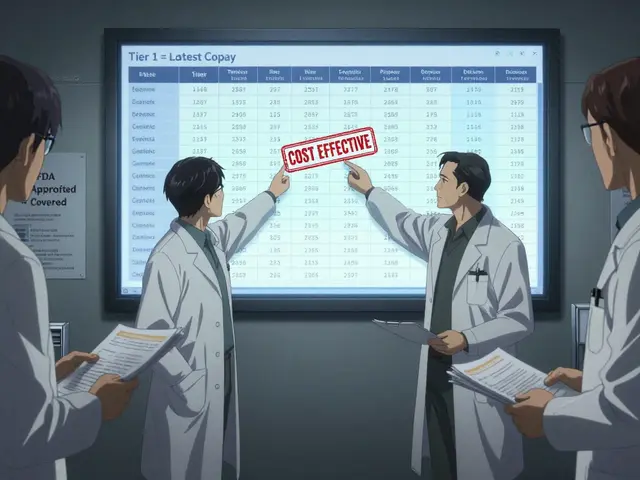
Biologics make up only 2% of prescriptions in the U.S., but they account for nearly half of all prescription drug spending. That’s a massive financial burden on patients and the system. Biosimilars can cut those costs by 15% to 35%-sometimes more. But cost alone doesn’t drive adoption. Patients and doctors are hesitant. Many think switching to a biosimilar means lower quality. Some believe biosimilars are untested. Others fear switching will cause side effects. That’s where pharmacists come in. Research from the American Society of Clinical Oncology shows that when pharmacists lead education efforts, biosimilar adoption jumps fast. At the US Oncology Network, after pharmacists took over substitution decisions and trained providers, biosimilar use for pegfilgrastim went from almost zero to over 80% in under a year. Pharmacists don’t just hand out pills. They explain the science. They answer questions. They document the switch. And they track outcomes.
How to Counsel Patients About Biosimilars
Patient counseling isn’t optional-it’s essential. A 2022 study found that patients are 21% more likely to stop taking their medication if the pill looks different after a switch. That’s why clear communication matters. Here’s what works:- Start with trust: "The FDA requires biosimilars to work just like the original drug. No meaningful differences in safety or effectiveness."
- Use analogies: "Think of it like two different brands of aspirin. They’re not made the same way, but they both relieve pain the same way."
- Address fears: "Switching between the original and biosimilar has been studied in thousands of patients. No increased risk of side effects."
- Explain traceability: "You’ll get a card with the batch number. If something happens, we can track exactly which version you took."
- Follow up: "Let’s check in next month. How are you feeling? Any new symptoms?"
Pharmacists vs. Doctors: Who Leads the Change?
Doctors often don’t know the latest biosimilar data. A 2022 study found that 79% of pharmacists had received continuing education on biosimilars, compared to just 43% of physicians. Pharmacists are more likely to recommend biosimilars-87% versus 62%. That gap creates tension. Some prescribers resist substitution. One doctor on Student Doctor Network complained that a pharmacist switched his patient’s Humira to a biosimilar without asking, and he got angry. The patient ended up discontinuing treatment. The solution? Collaboration. The US Oncology Network solved this by requiring all providers to complete mandatory biosimilar training and sign an acknowledgment form. Once doctors understood the process, interruptions dropped. No more last-minute calls asking, "Can I switch this?" Pharmacists aren’t replacing doctors. They’re supporting them. By handling substitution, pharmacists free up doctors to focus on patient care-not paperwork.
Real-World Barriers and How to Overcome Them
Even with strong science and good intent, barriers remain:- State laws vary: 48 states have biosimilar substitution laws, but rules differ. Some require patient consent. Others require prescriber approval. Know your state’s exact requirements.
- Rebate traps: Some pharmacy benefit managers (PBMs) still favor originator biologics because of rebates. Pharmacists should push back and advocate for formulary changes that prioritize cost-effective options.
- Billing confusion: 79% of pharmacists said they need more training on billing and reimbursement. Mixing up codes for reference products and biosimilars can lead to denied claims.
- Traceability gaps: If a patient has a reaction, the pharmacy must be able to report the exact batch number. That’s why documenting the product name and lot number in the EHR isn’t optional-it’s critical for safety.
What Pharmacists Should Do Today
You don’t need to wait for perfect conditions to make a difference. Here’s how to start now:- Learn your state’s substitution law. Check your state pharmacy board’s website. Know when you can substitute and what documentation is required.
- Identify which biosimilars in your inventory are interchangeable. Use the FDA’s Purple Book database. It’s free and updated weekly.
- Create a patient handout. Simple, one-page info sheets explaining biosimilars in plain language. Include the FDA’s "9 Things to Know" key points.
- Partner with prescribers. Offer to give a 10-minute lunch-and-learn to your local oncology or rheumatology clinics. Bring data. Show them the adoption numbers.
- Track your impact. Count how many biosimilar switches you make each month. Share that data with your pharmacy manager. Prove the value.
Why This Matters Beyond the Pharmacy Counter
Biosimilars aren’t just about saving money. They’re about access. Many patients skip biologic doses because they can’t afford them. With biosimilars, more people can get the treatment they need. Pharmacists are uniquely positioned to bridge the gap between science and patient care. We’re not just dispensers. We’re educators, advocates, and safety nets. The future of biologic therapy won’t be decided in boardrooms or by manufacturers. It will be decided in pharmacies, one conversation at a time.Can pharmacists substitute biosimilars without a doctor’s approval?
Only if the biosimilar has been designated as "interchangeable" by the FDA AND your state law allows automatic substitution. Most biosimilars are not interchangeable yet, so pharmacists usually need prescriber permission. Always check your state’s specific rules.
Are biosimilars as safe as the original biologic drugs?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the reference product. Thousands of patients have used biosimilars in the U.S. and Europe for over a decade with no increased risk of side effects. Switching between the original and biosimilar has been studied and found to be safe.
Why do some patients stop taking biosimilars after switching?
The most common reason is that the pill or injection looks different-different color, size, or packaging. Studies show patients are 21% more likely to discontinue use when they notice a change. Clear counseling about why the change happened and reassurance that it’s safe can prevent this.
Do pharmacists need special training to handle biosimilars?
Yes. Unlike generics, biosimilars require understanding of complex manufacturing, regulatory pathways, state substitution laws, and pharmacovigilance. Pharmacists should complete continuing education on biosimilars, especially on interchangeability, billing codes, and patient communication. Many pharmacy boards offer free or low-cost courses.
What should pharmacists document when substituting a biosimilar?
Pharmacists must record the name of the product dispensed (including the brand and generic name), the lot or batch number, and the date of substitution. This is critical for traceability in case of adverse events. The documentation should be in the patient’s electronic health record and shared with the prescriber if required by state law.
Are biosimilars cheaper than the original biologics?
Yes, typically by 15% to 35%, and sometimes more. However, rebate deals between drug manufacturers and pharmacy benefit managers can sometimes make the original product appear cheaper. Pharmacists should work with payers to ensure patients get the most cost-effective option, not just the one with the highest rebate.


Lance Nickie
January 14, 2026 AT 04:14biosimilars r just generic but with more steps and higher price tags. why not just cut the middleman?
Milla Masliy
January 15, 2026 AT 16:44I’ve seen this play out in my clinic-patients panic when the vial looks different, even if it’s the same drug. One woman cried because her Humira pen was blue instead of purple. We handed her a printed FDA comparison sheet and a cup of coffee. She stayed on it for 18 months. Communication matters more than you think.
Damario Brown
January 16, 2026 AT 16:08let me break this down real simple: pharmacists are getting paid to play doctor now. who authorized this? the FDA? no. the AMA? nah. but suddenly we’re supposed to trust some guy in a white coat to swap my biologic without my oncologist’s say-so? that’s not healthcare, that’s a liability waiting to happen. and don’t get me started on how many of these ‘interchangeable’ labels are just corporate marketing with a FDA stamp.
also, batch numbers? yeah right. i’ve seen pharmacies forget to log the damn thing. if i have an anaphylactic reaction, who’s liable? the pharmacist? the manufacturer? the PBM that pushed the cheaper version? nobody. that’s who.
John Pope
January 17, 2026 AT 23:50It’s not about substitution-it’s about sovereignty. The patient’s right to know what’s entering their body shouldn’t be outsourced to a pharmacist’s interpretation of state law. This isn’t switching from Tylenol to Advil. This is monoclonal antibodies-proteins folded by living cells, with post-translational modifications that can alter immunogenicity. We’re not talking about aspirin. We’re talking about biological systems that can trigger autoimmunity if the glycosylation profile shifts by 0.3%.
And yet, we’re told to trust a 12-minute continuing ed module and a PDF from the Purple Book? That’s not science. That’s capitalism dressed in scrubs. The real tragedy? The patients who benefit the most-low-income, chronically ill, uninsured-are the ones least equipped to question the swap. They’re just grateful it’s cheaper.
And don’t even get me started on the rebate traps. PBMs are playing 4D chess with our health system. Biosimilars aren’t saving money-they’re just shifting where the money flows. From pharma to PBM to pharmacy. Not to the patient. Not to the provider. To the middlemen.
Clay .Haeber
January 19, 2026 AT 02:29Oh wow, a pharmacist just became the new gatekeeper of biologic therapy? Next they’ll be writing prescriptions, doing MRIs, and diagnosing cancer over Zoom. Can’t wait for the TikTok trend: "Biosimilar Swap Stories with Nurse Jane". Meanwhile, the actual doctors who spent 12 years training are getting ghosted because someone in the back room found a 17% discount code.
And let’s be real-no one cares about the Purple Book except the 3 people who still use it. The rest of us just want our insulin to not cost a mortgage payment. If a biosimilar works, use it. If it doesn’t, switch back. Done. No 10-minute lunch-and-learns needed. Just let patients choose. Not the pharmacist. Not the PBM. THEM.
Priyanka Kumari
January 20, 2026 AT 04:00In India, we’ve been using biosimilars for over a decade-especially for TNF inhibitors in rheumatoid arthritis. The cost difference is life-changing. One patient told me, "I used to skip doses to make it last longer. Now I take it every week like clockwork."
But the real magic? When the pharmacist sits down with the patient, speaks in their language, and shows them the FDA data in simple terms. No jargon. No pressure. Just honesty. That’s what builds trust-not state laws or rebate charts.
Also, the batch number thing? Crucial. In our clinic, we print a small label with lot number and date and tape it to the patient’s medication diary. They love it. Feels like they’re part of the process, not just a number in a system.
Avneet Singh
January 21, 2026 AT 23:24Pharmacists are being handed undue authority under the guise of "cost containment." This is regulatory capture disguised as patient care. The FDA’s "no clinically meaningful difference" standard is a legal loophole, not a scientific guarantee. Biosimilars are not identical. They are *similar enough to pass regulatory tests*. There’s a difference.
And let’s not pretend the 80% adoption rate at US Oncology is some triumph. It’s coercion wrapped in data. Providers were trained into compliance. Patients were not given true informed consent. This isn’t innovation-it’s institutionalized pressure.
Adam Vella
January 23, 2026 AT 19:54While the intent behind promoting biosimilar adoption is commendable, the structural and epistemological assumptions underpinning this narrative are deeply flawed. The assumption that pharmacists, by virtue of their dispensing role, are epistemologically equipped to adjudicate clinical substitution decisions ignores the distributed nature of therapeutic expertise. Clinical judgment is not reducible to regulatory compliance or cost-benefit analysis.
Furthermore, the normalization of substitution without prescriber consent, even under "interchangeable" designation, constitutes a form of procedural overreach. The prescriber-patient relationship is not a transactional exchange; it is a fiduciary bond. To displace the prescriber’s authority-even partially-is to erode the foundations of medical trust.
It is not the pharmacist’s role to be the de facto gatekeeper of biologic therapy. That role belongs to the clinician who understands the patient’s comorbidities, immunological history, and psychosocial context-not the one who knows how to read the Purple Book.
Nelly Oruko
January 25, 2026 AT 02:56the whole thing feels like a bandaid on a broken system. we’re pushing biosimilars because we can’t fix drug pricing, not because we believe in better care.
but honestly? if it gets someone their medicine? i’m for it. just make sure they know what they’re getting. no jargon. no pressure. just facts.
vishnu priyanka
January 26, 2026 AT 10:16in my village back home, people use biosimilars because they can’t afford the original. no one’s crying about glycosylation profiles. they’re just glad they can breathe. maybe the real lesson here isn’t about FDA rules-it’s about how rich countries overcomplicate access to medicine.
Alan Lin
January 27, 2026 AT 13:03Let me be clear: this is not about cost. This is about accountability. When a patient is switched without informed consent, and then experiences a flare or an infusion reaction, who is held responsible? The pharmacist? The manufacturer? The PBM? The state board? The answer is nobody-because the system is designed to diffuse blame.
And yet, pharmacists are being asked to carry the burden of a broken system. You can’t fix $100,000-a-year drug pricing with a one-page handout and a state law that varies by county. What’s needed is federal reform-transparency in rebates, elimination of anti-competitive contracts, and mandatory prescriber-patient dialogue before substitution.
Pharmacists are heroes. But they shouldn’t be the last line of defense against a predatory system. That’s on Congress. On the FDA. On the manufacturers. Not on the pharmacist who’s already working 12-hour shifts.
Pankaj Singh
January 28, 2026 AT 12:29the 80% adoption stat is a lie. it’s based on patients who didn’t quit. not on outcomes. if someone’s disease worsens after switching, they don’t always report it. and if they do? the PBM suppresses the data. biosimilars are a corporate experiment with real human bodies. and pharmacists are the lab techs.
Gregory Parschauer
January 29, 2026 AT 22:05Oh, so now pharmacists are the new moral arbiters of biologic therapy? Let me guess-next they’ll be deciding who gets a liver transplant based on their "lifestyle score." This isn’t healthcare reform, it’s bureaucratic authoritarianism wrapped in a white coat. You think patients don’t notice when their $10,000-per-month drug suddenly becomes "just a biosimilar"? They feel it. They feel disrespected. They feel like their life is a cost-center.
And don’t give me that "FDA-approved" nonsense. The FDA doesn’t approve safety. It approves *statistical non-inferiority*. There’s a difference. A difference measured in IgG4 antibodies, glycosylation patterns, and immunogenicity risks that are only detectable after months of exposure. But sure, let’s trust a pharmacist who did a 45-minute webinar on biosimilars to make that call.
And the "interchangeable" designation? A marketing ploy. The same companies that made the originator biologic also made the biosimilar. Same factory. Same patents. Same profits. Just a different label. You call that competition? I call it a shell game.
And don’t even get me started on the rebate traps. The system is rigged. The PBM gets a kickback from the originator, so they push the expensive version-even if the biosimilar is cheaper. And now we’re blaming pharmacists for not fighting back? No. We’re blaming the entire pharmaceutical-industrial complex. And until we dismantle that, no amount of patient handouts or Purple Book training will fix what’s broken.
Patients aren’t dumb. They know when they’re being used. And if you think they’ll thank you for swapping their Humira for a cheaper version without asking, you’re living in a fantasy. They’ll just stop taking it. And then you’ll blame them for non-adherence. Classic.