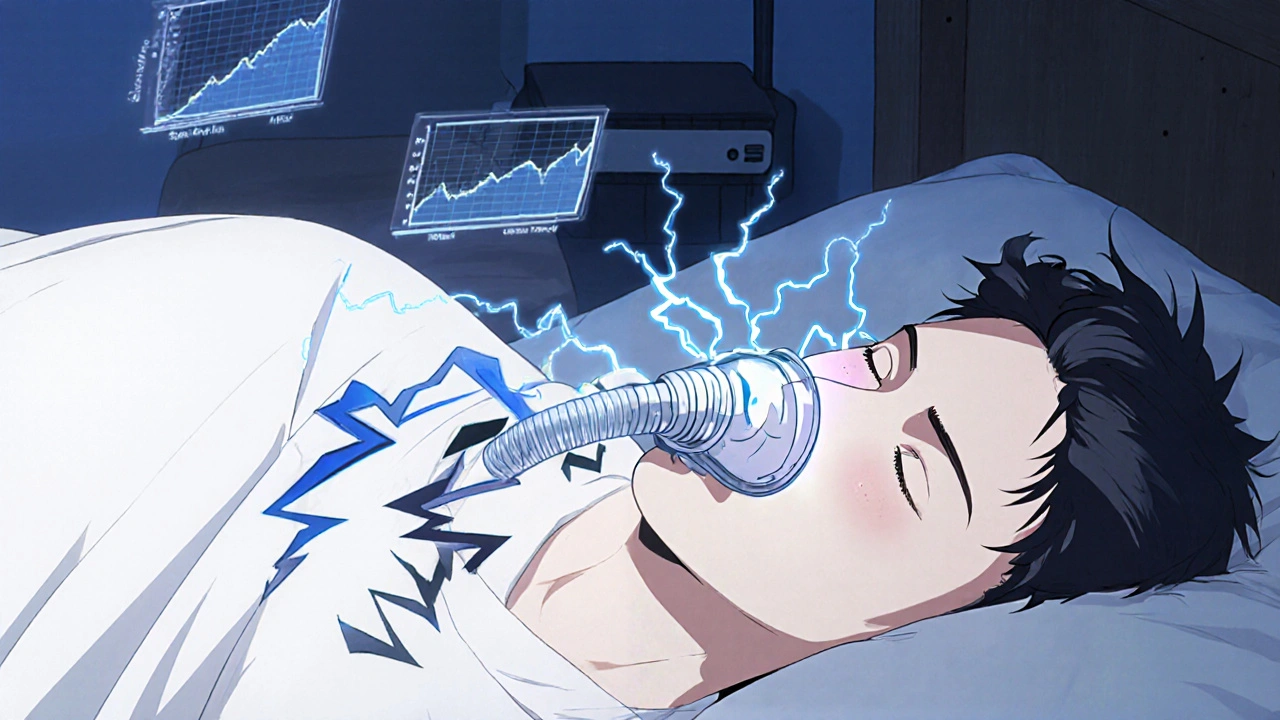
What Is Obstructive Sleep Apnea?
Obstructive sleep apnea (OSA) happens when your throat muscles relax too much during sleep, blocking your airway. This causes breathing to stop and start repeatedly-sometimes dozens of times an hour. You might not even notice it, but your body does. Your brain wakes you up just enough to restart breathing, which fragments your sleep. The result? You wake up exhausted, even after eight hours in bed. Snoring, gasping at night, and daytime fatigue are common signs. But OSA isn’t just about being tired. It raises your risk for high blood pressure, heart attacks, strokes, and even car accidents. About 1 billion people worldwide have it, and most don’t know they do.
Why CPAP Is Still the Gold Standard
Continuous Positive Airway Pressure (CPAP) therapy has been the go-to treatment for OSA since the 1980s, developed by Australian researchers at the University of Sydney. It works by delivering a steady stream of air through a mask, keeping your airway open so you can breathe normally. Modern machines are quieter, lighter, and smarter than ever. Auto-CPAP devices adjust pressure on the fly based on your breathing, while BiPAP machines give different pressures for inhaling and exhaling-helpful if you struggle with high pressure settings.
When used correctly, CPAP slashes your apnea events from severe levels (over 30 per hour) down to near-normal (under 5). Studies show it improves daytime alertness by 40%, lowers systolic blood pressure by 5-10 mmHg, and cuts sleepiness scores on the Epworth scale from 18 to under 9 in six months. For people with heart problems or diabetes, CPAP isn’t just helpful-it’s life-saving.
How CPAP Works: Masks, Machines, and Settings
CPAP isn’t one-size-fits-all. There are three main types of masks: nasal pillows (fit under the nose), nasal masks (cover the nose), and full-face masks (cover nose and mouth). About 62% of people who start with nasal masks end up switching to full-face within six months because they breathe through their mouth during sleep. The machine itself is small-about the size of a shoebox-and weighs less than 3 pounds. Most run on 26-30 decibels of noise, quieter than a whisper.
Pressure settings usually fall between 6-12 cm H₂O, determined during a sleep study. Many machines now track your usage, leak rates, and breathing events via Bluetooth apps like ResMed’s AirView or Philips’ DreamMapper. These help both you and your doctor see if you’re using it enough. Medicare and insurers require at least 4 hours of use per night on 70% of nights to keep covering the device. About 70% of users hit that mark.
The Big Problem: Adherence
Here’s the catch: CPAP only works if you use it. And many people don’t. About half of new users stop within the first year. The top complaints? Mask discomfort (35%), feeling claustrophobic (12%), dry mouth (25%), and nasal congestion (30%). One Reddit user said, “I’ve tried five masks over two years and still can’t tolerate more than two hours.” Another shared, “Switched to nasal pillows-now I get seven hours a night.”
Why do people quit? It’s not just discomfort. Some feel the machine is too bulky to travel with. Others find the noise disruptive-even though modern machines are quiet, the sound of air rushing can be unnerving at first. The good news? Most issues can be fixed. Heated humidifiers solve dryness for 78% of users. Chin straps help with mouth breathing. Trying a different mask style often makes all the difference. And patience matters: it takes most people 2-4 weeks to adjust.

Alternative Treatments: What Else Works?
If CPAP doesn’t work for you, you’re not out of options. Oral appliances-custom-fitted mouthpieces that push your jaw forward-are the most common alternative. They’re smaller, quieter, and easier to travel with. Studies show people use them 77% of nights after a year, compared to CPAP’s average of 4-5 hours per night. They’re especially effective for mild to moderate OSA and for people who can’t tolerate CPAP.
Surgery is another path, but it’s not a magic fix. Procedures like UPPP (removing excess throat tissue) work for only 40-60% of patients. Hypoglossal nerve stimulation (Inspire therapy) implants a device that stimulates the tongue muscle to keep the airway open. It reduces apnea events by 79%, but costs around $35,000 and requires surgery. It’s usually reserved for people who can’t use CPAP or oral appliances.
Positional therapy is gaining attention for those whose apnea only happens when sleeping on their back. Devices like NightBalance gently vibrate to encourage side sleeping, reducing apnea events by 51% in positional OSA cases. Lifestyle changes-losing weight, cutting alcohol, quitting smoking-also help. One study found a 10% weight loss cut apnea severity by half.
CPAP vs. Oral Appliances: The Real Comparison
| Feature | CPAP | Oral Appliance |
|---|---|---|
| Effectiveness (AHI reduction) | 90%+ reduction when used 7+ hours/night | 60-70% reduction (best for mild-moderate OSA) |
| Adherence rate (after 1 year) | 40-50% | 77% |
| Comfort | Lower (mask, tubing, noise) | Higher (small, no air pressure) |
| Travel-friendly | No (needs power, bulky) | Yes (fits in a pill case) |
| Cost (out-of-pocket) | $500-$3,000 (often covered by insurance) | $1,500-$5,000 (less likely covered) |
| Best for | Severe OSA, cardiovascular risk | Mild-moderate OSA, CPAP intolerance |
Who Should Avoid CPAP?
Not everyone benefits equally from CPAP. New research shows your brain’s “arousal threshold” matters. If you wake up easily during sleep disruptions, CPAP feels like a miracle-you’ll feel more alert, sharper, and calmer. But if you’re a deep sleeper with a low arousal threshold, CPAP might not improve your daytime thinking at all. In fact, a major study found no cognitive gains in this group. That’s why experts now say: if you’ve tried CPAP and feel no difference, it might not be the right tool for your body.
Also, if you have severe nasal congestion, chronic sinus issues, or anxiety around masks, CPAP can be more frustrating than helpful. In these cases, oral appliances or positional therapy may be better first steps.
What’s Next for Sleep Apnea Treatment?
The future is getting smarter. New CPAP machines now detect subtle breathing changes before full apneas happen. ResMed’s AirSense 11, released in 2022, is 15% better at catching early warning signs. Apps like Nightware use biofeedback to help users fall asleep faster and stay asleep longer-boosting CPAP adherence by 22% in early trials.
Researchers are also exploring personalized pressure algorithms based on 3D scans of your airway. Imagine a machine that learns your breathing pattern and adjusts in real time-not just to your events, but to your anatomy. There’s even work on wearable sensors that track blood oxygen, heart rate, and snoring sounds without a mask.
But the biggest shift might be in how we choose treatment. Instead of pushing CPAP on everyone, doctors are starting to match therapy to your physiology. If you’re a deep sleeper with low arousal thresholds? Maybe skip CPAP and start with an oral appliance. If you’re overweight and have positional apnea? Try weight loss and a side-sleeping device first.
Getting Started: What to Do Now
If you suspect you have OSA, start with a sleep test. Home tests are common now-they measure your breathing, oxygen levels, and heart rate while you sleep in your own bed. If results show moderate to severe OSA, your doctor will likely recommend CPAP. If it’s mild, they might suggest an oral appliance or lifestyle changes first.
Once you get a machine:
- Try different masks until you find one that feels comfortable.
- Use a humidifier if your nose feels dry or stuffy.
- Start with 1-2 hours a day, even while awake, to get used to the air pressure.
- Track your usage with the app-it helps you stay accountable.
- Call your DME provider if you’re struggling. Most offer 24/7 support.
Don’t give up after a week. It takes time. But if you stick with it, you’ll likely notice changes: less snoring, more energy, better focus, and fewer morning headaches.
Final Thoughts: There’s No One-Size-Fits-All
CPAP is powerful, proven, and life-changing-for those who use it. But it’s not the only answer. Oral appliances, positional therapy, weight loss, and even surgery have their place. The key is finding what works for you, not what’s advertised as the “best.”
OSA is a chronic condition, not a quick fix. Treatment isn’t about perfection-it’s about consistency. Even using CPAP 4 hours a night is better than none. And if CPAP doesn’t click? Talk to your sleep specialist. There’s another option out there. You just need to keep looking.
Is CPAP the only treatment for sleep apnea?
No, CPAP is the most effective treatment for moderate to severe obstructive sleep apnea, but it’s not the only one. Oral appliances, positional therapy devices, weight loss, and surgeries like uvulopalatopharyngoplasty (UPPP) or hypoglossal nerve stimulation (Inspire) are alternatives. Oral appliances are especially popular for mild to moderate cases or for people who can’t tolerate CPAP due to discomfort or claustrophobia.
Why do so many people stop using CPAP?
The most common reasons are mask discomfort, feeling claustrophobic, dry mouth or nose, and difficulty adjusting to the air pressure. About 50% of people stop using CPAP within the first year. Many of these issues can be solved-switching mask types, adding a humidifier, or using a chin strap can make a big difference. Patience and support from a sleep clinic also improve long-term use.
Are oral appliances as effective as CPAP?
For mild to moderate sleep apnea, oral appliances can be nearly as effective as CPAP. But for severe cases, CPAP is still superior at reducing breathing interruptions. The big advantage of oral appliances is adherence-people use them more consistently because they’re easier to wear, quieter, and portable. CPAP reduces apnea events more dramatically, but only if used 7+ hours a night. Oral appliances work well for those who can’t stick with CPAP.
Can sleep apnea be cured without a machine?
In some cases, yes. Significant weight loss can reduce or even eliminate sleep apnea in overweight individuals. Sleeping on your side instead of your back helps if your apnea is positional. Avoiding alcohol and sedatives before bed also reduces airway collapse. For some, these lifestyle changes are enough. But for moderate to severe cases, medical devices or surgery are usually needed to manage the condition long-term.
How do I know if I need CPAP or an oral appliance?
Your sleep specialist will look at your apnea severity (measured by AHI), your anatomy, your lifestyle, and your preferences. If your AHI is over 15, CPAP is usually recommended first. For mild to moderate cases, or if you’ve tried CPAP and couldn’t tolerate it, an oral appliance is a strong alternative. Some doctors now use your arousal threshold-a measure of how easily you wake up during sleep-to guide treatment. Deep sleepers with low thresholds may benefit more from oral appliances than CPAP.
Does insurance cover sleep apnea treatments?
Most insurance plans, including Medicare, cover CPAP machines and supplies if you have a diagnosis of moderate to severe sleep apnea and meet usage requirements (usually 4+ hours per night on 70% of nights). Oral appliances are often covered too, but sometimes require prior authorization and proof that CPAP failed. Surgery and nerve stimulation devices like Inspire are typically covered only after other treatments have been tried and failed. Always check with your provider before starting treatment.





Chris Ashley
November 13, 2025 AT 21:26Bro I tried CPAP for 3 weeks and it felt like sleeping with a jet engine strapped to my face. Mask leaked, nose dried out, and I kept yanking it off at 3 a.m. Then I got an oral appliance - tiny, no tubes, I can even talk with it in. Yeah it’s pricier, but I sleep 7 hours now. No more 10 a.m. naps. 🤘
kshitij pandey
November 15, 2025 AT 15:36From India, here! My uncle had OSA and we thought it was just snoring. Then he had a stroke. After that, we got him a CPAP - he hated it. So we tried a simple chin strap and side-sleeping pillow. He sleeps better now, and no more hospital visits. You don’t need fancy gadgets if you find what fits your body. Stay patient, stay healthy!
Brittany C
November 15, 2025 AT 17:26As a sleep tech, I’ve seen this play out 200+ times. The AHI reduction stats are solid, but the adherence gap isn’t about laziness - it’s about poor patient-treatment matching. CPAP isn’t ‘better’ universally; it’s just the most studied. We need more phenotyping: arousal thresholds, anatomical phenotypes, even circadian typing. Otherwise we’re just throwing machines at people like it’s a one-size-fits-all drug.
Sean Evans
November 17, 2025 AT 10:18LMAO so people are still acting like CPAP is some sacred cow? 🤡 You’re telling me 50% of users quit because it’s ‘uncomfortable’? Bro, it’s a LIFE-SAVING device. If you can’t tolerate it, maybe your lifestyle is the problem - you’re obese, drink nightly, and sleep on your back. Stop blaming the machine. Get your act together. Also, oral appliances? For severe OSA? That’s like using a bandaid on a severed artery. 😒
Anjan Patel
November 18, 2025 AT 16:44OH MY GOD. I JUST REALIZED - I’ve been sleeping with my mouth open for 12 YEARS and no one told me?! I thought I was just a ‘heavy sleeper’ - turns out I was gasping for air like a fish on land. I got a nasal pillow mask after reading this and now I wake up feeling human. I cried. I’m not joking. I’m 32 and I just had my first full night of sleep since college. Thank you, internet. 🥲
Scarlett Walker
November 20, 2025 AT 05:34Just wanted to say - if you’re on the fence about CPAP, don’t give up after a week. I was the guy who hated the mask, hated the noise, hated everything. Then I tried a heated humidifier + a different mask (full face, y’all) and now I forget I’m even wearing it. It’s not perfect, but it’s the closest thing to magic I’ve found. You deserve to wake up feeling alive.
Hrudananda Rath
November 22, 2025 AT 02:16It is, with profound regret, an epistemological travesty that the medical-industrial complex continues to prioritize CPAP as the de facto standard without sufficient regard for individual physiological variance. The reliance on AHI metrics alone, divorced from neurocognitive phenotyping, represents a reductionist paradigm that is both clinically myopic and ethically suspect. One must question the hegemony of the machine when human biology resists its imposition.
Brian Bell
November 24, 2025 AT 00:57Oral appliance guy here. I travel for work all the time. CPAP? Nah. I throw my appliance in my pocket, charge it in the hotel, and sleep like a baby. No cords, no noise, no drama. And honestly? I feel better than I did before I even knew I had OSA. Don’t let anyone tell you it’s ‘not as good’ - if it works for you, it’s good enough. 😎
Nathan Hsu
November 24, 2025 AT 05:56It is imperative to note, with the utmost gravity, that the assertion that ‘CPAP is not the only answer’ - while superficially plausible - must be contextualized within the framework of clinical evidence, insurance reimbursement structures, and the socioeconomic disparities in access to care. The oral appliance, while convenient, is often inaccessible to low-income populations due to lack of coverage - thus, the ‘choice’ is often illusory. We must advocate for equitable access - not just alternative therapies.