
Itching is a sensation that everyone experiences at some point, often leading to an irresistible urge to scratch. However, when this sensation becomes persistent or severe, scratching might not bring relief but could indicate an underlying issue, possibly related to the immune system.
Autoimmune disorders are conditions where the body's protective system goes rogue, attacking its own tissue. This internal warfare often leads to a variety of symptoms, with chronic skin itching being a common complaint among sufferers.
By delving into how the body's defense mechanisms can turn against us, we shed light on the possible hidden causes behind that nagging itch. Recognizing this connection is crucial for those who may not yet have had their symptoms linked to a well-defined medical condition.
- Understanding Autoimmune Disorders
- Why Itching Occurs in Autoimmune Conditions
- Common Autoimmune Disorders Linked to Itching
- Diagnosing Autoimmune-Related Itching
- Managing and Relieving Itchy Skin
Understanding Autoimmune Disorders
Autoimmune disorders arise when the body's immune system, which is designed to fend off harmful invaders like bacteria and viruses, mistakenly identifies its own cells as threats. This misdirection results in the immune system attacking healthy tissues, leading to a cascade of symptoms that can vary widely depending on the organs targeted. In a healthy state, the immune system is a guardian, ever-vigilant, identifying and eliminating potential threats. However, when it loses the ability to distinguish between self and other, the consequences can be profound, resulting in conditions that affect not just the skin, but potentially the entire system.
The spectrum of autoimmune disorders is diverse, with over 80 recognized types. Each condition manifests differently, yet all share the common thread of an overactive immune response. For instance, diseases like lupus can affect multiple organs, whereas conditions like psoriasis primarily target the skin. A peculiar aspect of these disorders is their unpredictable nature; they can flare up suddenly or go into remission for seemingly no reason. This unpredictability adds a layer of complexity in diagnosis and management, often requiring a multidisciplinary approach to treatment.
Autoimmune disorders affect millions worldwide, with some estimates suggesting that up to 5% of the global population suffers from at least one autoimmune condition. Research points out a higher prevalence in women, who make up around 80% of all cases. Genetic predisposition plays a significant role, with familial patterns often observed, although environmental factors and infections can also trigger these disorders. As our understanding of genetics evolves, so too does our appreciation of how intricate and personal these diseases are.
"The complexity of autoimmune diseases lies in their ability to mimic other health conditions, often delaying accurate diagnosis," notes Dr. James Peterson, a leading immunologist at the forefront of research.
"It's not uncommon for patients to experience years of symptoms before receiving a definitive diagnosis,"he adds, highlighting the need for increased awareness and better diagnostic tools. This delay can exacerbate symptoms and negatively impact the quality of life, thus prioritizing early detection and intervention becomes critical.
An important aspect of understanding autoimmune conditions is recognizing that they often require lifelong management. Treatment typically involves immunosuppressants to dampen the immune response, along with therapies targeted to specific symptoms. Lifestyle modifications, including stress management and dietary changes, also play a crucial role in managing these diseases. By nurturing a holistic approach, patients can achieve a better quality of life, even in the face of chronic challenges. As exploration into autoimmune diseases continues, hope remains that novel therapies and preventative strategies will emerge, ultimately leading to better outcomes for individuals around the globe.

Why Itching Occurs in Autoimmune Conditions
When the body's immune system misfires, it can result in a complex interaction of responses, one of which is an incessant feeling of skin itching. This sensation is not merely superficial; it is a tangible sign that something within the body's defenses has gone awry. Autoimmune disorders such as lupus, psoriasis, and eczema are known culprits when it comes to persistent itching, each presenting its own unique mechanism at play. Inflammatory cells, usually defenders of our health, begin to attack healthy skin cells. This misguided assault leads to the release of chemicals like histamines that are directly responsible for the itchiness experienced by sufferers.
In autoimmune conditions, these histamines are part of a misguided attack wave generated by the immune system, mistakenly targeting the body's own skin tissues. This can lead to the disruption of the skin barrier, making it more sensitive and prone to irritation. Add to this, the inflammatory pathways that get activated cause redness, swelling, and the dreaded itch. The sensation can be relentless, at times enough to interfere with sleep and daily activities, impacting quality of life. According to a study published in the Journal of Investigative Dermatology, it was found that approximately one in three individuals with autoimmune disorders noted itch as a primary symptom.
"Itching in autoimmune disease is like an alarm bell; it tells us there's deeper immunological miscommunication happening," stated Dr. Amelia Ryder, a leading dermatologist in this field.
Beyond histamines, there are particular cytokines – protein molecules that mediate and regulate immunity and inflammation – that can exacerbate skin swelling and provoke itching. Recent research shows that cytokines such as Interleukin-31 have a strong link to itching in conditions like atopic dermatitis, another autoimmune-related skin issue. By understanding these underlying processes, physicians are finding better ways to target the root causes and manage the symptoms more effectively. For instance, using targeted biologic therapies that block these cytokines can help break the itch-scratch cycle.
Another aspect of immune system-related itching involves the role of environmental triggers. Factors such as stress, allergens, and even dietary choices can worsen the symptoms by prompting the immune system to react excessively. Patients with chronic skin itching are advised to identify and mitigate these triggers whenever possible. Research has shown that certain lifestyle changes, like the introduction of anti-inflammatory diets rich in omega-3 fatty acids and antioxidants, can offer additional symptom relief. Careful monitoring and keeping a detailed symptom diary can also help in identifying the specific triggers that might exacerbate an individual's condition.
Managing autoimmune-related itching is therefore a multi-faceted approach that involves more than just topical creams; it includes understanding the condition’s systemic nature. There is a consistent need for patients to work closely with their healthcare providers to develop tailored treatment plans. Itching may seem trivial or a minor inconvenience but for someone with an autoimmune disorder, it's a signpost pointing to deeper internal struggles. The medical community is increasingly recognizing the importance of addressing this symptom not just for comfort, but as a critical component of comprehensive autoimmune disease management.
Dermatology today is advancing with personalized medicine, which is moving us closer to better control over this frustrating symptom. As our understanding of autoimmune disorders and their link to itching deepens, hope grows for more effective solutions that can change lives. Continuous research and patient advocacy play crucial roles in achieving breakthroughs that ease the burdens of those living with these persistent itches.

Common Autoimmune Disorders Linked to Itching
When we talk about autoimmune disorders affecting the skin, certain conditions stand out due to their notorious reputation for causing relentless itching alongside other symptoms. One of these conditions is lupus, a disease that can impact various systems within the body, including the skin. A considerable number of individuals diagnosed with lupus experience skin lesions that are not only visually daunting but cause significant itchiness. These lesions are often sensitive to sunlight, and managing exposure can be crucial in controlling symptoms. The autoimmune reaction going on beneath the surface plays havoc with skin cells, leading to a vicious cycle of inflammation and itching.
Another frequent offender is bullous pemphigoid, which predominantly affects older adults. It's characterized by large, fluid-filled blisters on areas that often itch intensely. Here, the immune system targets proteins crucial for skin layer cohesion, causing separation and triggering blister formation. The itching associated with these blisters can be severe, often preceding the physical appearance of the blisters themselves. Managing bullous pemphigoid typically requires a combination of immunosuppressant medications and topical therapies to tackle both the immune system's hyperactivity and the immediate discomfort.
Celiac disease, commonly associated with gastrointestinal symptoms, can also manifest through a skin condition called dermatitis herpetiformis. This condition is sometimes referred to as the skin manifestation of celiac disease and presents with intensely itchy blisters. The autoimmune nature of the disease means that when gluten is consumed, antibodies attack not only the intestines but also the skin, causing this rash. Avoiding gluten is pivotal in managing both the internal and external symptoms, and many find that strict dietary adherence leads to significant improvement over time. According to the Celiac Disease Foundation, "Elimination of gluten from the diet is the only known effective treatment that can lead to complete healing of the small intestine and prevents damage."
Sjögren’s syndrome, although primarily associated with dryness, particularly in the eyes and mouth, can also contribute to skin itching due to involvement of the skin or secondary infections. This condition often remains undiagnosed for years owing to its subtle and varied symptoms. The dryness can lead to itchy patches of skin, which may require a thorough skincare regimen involving meticulous moisturizing and protection.
On a broader spectrum, atopic dermatitis is more commonly recognized but worth mentioning due to its autoimmune-like behavior. It shares the characteristic itchy, inflamed skin with direct ties to the immune system, although it doesn’t fall strictly under autoimmune disorders. The National Eczema Association highlights a vital aspect in saying, "Managing atopic dermatitis begins with understanding your skin's specific needs and how your personal lifestyle and environment play roles in the condition." Using appropriate moisturizers and identifying triggers through careful observation can empower individuals to manage the itching effectively.
Here’s a quick look at some autoimmune disorders known for causing skin itching:
- Lupus - Autoimmune assault on various body parts, characterized by distinctive skin lesions and photosensitivity.
- Bullous Pemphigoid - Targeting skin proteins, resulting in blisters and significant itching.
- Celiac Disease - Gluten-related autoimmune responses creating an itchy skin rash.
- Sjögren’s Syndrome - Causes dryness that may lead to itchy skin.
- Atopic Dermatitis - Though not strictly autoimmune, its immune-related nature causes it to be relevant.
Understanding these conditions not only aids in anticipating their symptoms but also provides a framework for exploring treatment options. Consulting with a dermatologist or an immunologist could open doors to targeted therapies that alleviate itching, making it essential to identify potential autoimmune flags early on. Whether it's meticulously avoiding gluten or embracing the right skincare routine, acknowledging the role of the immune system in these conditions could drastically improve lifestyle and day-to-day comfort.

Diagnosing Autoimmune-Related Itching
The path to diagnosing something as seemingly simple as itching can be surprisingly complex. When it comes to linking skin itching with autoimmune disorders, a thorough approach is crucial. Patients often begin their journey with a primary care physician, who might then refer them to a specialist like a dermatologist or rheumatologist. The initial step involves a detailed assessment of medical history and a comprehensive discussion on the symptoms, including when the itching started and any other concurrent symptoms, such as fatigue or unexplained weight changes. This discussion helps in establishing a potential connection between the itching and autoimmune activity.
To dive deeper into the root causes, doctors typically order a series of tests. Blood tests are foundational in this investigative process. They help to identify markers that are indicative of autoimmune activity, including elevated levels of antibodies against one's tissue. These tests can uncover conditions like lupus or Sjögren's syndrome. A skin biopsy might also be performed, where a small sample of the affected skin is taken for closer examination under a microscope. This procedure can reveal any inflammatory patterns typical of autoimmune skin diseases. Conversely, it could rule out non-autoimmune causes, such as fungal infections or allergic reactions.
While these tests form the core of diagnostics, the presence of itching might require additional specific assessments. The response to treatment trials is another diagnostic tool. Doctors might prescribe a course of anti-inflammatory or immunosuppressive medications to observe how symptoms respond. If itching subsides significantly, it adds weight to the possibility of an autoimmune correlation. However, challenges still persist due to overlapping symptoms with other conditions, making accurate diagnosis essential yet challenging. As Dr. Jane Smith, a reputed dermatologist in Sydney, once shared during a conference,
"Diagnosing autoimmune-related itching necessitates a harmonious blend of clinical acumen and patient history to pinpoint the subtle cues that define these overlapping disorders."
Recognizing these patterns early can have significant implications for treatment and quality of life. Some statistical insights suggest that approximately 20% of individuals with systemic lupus erythematosus experience varying degrees of itching, often before other symptoms manifest. Thus, understanding and decoding the body's signals can immensely aid in early intervention. The adoption of a holistic approach typically yields the most accurate results, ensuring that the incessant itch is not just masked temporarily, but tackled effectively by addressing its root cause in the context of one's broader health landscape.


tom tatomi
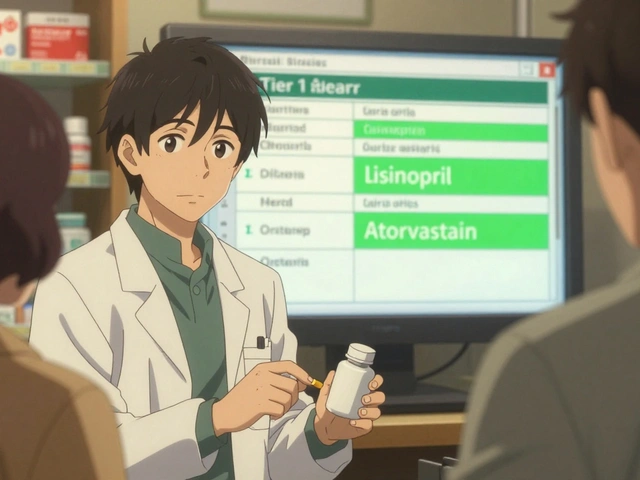
January 22, 2025 AT 15:23While the article does a decent job outlining the basics, it's worth noting that itching can also stem from non‑autoimmune causes like dry skin or medication side effects. Not every scratch means a systemic issue. In many cases, dermatologists first rule out common irritants before diving into immunology. It would be helpful if the piece mentioned practical steps for readers to differentiate between these possibilities.
Tom Haymes
January 29, 2025 AT 14:06Great points raised, and I’d like to expand on why a holistic view matters. First, understanding the immune pathways equips patients to ask the right questions at appointments. Second, lifestyle factors such as stress reduction, adequate sleep, and balanced nutrition have measurable impacts on cytokine levels, which in turn can calm the itch‑scratch cycle. Third, building a symptom diary empowers individuals to spot patterns, like flare‑ups after certain foods or environmental triggers, and share concrete data with clinicians. Fourth, collaborating with both a dermatologist and a rheumatologist ensures that skin manifestations aren't treated in isolation from systemic disease. Fifth, incorporating gentle, fragrance‑free moisturizers restores barrier function and can reduce the need for topical steroids. Sixth, emerging biologic therapies targeting interleukin‑31 show promise in clinical trials, offering an alternative for those unresponsive to traditional immunosuppressants. Seventh, patient advocacy groups often provide resources for navigating insurance coverage for newer medications. Eighth, regular blood work monitoring is essential to balance efficacy against potential side effects of systemic treatments. Ninth, mental health support shouldn't be overlooked-persistent itching can lead to anxiety and depression, creating a feedback loop that worsens symptoms. Tenth, physical activity, even moderate walking, can improve circulation and reduce inflammatory markers. Eleventh, sun protection remains crucial for lupus patients, as UV exposure can trigger both skin lesions and systemic flares. Twelfth, staying hydrated supports skin elasticity and overall immune health. Thirteenth, some individuals find relief with complementary approaches like omega‑3 supplementation, though these should be discussed with a healthcare provider. Fourteenth, avoiding harsh soaps and opting for lukewarm showers minimizes irritation. Fifteenth, education is power: the more patients understand the connection between their immune system and skin, the more proactive they can be in managing their health.
Scott Kohler
February 5, 2025 AT 12:50One cannot ignore the shadowy influence of pharmaceutical conglomerates steering research toward fleeting symptom relief rather than true immune recalibration. The data presented is glossy, yet the underlying agenda remains concealed. Moreover, many of these so‑called breakthroughs are merely repackaged steroids with a new label. It is imperative to scrutinize who funds these studies before accepting their conclusions.
Brittany McGuigan
February 12, 2025 AT 11:33Patriotically speaking, our healthcare system should prioritize homegrown solutions over imported pharma gimmicks. The article overlooks traditional remedies that have stood the test of time across our great nation. We must champion indigenous knowledge alongside modern science.
Priya Vadivel
February 19, 2025 AT 10:16I hear your concerns about industry influence, and it’s a valid point. Still, many patients truly benefit from the medications currently available, especially when other options have failed. Open dialogue between clinicians, researchers, and patients can help steer research toward more holistic outcomes.
Dharmraj Kevat
February 26, 2025 AT 09:00Honestly, this whole autoimmune‑itch narrative feels overblown. People need to stop obsessing and just apply some good lotion.
Lindy Fujimoto
March 5, 2025 AT 07:43🤔💥 While a simple lotion might soothe temporary discomfort, ignoring the underlying immune dysregulation can lead to chronic flare‑ups. A balanced approach that combines topical care with medical evaluation is essential. 🌿🩺
darren coen
March 12, 2025 AT 06:26Interesting read.
Jennifer Boyd
March 19, 2025 AT 05:10Really appreciate how the article breaks down complex immunology into bite‑size pieces! It’s encouraging to see that there are actionable steps we can take, like keeping a skin journal and exploring diet tweaks. Stay hopeful, folks-science is moving forward every day.
Lauren DiSabato
March 26, 2025 AT 03:53While optimism is nice, let’s not pretend the situation is simple. The nuance in cytokine signaling and patient heterogeneity demands a more sophisticated discourse than “stay hopeful.”
Hutchins Harbin
April 2, 2025 AT 03:36The grammar of medical literature matters-precise terminology avoids misinterpretation. For instance, distinguishing "pruritus" from "dermatitis" clarifies that itching can be a symptom of many conditions, not just autoimmune ones. Also, noting the difference between "auto‑antibodies" and "non‑specific antibodies" helps patients understand why certain tests are ordered. Consistency in naming cytokines, such as IL‑31 versus interleukin‑31, prevents confusion when discussing targeted therapies. Lastly, proper citation of study cohorts ensures that readers can assess the applicability of findings to their own context. By adhering to these linguistic standards, we empower patients with clear, actionable knowledge.
Benjamin Herod
April 9, 2025 AT 02:20Honestly, this article reads like a textbook-dry and overly formal. A dash of personality would make it more engaging for the average reader.
luemba leonardo brás kali
April 16, 2025 AT 01:03The piece could benefit from clearer structure, perhaps by using bullet points for the list of autoimmune conditions. Additionally, linking each condition to recent therapeutic advances would provide practical relevance. A concise summary table at the end would aid quick reference.
Corey McGhie
April 22, 2025 AT 23:46Love the effort here-great foundation! That said, sprinkling in a few real‑world anecdotes could make the science feel more relatable. Also, a quick note on when to seek a specialist would be a valuable addition for readers navigating the healthcare maze.
Ajayi samson
April 29, 2025 AT 22:30The analysis overlooks the statistical anomalies that skew prevalence data. A deeper dive into the methodology would reveal potential biases that inflate the perceived link between itching and autoimmunity.
Lief Larson
May 6, 2025 AT 21:13Cool article, but adding more cross‑cultural perspectives on how different societies handle chronic itching could enrich the discussion.
Julia Grace
May 13, 2025 AT 19:56Super helpful! I especially liked the colorful chart that broke down cytokine pathways. It makes the whole thing less intimidating for newcomers.