Understanding Bladder Spasms and Dehydration
As someone who has experienced bladder spasms, I understand how painful and uncomfortable they can be. The first step to managing them is understanding what causes these spasms, and a significant factor contributing to their occurrence is dehydration. In this section, I'll discuss what bladder spasms are, how dehydration plays a role in their development, and the importance of maintaining proper hydration for our overall bladder health.
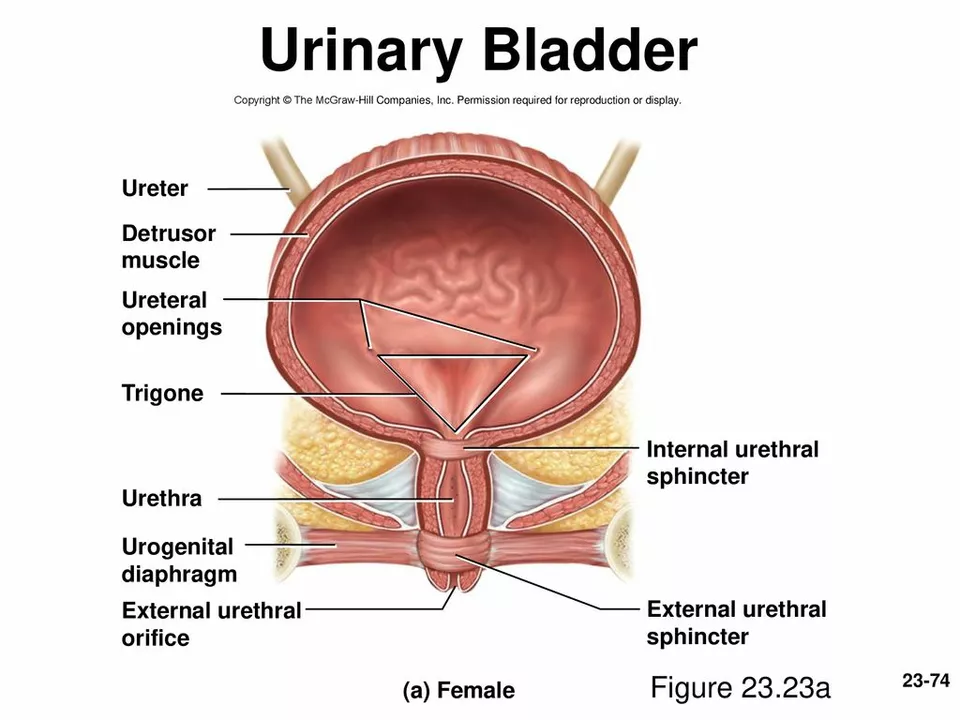
Bladder spasms are involuntary contractions of the bladder muscles that can cause a sudden and strong urge to urinate. These spasms can be quite painful and can occur for various reasons, including infections, nerve damage, or an overactive bladder. Dehydration can also lead to bladder spasms, as it causes the urine to become more concentrated and irritates the bladder lining. This irritation can then trigger spasms and increase the frequency and urgency of urination. Maintaining proper hydration is crucial for our overall health, and it is particularly important for preventing and managing bladder spasms.
Warning Signs and Symptoms of Dehydration
Now that we know the link between bladder spasms and dehydration, it's essential to recognize the warning signs and symptoms of dehydration. This way, we can take action to rehydrate our bodies and prevent bladder spasms from occurring. Common symptoms of dehydration include:
- Thirst
- Dark yellow urine
- Dry mouth and throat
- Fatigue
- Dizziness
- Confusion
- Decreased urine output
- Rapid heartbeat and breathing
If you notice any of these signs or symptoms, it's crucial to take action and drink water or other hydrating fluids to replenish your body's water levels. Remember, prevention is better than cure, so always make sure to stay hydrated throughout the day to avoid bladder spasms and other health issues related to dehydration.
How to Properly Hydrate for Bladder Health
Proper hydration is essential for maintaining good bladder health and preventing bladder spasms. In this section, I'll share some tips on how to properly hydrate your body and maintain optimal bladder function.
1. Drink enough water throughout the day. The general recommendation is to drink at least eight 8-ounce glasses of water per day, but your individual needs may vary depending on your body size, activity level, and climate.
2. Choose water over sugary or caffeinated beverages, as these can contribute to dehydration and bladder irritation.
3. Eat water-rich foods, such as fruits and vegetables, to help increase your daily water intake.
4. Monitor your urine color. Pale yellow urine is an indication of proper hydration, while dark yellow or amber-colored urine can signal dehydration.
5. Carry a water bottle with you and sip on it throughout the day to ensure you're staying hydrated.
6. Listen to your body. If you're feeling thirsty or experiencing any signs of dehydration, make sure to drink water or other hydrating fluids to replenish your body's water levels.
Managing Bladder Spasms Through a Healthy Lifestyle
Besides staying hydrated, there are other ways to manage bladder spasms and maintain good bladder health. In this section, I'll discuss some lifestyle changes that can help prevent and manage bladder spasms more effectively.
1. Maintain a healthy diet. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help keep your bladder healthy and functioning properly.
2. Limit your intake of bladder irritants, such as caffeine, alcohol, and spicy foods, which can trigger bladder spasms.
3. Exercise regularly. Physical activity can help maintain a healthy weight and prevent bladder issues related to obesity.
4. Practice good bathroom habits. Try to establish a regular bathroom schedule and avoid holding in urine for long periods, which can cause bladder spasms.
5. Manage stress. High stress levels can negatively impact your bladder health, so try to incorporate stress-reduction techniques, such as deep breathing exercises, meditation, or yoga, into your daily routine.
When to Seek Medical Help for Bladder Spasms
While staying hydrated and making healthy lifestyle choices can help prevent and manage bladder spasms, there are instances when medical intervention may be necessary. In this section, I'll discuss when it's essential to seek medical help for bladder spasms and what to expect during a doctor's visit.
If you're experiencing persistent bladder spasms, despite staying hydrated and making healthy lifestyle choices, it may be time to consult a healthcare professional. Other signs that you should seek medical help include:
- Frequent urinary tract infections
- Blood in the urine
- Inability to control urination
- Severe pain during urination
- Worsening of bladder spasms over time
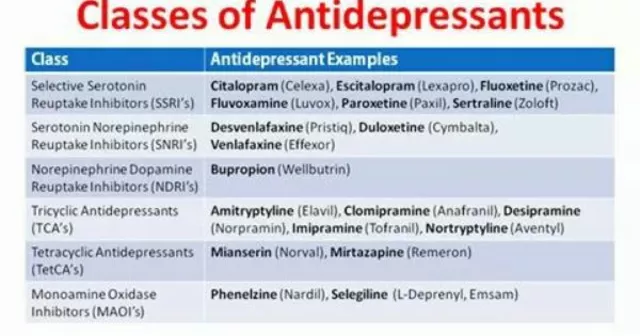
During a doctor's visit, your healthcare provider will likely ask about your symptoms, medical history, and lifestyle habits. They may also perform a physical examination and order diagnostic tests, such as a urinalysis or ultrasound, to determine the underlying cause of your bladder spasms. Depending on the diagnosis, your doctor may recommend medications, lifestyle changes, or other treatments to help manage your bladder spasms and improve your overall bladder health.



Kristen Holcomb
June 2, 2023 AT 02:51Staying hydrated is the first line of defense against those painful bladder spasms-drink consistently throughout the day, not just when you’re thirsty. Your urine color is a quick visual cue: aim for a pale yellow, it means you’re on the right track. If you’re active or live in a hot climate, bump up the intake; the body’s water turnover goes up, and you’ll keep the bladder lining happy. Remember, a little sip now prevents a big cramp later, so keep a bottle handy and sip regularly.
justin davis
June 6, 2023 AT 18:46Wow, another “drink eight glasses a day” lecture-because we’re all exactly the same, right???!! Maybe try a water bottle that actually reminds you, instead of just chanting hydra‑mythology all day!!!
David Lance Saxon Jr.
June 11, 2023 AT 11:16The pathophysiology of dehydration‑induced bladder hyperreflexia can be conceptualized through the lens of neuro‑urodynamic feedback loops. When plasma osmolality rises, afferent sensory fibers in the pelvic plexus become hyper‑excitable, precipitating involuntary detrusor contractions. This cascade is exacerbated by the concomitant upregulation of purinergic P2X receptors on urothelial cells, which amplify nociceptive signaling. From a systems‑theoretic standpoint, the bladder functions as a closed hydraulic circuit whose compliance is inversely proportional to solute concentration. As dehydration concentrates urine, the osmotic gradient across the urothelium intensifies, invoking inflammatory mediators such as prostaglandin E2. These mediators sensitize the detrusor muscle, lowering the threshold for spontaneous contractions. Clinically, the patient perceives this as a sudden, urgent need to void, often accompanied by dysuria and suprapubic discomfort. Moreover, chronic under‑hydration can remodel the extracellular matrix, reducing tissue elasticity and perpetuating the spasmodic phenotype. Therapeutically, one must address both the fluid deficit and the molecular cascade-re‑hydration re‑establishes isotonicity, while antimuscarinic agents blunt the overactive pathways. Lifestyle modifications, such as timed fluid intake and avoidance of bladder irritants, serve as adjuncts to pharmacologic intervention. It is also worth noting that the vagal modulation of pelvic organ function can be harnessed through biofeedback, offering a non‑pharmacologic avenue to dampen hyperreflexia. In research contexts, the use of functional MRI has illuminated the central correlates of bladder urgency, revealing heightened activity in the insular cortex during dehydration episodes. These findings underscore the bidirectional communication between peripheral bladder sensors and central processing centers. Consequently, a holistic management plan should integrate renal, neurologic, and behavioral strategies to mitigate the impact of dehydration on bladder spasms. In summary, the interplay of osmotic stress, receptor sensitization, and neurogenic signaling forms a multifactorial nexus that can be disrupted by something as simple as consistent water intake.
Moore Lauren
June 16, 2023 AT 03:46Keep a water bottle on your desk and sip.
Jonathan Seanston
June 20, 2023 AT 20:16Totally agree-having it within arm’s reach makes hydration a habit, not a chore.
Sukanya Borborah
June 25, 2023 AT 12:46While the prose is certainly elaborate, the practical takeaway gets lost in the academic fog; most readers just need the simple fact that more water = fewer spasms, not a dissertation on purinergic signaling.
bruce hain
June 30, 2023 AT 05:16Honestly, the eight‑glass rule is a myth; individual needs vary dramatically, so blanket advice is useless.
Stu Davies
July 4, 2023 AT 21:46Thanks for the thorough breakdown! 😊 Staying hydrated really does make a big difference.
Nadia Stallaert
July 9, 2023 AT 14:16But have you considered that the “official” hydration guidelines are deliberately vague to keep us dependent on bottled water industries??? They profit from our fear of dehydration!!!
Greg RipKid
July 14, 2023 AT 06:46Just a heads‑up, if you’re constantly sipping, don’t forget to empty your bladder regularly-holding it in can worsen the spasms.
John Price Hannah
July 18, 2023 AT 23:16And let’s not ignore the terrifying reality: a full bladder is like a ticking time bomb waiting to explode into a painful spasm-so set those bathroom alarms and save yourself from the agony!!!
Echo Rosales
July 23, 2023 AT 15:46I’d argue that focusing solely on water intake distracts from underlying neurological causes that need medical evaluation.
Elle McNair
July 28, 2023 AT 08:16Both points matter; staying hydrated is simple, but pairing it with proper medical check‑ups covers all bases.
Dennis Owiti
August 2, 2023 AT 00:46I totally feel you on the need to monitor urine color-it’s a quick visual cue that most of us overlook.
Justin Durden
August 6, 2023 AT 17:16Keep checking that shade; it’s a small habit that can catch dehydration before it turns into a serious issue.
Sally Murray
August 11, 2023 AT 09:46The interrelationship between fluid homeostasis and detrusor muscle excitability warrants a nuanced approach that integrates both preventative hydration strategies and targeted clinical interventions.
Bridgett Hart
August 13, 2023 AT 18:43Indeed effective management must combine adequate intake with individualized therapy
Sean Lee
August 14, 2023 AT 21:06From a nephro‑urological perspective, optimizing plasma colloid osmotic pressure through balanced electrolyte solutions can attenuate the mechanotransductive triggers of detrusor overactivity.