Opioid Side Effects: What You Need to Know Before Taking Them
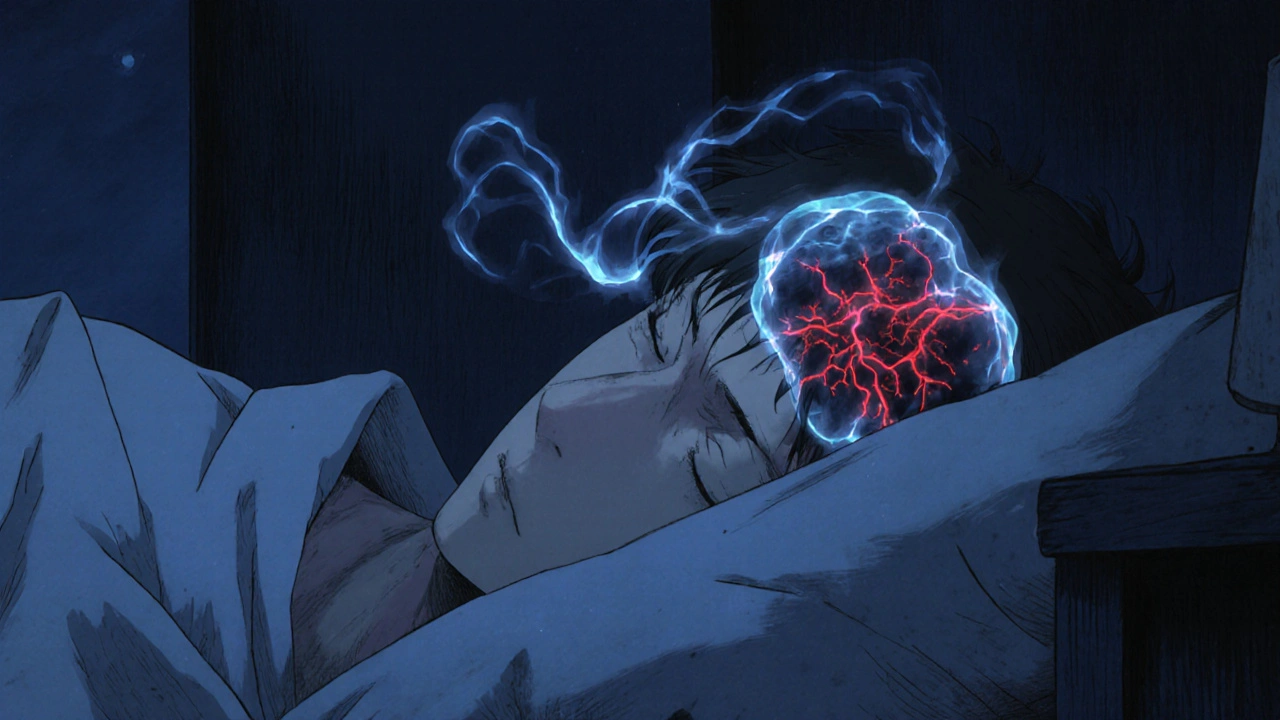
When you take opioids, a class of powerful pain-relieving drugs that include prescription painkillers like oxycodone and hydrocodone, as well as illegal drugs like heroin. Also known as narcotics, they work by binding to receptors in your brain and spinal cord to block pain signals. But they don’t just stop pain—they also slow down your breathing, change how your gut moves, and can trick your brain into craving more, even when you don’t need them.
One of the most dangerous opioid side effects, the risk of slowed or stopped breathing. Also known as respiratory depression, this is the leading cause of death in opioid overdoses. It doesn’t always come with warning signs—you might feel drowsy, then fall asleep, and never wake up. This isn’t rare. In fact, over 70% of drug overdose deaths in the U.S. involve opioids, and many happen because people didn’t realize how quickly breathing can shut down.
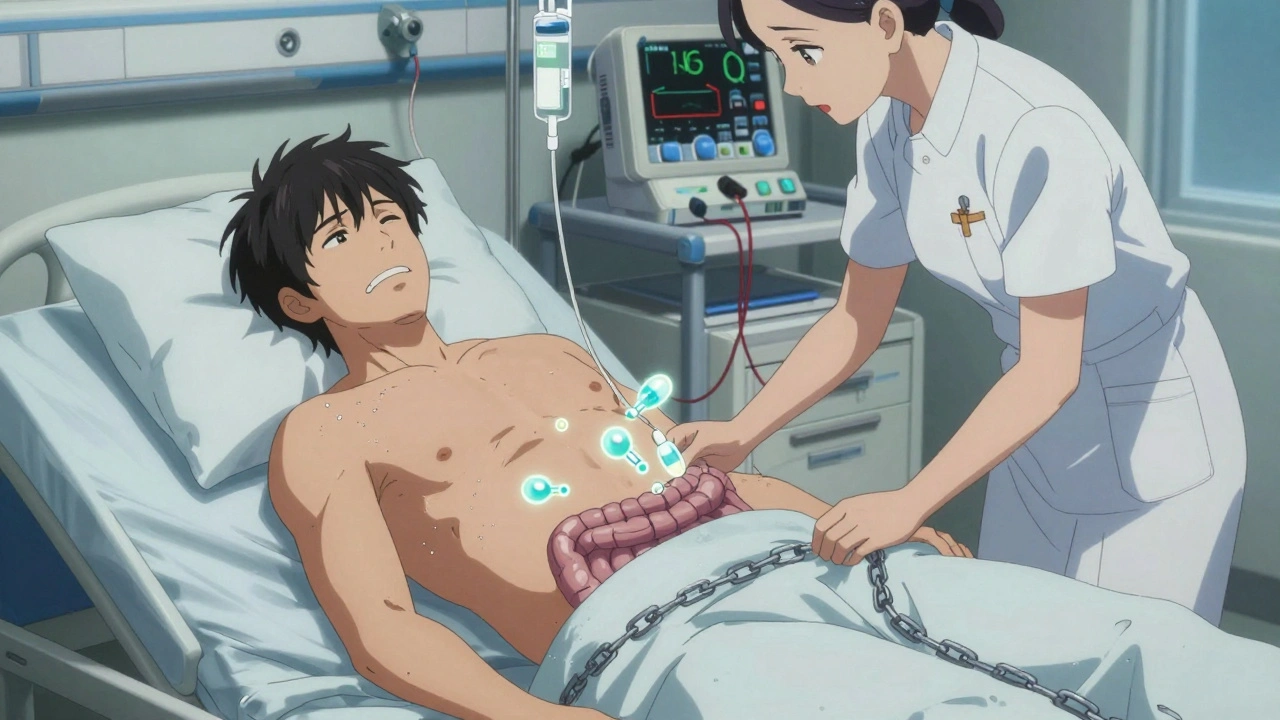
Then there’s constipation from opioids, a side effect so common it affects nearly everyone who takes them long-term. Unlike other side effects, this one sticks around even if you build tolerance to pain relief. Your gut slows down, stools become hard, and you might go days without a bowel movement. It’s not just uncomfortable—it can lead to serious complications like bowel obstruction if ignored. And let’s not forget opioid dependence, when your body starts to rely on the drug to feel normal. You might not be addicted yet, but if you feel sick when you skip a dose, or find yourself taking more than prescribed, your body is already changing. This isn’t weakness—it’s biology. Opioids rewire your brain’s reward system, and that change doesn’t vanish when you stop taking them.
Many people think side effects like dizziness or nausea will fade after a few days. Sometimes they do. But others—like constipation, mood swings, and lowered hormone levels—stick around as long as you’re on the drug. And if you’ve been on opioids for more than a few weeks, stopping suddenly can trigger withdrawal: muscle aches, sweating, diarrhea, anxiety, and insomnia. That’s why doctors don’t just hand out prescriptions anymore—they monitor use, check for signs of misuse, and often recommend alternatives like physical therapy or non-opioid pain meds.
What you’ll find below isn’t a list of warnings—it’s a practical guide to what actually happens when you take opioids. From the subtle signs you might miss to the emergency red flags that demand immediate action. You’ll see real cases, real data, and real advice from people who’ve been through it. Whether you’re taking them now, helping someone who is, or just trying to understand why this problem is so widespread, these posts give you the facts without the fluff. No scare tactics. Just what you need to stay safe.