
Rhabdomyolysis Risk Checker
Check if your medications create dangerous combinations that could lead to muscle breakdown and kidney failure. Based on evidence from clinical studies.
Your Risk Assessment
Imagine waking up with severe muscle pain, dark urine, and feeling like you’ve been hit by a truck-except you didn’t lift weights or run a marathon. You just took your usual statin and a new antibiotic for a sinus infection. That’s when rhabdomyolysis can sneak up on you. It’s not rare. It’s not theoretical. And it’s often caused by something as simple as two common medications taken together.
What Exactly Is Rhabdomyolysis?
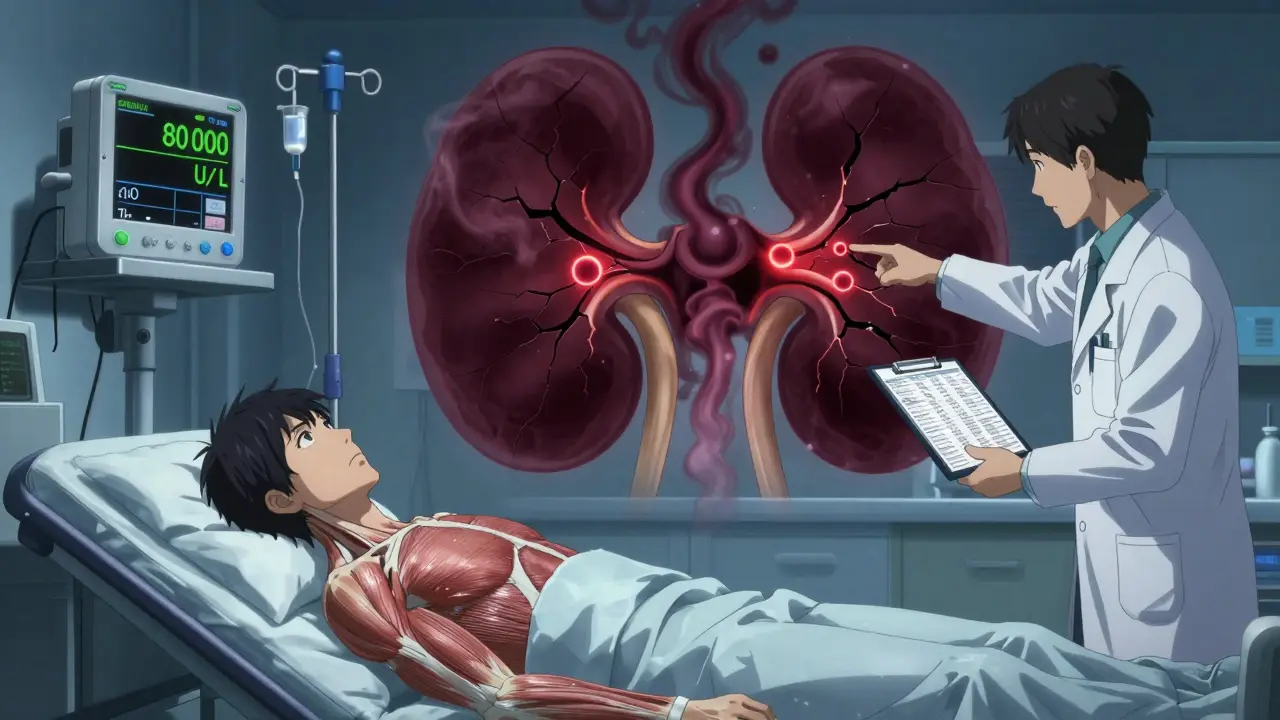
Rhabdomyolysis is when your muscle cells break down rapidly and spill their contents into your bloodstream. The main danger? Myoglobin, a protein from muscle tissue, floods your kidneys and can cause acute kidney failure. Up to half of people with severe rhabdomyolysis end up needing dialysis. About 5-15% die if their kidneys fail. It doesn’t always start with the classic signs-muscle pain, weakness, and dark urine. In fact, only about half of patients show all three. Many just feel tired, nauseous, or have vague abdominal pain. By the time they go to the ER, their creatine kinase (CK) levels are already over 10,000 U/L-sometimes over 100,000. That’s 20 times the normal limit.Medications Are the Top Cause
About 7-10% of all rhabdomyolysis cases come from drugs. And nearly two-thirds of those are linked to statins-cholesterol-lowering pills like atorvastatin (Lipitor) and simvastatin (Zocor). But here’s the catch: most of these cases aren’t from statins alone. They’re from statins mixed with other meds. The biggest red flag? Combining simvastatin with drugs that block the CYP3A4 enzyme. That’s the liver’s main system for breaking down statins. When it’s shut down, statin levels skyrocket. Erythromycin, clarithromycin, itraconazole, and even grapefruit juice can do this. One study found the risk of rhabdomyolysis jumps 18.7 times when simvastatin is taken with clarithromycin. Fibrates aren’t safe either. Gemfibrozil combined with simvastatin increases risk by 15-20 times compared to statin alone. That’s why doctors now avoid this combo entirely. Even colchicine, used for gout, becomes dangerous with clarithromycin-raising rhabdomyolysis risk by 14 times.Who’s Most at Risk?
It’s not just about the drugs. Your body matters too. - People over 65 are more than three times as likely to develop drug-induced rhabdomyolysis. - Women have a 70% higher risk than men. - Anyone with kidney problems (eGFR under 60) faces a 4.5-fold increase. - Taking five or more medications? Your risk jumps 17 times. Genetics play a role too. About 1 in 5 people carry the SLCO1B1*5 gene variant, which makes them far more sensitive to simvastatin. That’s why some people get muscle damage on low doses while others tolerate high doses fine.The Deadliest Combinations
Some drug pairs are like landmines. Here are the most dangerous ones:- Simvastatin + Clarithromycin/Erythromycin: 18.7x higher risk. Common in older adults with infections.
- Simvastatin + Gemfibrozil: 15-20x higher risk. Still prescribed despite warnings.
- Colchicine + Clarithromycin: 14.2x higher risk. Often missed because gout and infections are common in elderly.
- Erlotinib (cancer drug) + Simvastatin: CK levels over 20,000 U/L reported within days. Oncologists rarely check for this.
- Propofol (anesthesia) + prolonged ICU use: Causes mitochondrial collapse. 68% mortality when rhabdomyolysis develops.
- Leflunomide (arthritis drug) + any CYP3A4 inhibitor: CK levels can exceed 50,000 U/L. Requires plasma exchange.
What Happens in Your Body?
When muscle cells break open, they release: - Myoglobin: Turns urine dark red or brown. Clogs kidney tubules. - Electrolytes: Potassium spikes (hyperkalemia), causing dangerous heart rhythms. - Calcium: Drops sharply (hypocalcemia), leading to muscle spasms and confusion. - CK: The diagnostic marker. Levels above 5,000 U/L mean serious damage. Your kidneys try to filter this mess. But myoglobin forms crystals in the tubules, blocking flow. That’s when kidney failure starts. Without fast treatment, you’re looking at weeks on dialysis-or worse.How Doctors Diagnose It
There’s no single test. Diagnosis comes from: - CK levels: Above 1,000 U/L (5x normal) is the threshold. Severe cases hit 5,000-100,000+. - Urine test: Myoglobinuria turns urine cola-colored. But it’s not always present. - Medical history: Did you start a new drug? Change a dose? Add an antibiotic? - Symptoms: Even vague ones-fatigue, nausea, muscle stiffness-matter if you’re on high-risk meds. A 2020 study found CK >1,000 U/L has 99.2% specificity for rhabdomyolysis. That means if your CK is that high and you’re on a risky drug combo, it’s almost certainly rhabdomyolysis.What to Do If You Suspect It
Stop the medication immediately. Don’t wait for a doctor’s call. Then:- Drink water-lots of it. Aim for clear urine.
- Go to the ER. Don’t wait until tomorrow.
- Bring a list of all your meds, including supplements.

Why This Keeps Happening
Doctors aren’t ignoring the risk. But the system is broken. - 92% of patients on Reddit who developed rhabdomyolysis said their provider didn’t warn them about the interaction. - Many EHR systems don’t flag high-risk combos unless the dose is extreme. - Pharmacists aren’t always consulted when prescriptions are written. - Patients don’t know to ask. They assume their meds are safe together. The FDA’s Adverse Event Reporting System shows statin-related rhabdomyolysis cases spiked after 2020 with new antivirals like remdesivir. The EMA now requires statin labels to list exact contraindications with CYP3A4 inhibitors. But many U.S. prescribers still don’t check.Long-Term Damage and Recovery
Even if you survive, you’re not out of the woods. - 43.7% of survivors still have muscle weakness six months later. - Recovery takes 12-13 weeks without kidney damage. With dialysis? Over 28 weeks. - Some people never fully regain their strength. And the risk doesn’t go away. If you had rhabdomyolysis from a statin, you’re more likely to get it again-even with a different statin.How to Protect Yourself
If you take any of these: - Statins (atorvastatin, simvastatin, rosuvastatin) - Colchicine - Fibrates - Antiretrovirals - Cancer drugs like erlotinib - Any antibiotic or antifungal Do this:- Ask your doctor: “Could this drug interact with anything I’m already taking?”
- Ask: “Is there a safer alternative?” (e.g., pravastatin instead of simvastatin-it’s not metabolized by CYP3A4).
- Use a free drug interaction checker like Medscape or Drugs.com. Don’t rely on memory.
- Watch for early signs: unexplained muscle soreness, dark urine, fatigue. Don’t brush it off as “just getting older.”
- Get a CK test if you’re on high-risk combos and feel off-even if you think it’s nothing.




Marlon Mentolaroc
January 23, 2026 AT 15:11Bro this is wild. I had a buddy take simvastatin with clarithromycin for a sinus infection and ended up in the ICU. He thought muscle soreness was just from lifting. Turns out his CK was 87,000. No joke, he needed dialysis for three weeks. Doctors didn’t even flag the interaction. That’s terrifying.
siva lingam
January 24, 2026 AT 23:04So let me get this straight… we’re telling people to stop taking meds they’ve been on for years because some study says so? Cool. I’ll just stop taking everything and live off kale and vibes.