
Head Injury Assessment Tool
Check Your Symptoms
For patients taking blood thinners (warfarin, rivaroxaban, apixaban, aspirin, etc.), select any symptoms you or someone else is experiencing after a head injury:
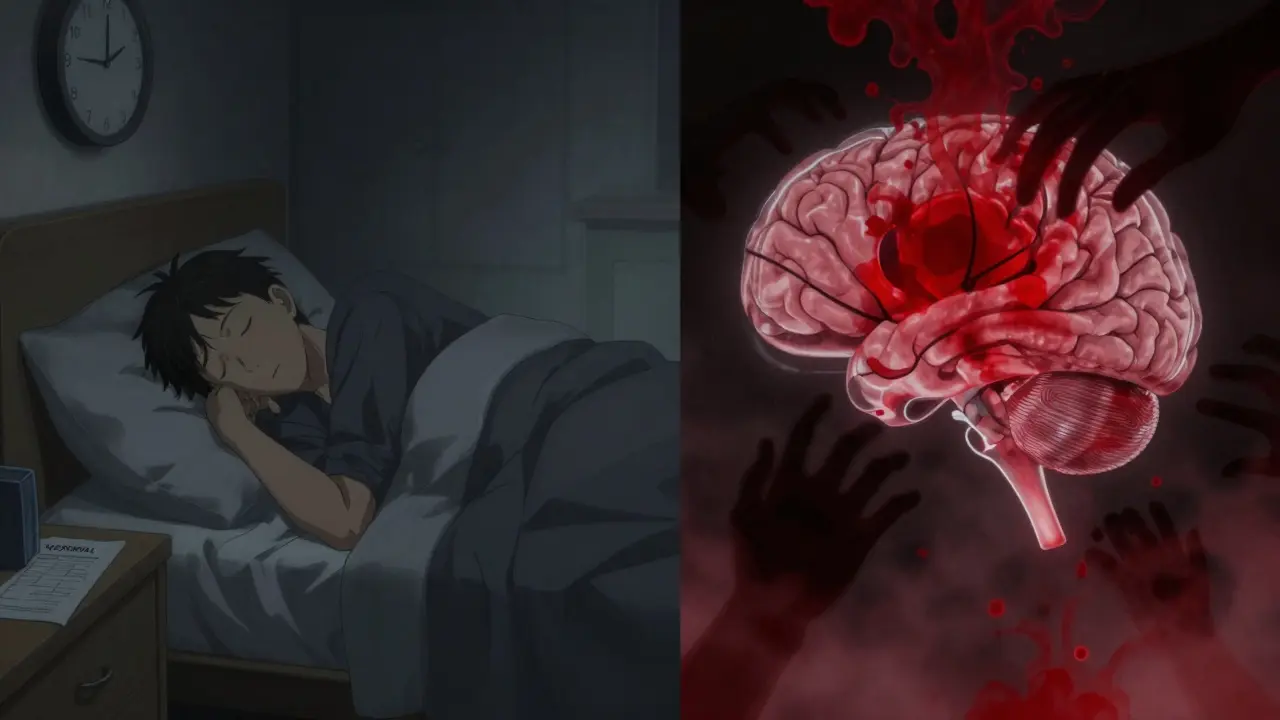
When you’re on blood thinners and hit your head, even a minor bump can turn into a life-threatening situation. It’s not about how hard you fell-it’s about what’s happening inside your skull. Blood thinners, whether they’re warfarin, rivaroxaban, apixaban, or aspirin, make it harder for your blood to clot. That’s good for preventing strokes or clots, but it’s dangerous when trauma happens. A small bleed inside the brain can grow slowly over hours or even days, and by the time symptoms show up, it might be too late.
Why Even a Small Head Injury Matters
You might think, "I didn’t lose consciousness. I didn’t black out. It was just a slip on the bathroom floor." But for someone on anticoagulants, that’s not enough. Studies show that people taking blood thinners have 2 to 3 times higher risk of bleeding inside the skull after even minor head trauma compared to those not on these medications. The risk isn’t just from big falls-it’s from any impact to the head or neck. A stumble down a step, a bump against a doorframe, or even a fall from a standing position can cause a slow, silent bleed.
What makes this worse is that symptoms don’t always show up right away. You might feel fine for hours, then suddenly get dizzy, confused, or start vomiting. That’s because bleeding in the brain doesn’t always happen instantly. It can creep up over 24 to 72 hours. That’s why waiting to see if you "feel okay" is one of the biggest mistakes people make.
When to Go Straight to the ER
If you’re on blood thinners and hit your head, don’t wait. Don’t call your doctor and wait for an appointment. Go to the emergency room immediately if you have any of these:
- Any loss of consciousness-even for a few seconds
- Confusion, trouble speaking, or memory loss (especially about the fall)
- Headache that gets worse over time
- Nausea or vomiting more than once
- Dizziness, balance problems, or weakness on one side of the body
- Blurred vision, unequal pupils, or double vision
- Any visible injury to the head or neck
- Fall from a height (even just one step)
- Age 65 or older
These aren’t just suggestions-they’re hard rules in emergency medicine. The Washington State Department of Health and the American College of Emergency Physicians (ACEP) both say: if you’re on blood thinners and have any of these signs, get a CT scan right away. No exceptions. No "let’s wait and see."
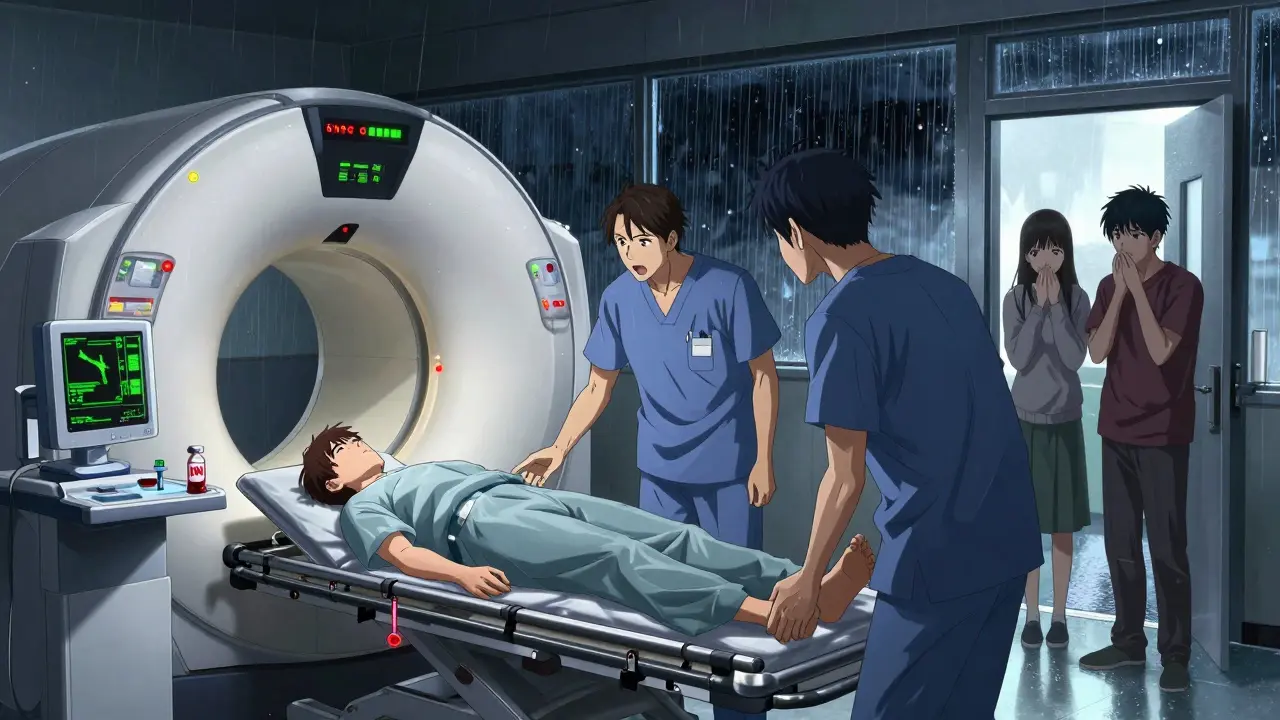
Why a CT Scan Is Non-Negotiable
The only way to see if there’s bleeding in the brain after a head injury is a non-contrast head CT scan. It’s fast, widely available, and highly accurate for detecting fresh bleeding. MRI might show more detail later, but in the emergency setting, CT is the gold standard because it’s quick and picks up acute bleeds better than anything else.
Here’s what happens in the ER: You’ll get a CT scan within minutes of arrival. The hospital will also run blood tests-specifically, a PT/INR test to check how well your blood clots. If you’re on warfarin, they’ll want to know your INR level. If it’s above 3.5, the risk of bleeding is much higher. If you’re on a DOAC like rivaroxaban or apixaban, they’ll check your kidney function and time since your last dose, because these drugs clear from your body faster than warfarin.
Some hospitals use special CT settings-0.5 mm to 1.25 mm "bone algorithm" images-to catch tiny skull fractures that might not show up on a regular scan. These fractures can be a sign of more serious internal damage, even if you feel okay.
What If the CT Scan Is Normal?
This is where things get tricky. A normal CT scan doesn’t mean you’re in the clear. About 0.5% to 1% of patients on blood thinners with a normal initial scan will develop a delayed bleed within 72 hours. That’s why you can’t just go home and hope for the best.
Some hospitals, like the University of Texas Health Science Center, require a 6-hour observation period after the injury-even with a normal CT. During that time, nurses will check your mental status, vital signs, and neurological function every hour. If you stay stable, you might be discharged with clear instructions. But if you develop any new symptoms-headache, nausea, drowsiness-you’ll get another CT scan right away.
Other places, like Johns Hopkins, recommend 24-hour observation for all anticoagulated patients, regardless of initial scan results. Why? Because delayed bleeding doesn’t always follow a predictable timeline. One patient in a 2024 study had a negative CT, was sent home, and suffered a major stroke three days later after stopping their rivaroxaban. That’s not a rare case-it’s a warning.
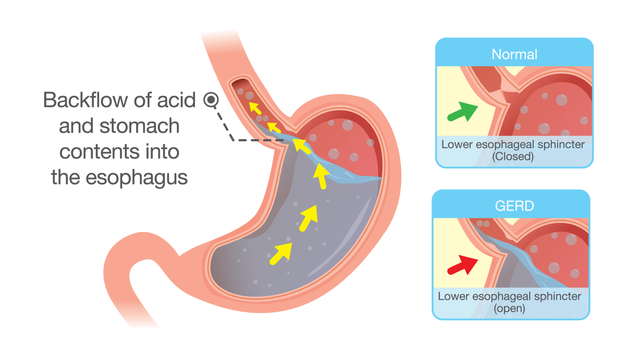
Don’t Stop Your Blood Thinners Without Help
Here’s a dangerous myth: "I hit my head. I should stop my blood thinner." Don’t do it. Stopping your anticoagulant suddenly can cause a clot-leading to a stroke, heart attack, or pulmonary embolism. The risk of stopping is often higher than the risk of a slow bleed.
If bleeding is found, doctors will decide whether to reverse the anticoagulant. For warfarin, they might give vitamin K or PCC (prothrombin complex concentrate). For DOACs like rivaroxaban, they might use idarucizumab (Praxbind). But this is never done on your own. It’s a decision made by an emergency physician, often with input from a hematologist or neurosurgeon.
Even if your CT is clean, never adjust your dose without talking to your doctor. The same 2024 study that showed delayed bleeds also found that patients who stopped their DOACs after a head injury were at higher risk of ischemic stroke.
What to Do After You Leave the Hospital
If you’re discharged, you’ll get written instructions. Read them. Then read them again. You should know exactly what symptoms mean you need to come back:
- Worsening headache
- Repeated vomiting
- Difficulty waking up or staying alert
- Slurred speech or weakness in arms or legs
- Seizure
- Confusion or memory loss that gets worse
Have someone stay with you for at least 24 hours. Don’t drive. Don’t drink alcohol. Don’t take any new medications-including over-the-counter painkillers like ibuprofen or naproxen-unless your doctor says it’s okay. These can interfere with your blood thinner or worsen bleeding.
Follow up with your primary care doctor or anticoagulation clinic within 48 hours. They’ll check your INR (if on warfarin), review your symptoms, and decide whether it’s safe to restart or adjust your medication.
Why the Canadian Rule Doesn’t Apply to You
You might have heard of the Canadian CT Head Rule-a tool doctors use to decide if someone with a head injury needs a scan. It’s great for healthy people. But it was never tested on people taking blood thinners. In fact, the creators say it’s unsafe to use on anticoagulated patients. One study found that using this rule on people like you could miss up to 15% of brain bleeds.
That’s why guidelines from the American College of Surgeons and ACEP specifically say: don’t rely on standard head injury rules if you’re on blood thinners. You need a higher level of caution.
What’s Changing in 2026
Doctors are starting to look beyond CT scans. The FDA approved a blood test in 2018 called the Banyan Brain Trauma Indicator, which measures two proteins (UCH-L1 and GFAP) that leak into the blood after brain injury. It’s not perfect, but it might help identify patients who don’t need a CT scan at all. Right now, it’s mostly used for patients with mild symptoms and normal mental status-but research is ongoing.
Researchers are also working on a new version of the Canadian rule specifically for patients on DOACs. That could lead to more personalized care by 2025-2026. But until then, the safest rule is simple: if you’re on blood thinners and hit your head, get a CT scan. No ifs, ands, or buts.
Bottom Line
Head injuries on blood thinners aren’t like regular head injuries. They’re more dangerous, more unpredictable, and require immediate action. Don’t downplay a bump. Don’t wait for symptoms. Don’t assume you’re fine because you didn’t black out. The brain doesn’t always scream before it bleeds.
When in doubt, go to the ER. Get the CT scan. Get the blood test. Don’t stop your meds. Follow up. Your life depends on acting fast-not waiting.




Mina Murray
January 7, 2026 AT 10:42Let me tell you something nobody else will: the FDA approved that Banyan test in 2018, but hospitals still won’t use it because they make more money off CT scans. Big Pharma and imaging centers have a quiet agreement-you get the scan, we get the profit. I’ve seen it. A friend got a normal CT, got sent home, and bled out three days later. The hospital refused to re-scan because ‘it wasn’t protocol.’ Protocol is a money trap. They’d rather you die quietly than admit their system is broken.
Christine Joy Chicano
January 9, 2026 AT 09:03There’s something haunting about how silently brain bleeds creep in-like a tide rising under a calm shore. You don’t feel the water until you’re ankle-deep, then waist-deep, then gasping. And yet, we treat head trauma on anticoagulants like it’s a minor inconvenience. The science is clear: even a stumble on a rug can be a silent death sentence. I wish more people understood that ‘feeling fine’ is the most dangerous lie the body tells.
Adam Gainski
January 10, 2026 AT 07:09Great breakdown. I’m a paramedic and I can’t tell you how many times I’ve had patients insist they’re fine after a fall, especially older folks on warfarin. One guy fell off his porch ladder, said he didn’t need help, and drove himself to the store. Two hours later, his daughter found him slumped in the cereal aisle. CT showed a subdural hematoma the size of a walnut. He’s fine now, but only because we got him in time. Please, if you’re on blood thinners-don’t be brave. Be smart. Get scanned.
Elen Pihlap
January 11, 2026 AT 05:37But what if you don’t have insurance? What if you’re just one missed paycheck away from homelessness? Do you just die because you can’t afford a CT? This whole system is rigged. I saw my cousin wait 14 hours in the ER because they said ‘it’s not an emergency unless you’re screaming.’ She was on rivaroxaban. She died in the parking lot. No one even apologized.
Poppy Newman
January 13, 2026 AT 02:40This is so important 😭 I’m on apixaban for AFib and I just slipped on ice last week. I went straight to urgent care. They were like ‘eh, you’re fine.’ I said ‘nope, CT or I’m walking out and going to ER.’ They did it. Nothing. But I slept with my daughter next to me for 48 hours. Better safe than sorry 💪🫶
Jessie Ann Lambrecht
January 14, 2026 AT 10:36STOP WAITING. STOP RATIONALIZING. STOP THINKING YOU’RE FINE. This isn’t a suggestion-it’s a lifeline. I’ve lost two friends to delayed bleeds after ‘minor’ head injuries. One was 52, healthy, active. She hit her head on a cabinet door. Thought she was fine. Watched TV. Went to bed. Never woke up. Her husband found her with a bruise the size of a quarter. That’s it. A quarter. That’s all it took. If you’re on blood thinners, your brain is a ticking bomb. And you? You’re the only one holding the detonator. Don’t let it go off.
Vince Nairn
January 15, 2026 AT 06:02Kyle King
January 15, 2026 AT 22:38They’re lying. The whole thing. CT scans don’t catch delayed bleeds. That’s why they invented the ‘6-hour observation’ loophole. They don’t want to admit the truth: blood thinners are poison and the drugs are designed to kill slowly so you keep buying them. I read a whistleblower report from a lab tech who said they were told to downplay small bleeds to avoid ‘alarm fatigue.’ They’re not saving lives-they’re selling fear and scans. And don’t even get me started on Praxbind. That’s a billion-dollar drug for a problem they created.