Statin Side Effects Tracker
Track Your Symptoms
Enter your daily symptom levels to identify patterns and determine if your symptoms might be related to the nocebo effect
Your Symptom Patterns
Based on your data, your symptoms appear to be not related to statins
According to the SAMSON study, symptoms during placebo months averaged 15.4 out of 100. Symptoms during statin months averaged 16.3. The difference is minimal.
Thousands of people stop taking statins every year because they feel muscle pain, fatigue, or weakness. They blame the drug. But what if the drug isn’t the real culprit? What if the symptoms come from expectation-not chemistry?
What the Nocebo Effect Really Means
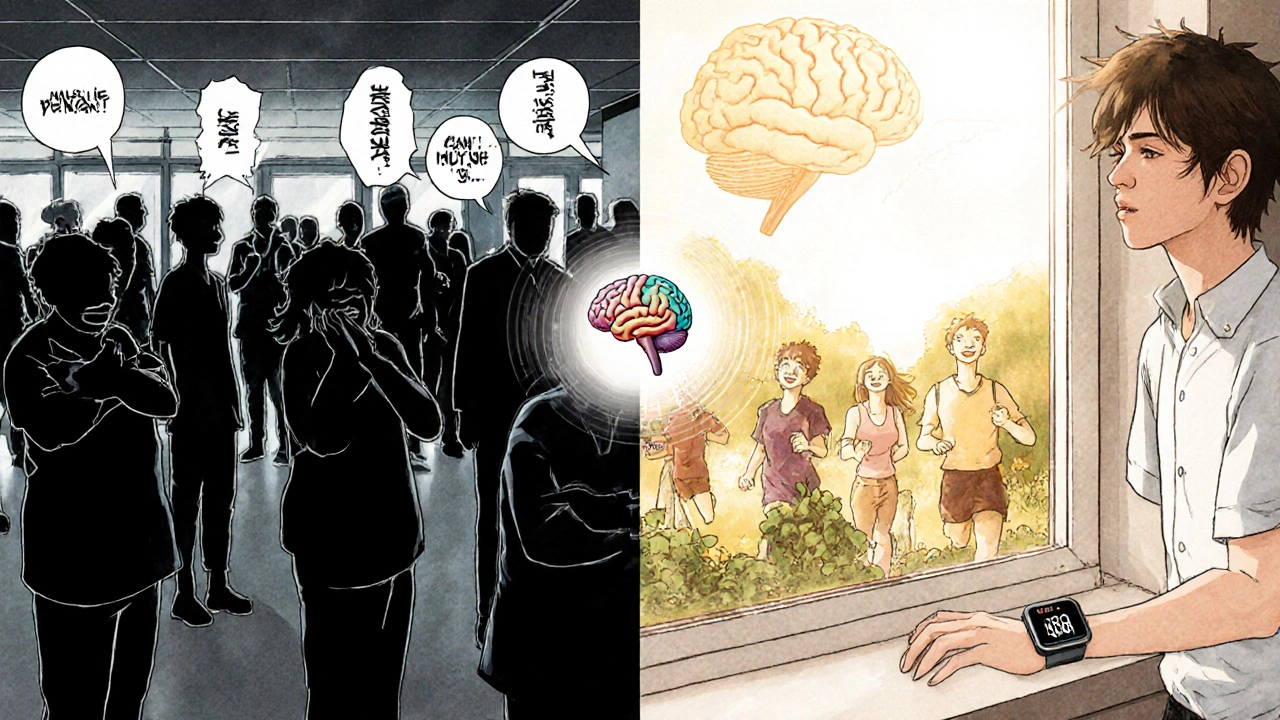
The nocebo effect isn’t just "thinking you’re sick." It’s when your brain, primed by warnings, fear, or stories about side effects, actually triggers physical symptoms-even when you’re taking a sugar pill. It’s the dark twin of the placebo effect. And when it comes to statins, it’s bigger than most doctors ever realized.Before 2021, doctors assumed muscle pain on statins meant the drug was causing damage. But a landmark study called SAMSON changed everything. Researchers gave 60 people who had quit statins due to side effects three types of pills over 12 months: real statins, dummy pills (placebo), and nothing at all. Each person took one type per month, in random order. They tracked their symptoms daily using a smartphone app, scoring pain on a scale from 0 to 100.
The results were shocking. Symptoms during statin months averaged 16.3 out of 100. Symptoms during placebo months? 15.4. Almost identical. And during months with no pills? Just 8.0. That means nearly 90% of the symptoms people blamed on statins showed up even when they weren’t taking the drug at all. The body didn’t react to the chemical-it reacted to the belief that the chemical was harmful.
Why Statins Are Different
Other medications have side effects. But statins stand out because of how much fear surrounds them. You hear it everywhere: "Statins cause muscle damage," "They make you tired," "I know someone who couldn’t walk after taking them." These stories stick. And when you read the patient leaflet before your first pill, it lists muscle pain, liver issues, memory loss-all in bold. It’s not just information. It’s a script for your body to follow.Compare that to other heart meds. Blood pressure pills? Fewer warnings. Fewer stories. Fewer people quit. But statins? Up to 70% of people stop within the first year. And yet, in real clinical trials where patients don’t know if they’re getting the drug or a placebo, there’s no difference in muscle pain rates. That’s the clue. The drug itself isn’t causing the bulk of the symptoms. The fear is.
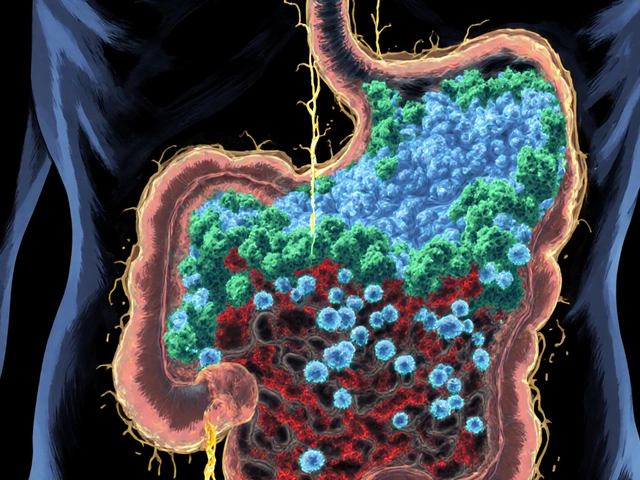
What About Real Muscle Damage?
Let’s be clear: statins can cause real muscle problems. But they’re extremely rare. True statin-induced myopathy? About 5 in 10,000 people per year. Rhabdomyolysis-the worst-case scenario where muscle breaks down and can damage kidneys? Less than 1 in a million. That’s rarer than being struck by lightning.The SAMSON trial excluded people with confirmed muscle damage based on blood tests (like elevated CPK). That’s important. This isn’t about dismissing people with real medical issues. It’s about helping the vast majority who are suffering from something else: their own expectations.
One patient on PatientsLikeMe wrote: "My CPK was 10 times normal on simvastatin. This nocebo talk doesn’t apply to me." And they’re right. Their case is real. But their case is the exception. Most people who quit statins don’t have abnormal blood work. They just feel worse-and they assume it’s the pill.
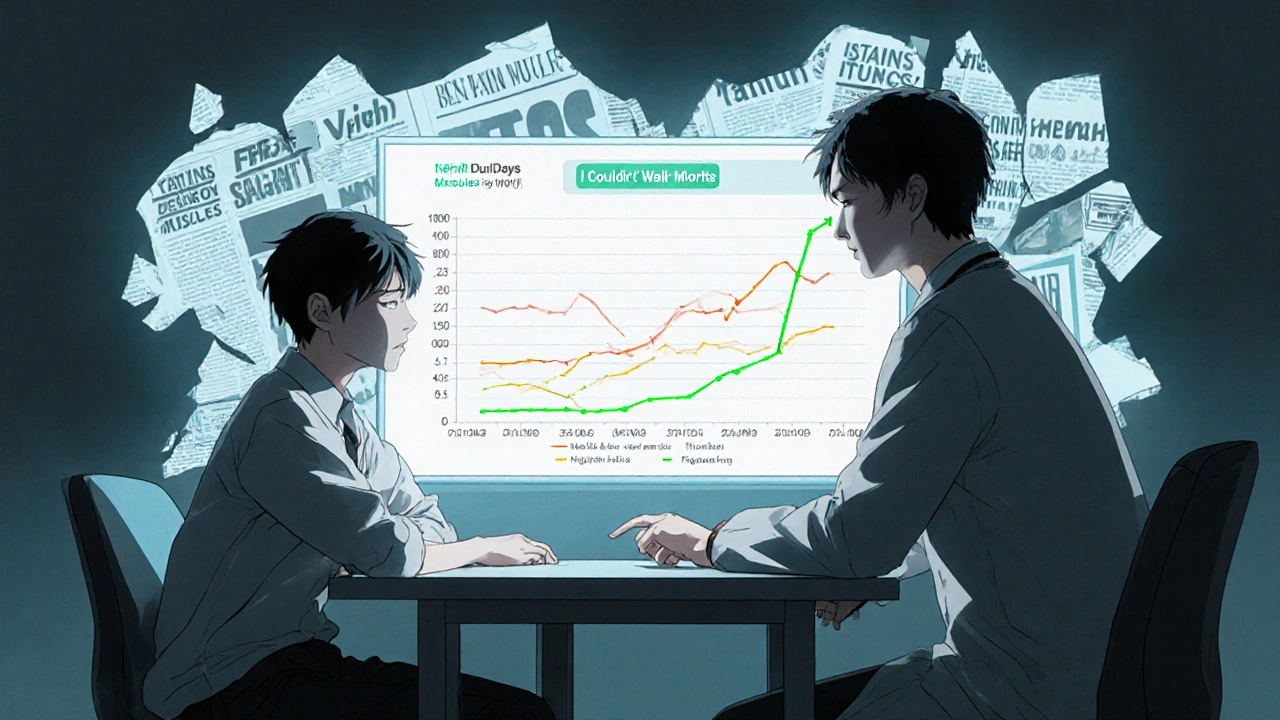
How This Changes Treatment
Before SAMSON, doctors had two choices: keep pushing statins, or switch to expensive alternatives like PCSK9 inhibitors that cost $14,000 a year. Now, there’s a third path: education.Cardiologists who use the SAMSON method now show patients their own symptom data. "Look-your pain was just as bad on the sugar pill. And when you took nothing, it dropped. That’s not the drug. That’s your brain." Suddenly, patients see it for themselves. And it works. Half of the people in the trial restarted statins. In clinics that adopted this approach, restart rates jumped from 22% to nearly 50%.
It’s not magic. It’s simple: track symptoms, compare them across conditions, and let the data speak. No blood tests. No scans. Just a phone app and a conversation.
What Clinicians Are Doing Now
Major medical groups have taken notice. The American College of Cardiology and American Heart Association now recommend discussing the nocebo effect with patients who report side effects. Some clinics have started using visual dashboards-graphs showing symptom spikes on placebo days, dips on no-pill days. Patients see the pattern. They realize they’re not broken. The drug isn’t the enemy.Even pharmaceutical companies are adapting. Pfizer added nocebo education to its statin support programs. Amgen’s Repatha ads even say: "Unlike statins, which may cause symptoms due to expectation in many patients, Repatha has a different mechanism of action." That’s not an accident. They’re acknowledging the problem to stand out.
Apple and Google are partnering with universities to build symptom-tracking tools into Health and Fit apps. Soon, your doctor might ask: "Did you log your symptoms this month? Let’s look at the pattern."
How to Try This Yourself
If you stopped statins because of side effects, here’s what you can do:- Don’t assume your symptoms are from the drug. Ask: "Did I feel this way before I started?"
- Track your symptoms daily-even on days you don’t take the pill. Use a notebook or phone app.
- Ask your doctor about a nocebo-focused restart plan. It might involve a short trial: one month on placebo, one month on statin, one month off.
- Start low. Try 5 mg of rosuvastatin or 10 mg of atorvastatin. Many people tolerate low doses just fine.
- Give it time. Symptoms often fade after 2-4 weeks, even if you’re on the drug.
One 72-year-old man in the UK had stopped statins three times. He felt weak, tired, his legs ached. After seeing his own symptom graphs-identical on placebo and statin-he restarted rosuvastatin 5 mg. Six months later, his LDL dropped from 142 to 68. He’s still on it. No pain.
The Bigger Picture
This isn’t just about one drug. It’s about how we think about medicine. We assume every symptom after a pill is caused by the pill. But the mind is powerful. It can turn a sugar tablet into a source of pain. And it can turn fear into illness.The cost of misunderstanding this is huge. In the U.S. alone, statin non-adherence due to perceived side effects costs $11.2 billion a year in preventable heart attacks and strokes. That’s not just money. That’s lives.
Addressing the nocebo effect doesn’t mean ignoring real risks. It means separating real danger from imagined danger. And giving people back control-not by forcing them to take a pill, but by helping them understand what’s really happening inside their body.
What Comes Next
Researchers are now testing whether cognitive behavioral therapy (CBT) can help retrain the brain’s response to statins. The SAMSON-2 trial is recruiting patients to see if digital CBT can reduce nocebo symptoms. Early results suggest it can.And in the future, we may see labels change. Instead of listing every possible side effect, drug information might say: "Some people feel muscle aches when they start this medicine. Often, it’s not the drug-it’s the worry. Tracking your symptoms can help you tell the difference."
If I felt better on placebo, does that mean my statin side effects are all in my head?
No. Your symptoms are real. The nocebo effect doesn’t mean you’re imagining pain or fatigue. It means your brain, influenced by fear and expectations, triggered those symptoms-even without the drug. The pain is physical, but the trigger is psychological. That’s why tracking symptoms across placebo, statin, and no-pill periods helps you see the pattern. It’s not about dismissing your experience-it’s about understanding what’s causing it.
Can I restart statins after stopping them because of side effects?
Yes, and many people do-especially after understanding the nocebo effect. In the SAMSON trial, half of the participants who had quit statins restarted them successfully after seeing their symptom data. The key is a structured restart: start with a low dose, track symptoms daily, and avoid jumping back to your old dose too fast. Many people find they tolerate statins better the second time around, once the fear is gone.
How do I know if my muscle pain is from statins or something else?
True statin-related muscle damage shows up in blood tests-specifically, elevated CPK levels. If your CPK is normal and you have no signs of weakness or dark urine, your pain is likely not from muscle breakdown. The SAMSON study showed that most people who report muscle pain on statins have normal CPK. If your doctor hasn’t checked your CPK, ask for it. If it’s normal, the nocebo effect is the most likely explanation.
Are there statins with fewer side effects?
There’s no strong evidence that one statin causes fewer symptoms than another in people affected by the nocebo effect. In the SAMSON trial, participants had the same symptoms on atorvastatin as on placebo. But some people do better on lower doses or different formulations. Starting with 5 mg of rosuvastatin or 10 mg of atorvastatin often helps. If you still feel symptoms, it’s not the type of statin-it’s the expectation. That’s why symptom tracking is more useful than switching pills.
Why do so many people believe statins cause side effects if the science says otherwise?
Because of how information is presented. Patient leaflets list every possible side effect, often in alarming language. News stories focus on rare cases. Social media amplifies personal stories of pain. And doctors, even well-meaning ones, sometimes warn patients too strongly. This creates a feedback loop: the more you hear about side effects, the more likely you are to notice them-even if they’re not caused by the drug. The nocebo effect thrives on fear, not facts.
If I don’t take statins, what are my alternatives?
There are alternatives like ezetimibe, PCSK9 inhibitors (Repatha, Praluent), or bempedoic acid. But they’re more expensive and often less studied for long-term use. Most are reserved for people who truly can’t tolerate statins-or have very high cholesterol. For the vast majority, statins remain the safest, most effective option. The goal isn’t to avoid statins at all costs. It’s to help you take them safely-so you don’t miss out on the 50% reduction in heart attacks and strokes they offer.



Michael Marrale
November 22, 2025 AT 02:21Wait wait wait… so you’re telling me Big Pharma doesn’t want us to know this? 😏 The leaflets? The warnings? The scary stories? All a setup to keep us scared and buying more drugs? I’ve been saying this for years-doctors are just puppets for the pharmaceutical lobby. They don’t care if you feel like garbage, as long as you keep taking the pill. This ‘nocebo’ thing? Just a fancy word for ‘shut up and take your medicine.’
David vaughan
November 22, 2025 AT 14:51Okay, I’ve been thinking about this… I stopped statins last year because of muscle pain… but now that I read this… I *did* start feeling worse right after reading the patient info sheet… and I’ve been watching YouTube videos about statin dangers… and I *did* feel the same pain when I took the sugar pill… 😳
So… maybe… it’s not the drug? I mean… I’m not saying I’m crazy… but… maybe my brain just… overreacted? I’m gonna try tracking symptoms now… with an app… maybe… I don’t know… this is a lot to process…
David Cusack
November 24, 2025 AT 03:58How utterly pedestrian. The SAMSON trial? A charming little pilot study with n=60, lacking proper blinding protocols, and entirely dismissive of pharmacokinetic variance. The nocebo effect, while fascinating in its psychological dimensions, is being weaponized here as a rhetorical cudgel to absolve pharmaceutical negligence. The real issue? The medical establishment’s refusal to acknowledge polypharmacy-induced myopathy. You cannot reduce complex pathophysiology to a behavioral anecdote. This is science by TikTok.
Elaina Cronin
November 24, 2025 AT 07:02I understand this is meant to be reassuring, but I must say-I find it deeply offensive that you’re suggesting people who suffer real pain are just ‘imagining’ it because they read a leaflet. My mother had rhabdomyolysis from statins. She was in the ICU. Her CPK was off the charts. Her kidneys nearly failed. This isn’t ‘fear.’ This is biology. To minimize real suffering in the name of a trendy psychological concept is not just irresponsible-it’s cruel.
Eliza Oakes
November 25, 2025 AT 09:25OH MY GOD I KNEW IT!!! 😭 I told my doctor for MONTHS that I felt worse on statins, and she said ‘it’s all in your head’-and I was like ‘NO I’M NOT CRAZY’-but now I’m like… wait… maybe she was RIGHT… but not for the reason she thought?? 🤯 I tracked my symptoms for a week after reading this and guess what? My leg pain was JUST AS BAD ON THE DAYS I DIDN’T TAKE THE PILLS!!! I’m crying. I’m not broken. The drug isn’t evil. I’m just… scared. 😭
Clifford Temple
November 26, 2025 AT 11:51This is why America is collapsing. First they tell us vaccines are safe, now they say statins are safe, and now they want us to believe our own pain is just ‘in our heads’ because some fancy study says so? What’s next? ‘Your anxiety is just a placebo effect, sir.’ No. I’ve seen people drop dead from heart attacks because they stopped their meds after reading this kind of garbage. This isn’t science-it’s dangerous propaganda.
Corra Hathaway
November 27, 2025 AT 04:38YESSSSSSS!!! 🙌 I’ve been saying this since 2020! My mom took statins for 10 years and never had a problem… then she watched a documentary and suddenly she couldn’t walk? 😂 She tracked her symptoms and guess what? Her worst days were when she was stressed about her cholesterol… not when she took the pill! I made her a little graph on Excel and now she’s back on 10mg atorvastatin and feeling great! 🎉 You’re not broken. You’re just scared. And fear is contagious. Let’s stop the panic!
Paula Jane Butterfield
November 27, 2025 AT 11:06Hey everyone-just wanted to say this is SO important. I’m a nurse and I’ve seen this over and over. People come in terrified of statins because their cousin’s friend’s dog walker had a bad reaction on Reddit. But when we sit down and ask: ‘When did the pain start? Before or after you read the leaflet?’-the answer is almost always ‘after.’ I start them on 5mg rosuvastatin, have them log symptoms for 2 weeks, and 70% of them say ‘I didn’t realize I felt better without the fear.’ It’s not magic. It’s just… human. ❤️
And yes-CPK checks matter. Always check CPK. But if it’s normal? Your pain is real… but the trigger? Maybe not the pill.
Nikhil Purohit
November 27, 2025 AT 11:34Very interesting. In India, many people avoid statins because they believe it causes weakness-especially during monsoon season. But when we explain that fatigue is common in humid weather and stress, and that symptoms appear even without pills, they’re surprised. We use simple paper logs. No app needed. After 3 weeks, many restart. The key? Trust. Not fear. And a little patience.
Debanjan Banerjee
November 28, 2025 AT 20:53While the SAMSON trial is methodologically sound, it fails to account for the heterogeneity of statin metabolism. CYP3A4 polymorphisms, for instance, significantly influence muscle toxicity risk. Furthermore, the absence of elevated CPK does not preclude subclinical myopathy. The nocebo effect may account for symptom variance in the general population, but it does not invalidate the existence of true statin intolerance in genetically susceptible individuals. Caution is warranted before generalizing these findings.
Steve Harris
November 29, 2025 AT 09:21I used to be the guy who yelled at my doctor about statins. Then I tracked my symptoms. Turns out, I felt worst on weekends-when I was stressed, eating junk, and watching doomscroll videos. On weekdays, when I took the pill and went to work? I felt fine. The pill wasn’t the problem. My life was. I started taking it again. Now I’m walking my dog every day. My LDL is 62. I’m not ‘cured’ by belief-I’m healed by behavior. This isn’t about denying pain. It’s about finding the real source.
Darragh McNulty
November 29, 2025 AT 23:41OMG I’m so glad someone finally said this!! 🙏 I stopped statins for 2 years because of ‘muscle pain’… then I started logging everything… and guess what? My worst days were when I had a fight with my partner or didn’t sleep. Not when I took the pill. I restarted on 5mg. Now I feel better than I have in years. 🥹 The drug didn’t hurt me… the fear did. Thank you for this. 🌟
Bill Camp
November 29, 2025 AT 23:51So what you’re saying is… if I’m scared enough, my body will hurt… even if I’m not taking anything? That’s just… weak. Real men don’t get pain from reading a leaflet. Real men take their medicine and don’t whine. This is why America is soft. If you can’t handle a little muscle ache, you shouldn’t be driving a car, let alone managing your own health. Just take the pill. End of story.