Foot pain can hijack your day, and plantar fasciitis is one of the most common culprits. The big question on many people’s radar is whether aspirin can calm the ache and get you back on your feet. Below you’ll find a plain‑spoken walk‑through of how aspirin works, what plantar fasciitis actually is, and what you should consider before reaching for that bottle.
How aspirin works in the body
When you first meet Aspirin is a non‑steroidal anti‑inflammatory drug (NSAID) that reduces pain, fever and inflammation by blocking the enzyme cyclooxygenase (COX), you’re looking at a chemistry shortcut that stops prostaglandins from forming. Prostaglandins are tiny messengers that tell nerves to feel pain and make blood vessels swell. By cutting the COX pathway, aspirin dulls the pain signal and eases swelling.
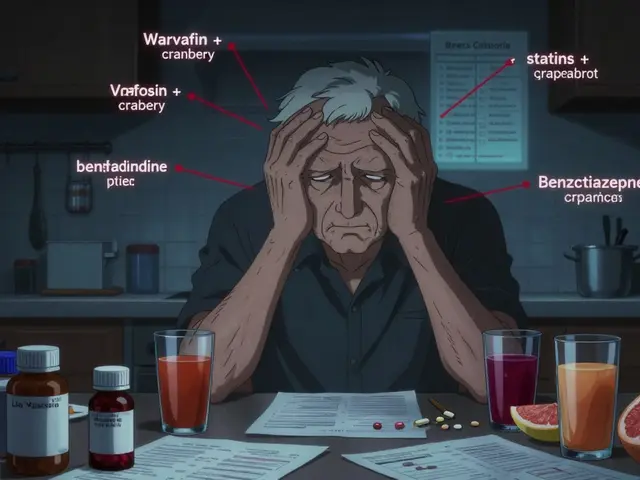
Unlike many newer NSAIDs, aspirin also thins the blood a bit, which can be helpful for heart health but adds a caution flag for people with bleeding disorders or who are on anticoagulants.
What is plantar fasciitis?
Plantar fasciitis is an inflammation of the plantar fascia, a thick band of connective tissue that runs from the heel bone to the toes and supports the arch of the foot. The condition usually shows up as a sharp sting in the heel first thing in the morning or after a long period of rest.
Key risk factors include tight calf muscles, high‑arched or flat feet, excessive running, and shoes that lack proper arch support. Over time, the fascia can develop micro‑tears, leading to chronic inflammation and pain.
Can aspirin relieve plantar fasciitis pain?
Because the core problem is inflammation, aspirin’s anti‑inflammatory action can provide modest relief, especially for mild cases. A typical over‑the‑counter dose (300-500 mg every 4-6 hours, not exceeding 3 g per day) may soften the ache enough to allow you to stretch and move without aggravating the tissue.
However, aspirin is not a cure. It reduces the symptom of pain and swelling but does not address the underlying tightness or biomechanical stress that caused the fasciitis in the first place. For many patients, aspirin works best as a short‑term bridge while they adopt other treatments.

Comparing aspirin with other NSAIDs
When it comes to foot‑related inflammation, several NSAIDs vie for the top spot. Below is a quick snapshot of how aspirin stacks up against ibuprofen and naproxen.
| Drug | Typical Oral Dose for Pain | Onset of Relief | Duration of Action | Common Side Effects |
|---|---|---|---|---|
| Aspirin | 300-500 mg every 4‑6 h (max 3 g/day) | 30-60 min | 4‑6 h | Stomach irritation, bleeding risk |
| Ibuprofen | 200-400 mg every 4‑6 h (max 1.2 g/day OTC) | 20-30 min | 4‑6 h | Heartburn, kidney strain |
| Naproxen | 220‑250 mg every 8‑12 h (max 660 mg/day OTC) | 30-45 min | 8‑12 h | GI upset, increased blood pressure |
All three drugs hit the COX enzymes, but ibuprofen tends to act a bit quicker, while naproxen sticks around longer. Aspirin’s extra blood‑thinning effect can be a pro for heart‑health‑aware folks, but it also raises the stakes for stomach bleeding, especially if you take it on an empty stomach.
Non‑medication strategies that complement aspirin
Relying on a pill alone is like trying to fix a leaky roof with tape. Here are evidence‑based moves that work hand‑in‑hand with aspirin:
- Stretching exercises are targeted motions that lengthen the calf muscles and plantar fascia, reducing tensile stress on the heel. A popular routine is the “wall stretch”: stand an arm’s length from a wall, place both hands on it, step one foot back, keep the heel down, and hold for 30 seconds. Repeat three times per leg.
- Orthotic insoles are custom or over‑the‑counter shoe inserts that provide arch support and redistribute pressure across the foot. Even a simple arch‑supporting insole can cut heel strain by up to 30 %.
- Physical therapy is a structured program of manual techniques, exercises, and education designed to improve foot biomechanics. A therapist can teach you how to walk with a shorter stride and stronger foot muscles.
- Cold therapy is application of ice or a cold pack to the heel for 15‑20 minutes after activity, which curbs swelling. Consistency matters - aim for three sessions a day during flare‑ups.
- Corticosteroid injections, while effective for severe inflammation, carry a risk of fascia rupture and are typically reserved for cases that don’t improve after 6‑8 weeks of conservative care.
When you pair these measures with a sensible aspirin regimen, many people notice a quicker drop in pain intensity and can progress to full‑strength activity sooner.

Safety tips and red flags
Before you pop that aspirin, ask yourself these quick checks:
- Do you have a history of stomach ulcers, bleeding disorders, or are you on blood thinners? If yes, skip aspirin and talk to a doctor.
- Are you pregnant or nursing? Aspirin is generally discouraged in the third trimester.
- Is your pain lingering beyond 3 months despite NSAIDs, stretching and orthotics? That could signal a heel spur, nerve involvement, or another condition that needs imaging.
If any of these apply, schedule a visit with a podiatrist or physiotherapist. Early diagnosis helps you avoid chronic heel pain that can become a lifelong nuisance.
Putting it all together: a simple daily plan
Here’s a no‑frills routine you can start tomorrow:
- Morning: 300 mg aspirin with a small breakfast, followed by a 5‑minute calf stretch.
- Mid‑day: Slip fitted orthotic insoles into your work shoes, take a 2‑minute walk break every hour to keep the fascia from stiffening.
- Evening: Ice the heel for 15 minutes, do the wall stretch again, and if needed, take a second 300 mg aspirin dose (watch the daily total).
Track your pain on a 0‑10 scale for two weeks. If scores drop by at least two points and you can walk pain‑free for 20 minutes, you’ve found a workable combo. If not, consider swapping aspirin for ibuprofen or seeking professional guidance.
Frequently Asked Questions
Can aspirin cure plantar fasciitis?
No. Aspirin reduces pain and swelling temporarily but does not heal the torn fascia. It works best alongside stretching, orthotics and other conservative measures.
How often can I take aspirin for foot pain?
The OTC limit is 3 g per day (about six 500 mg tablets). Space doses at least four hours apart and avoid taking it on an empty stomach.
Is aspirin safe for long‑term use?
Long‑term daily aspirin can increase the risk of gastrointestinal bleeding and ulcers. If you need more than a few weeks of relief, switch to another NSAID or discuss alternative therapies with a healthcare professional.
Should I combine aspirin with other treatments?
Yes. Combining aspirin with stretching, proper footwear, and cold therapy often gives faster relief than the pill alone. Just avoid taking multiple NSAIDs at the same time to prevent overdose.
When is it time to see a doctor for plantar fasciitis?
If pain persists beyond three months, worsens despite conservative care, or you notice numbness, bruising, or a sudden sharp burst of pain, schedule an appointment. Imaging may be needed to rule out a heel spur or stress fracture.
Bottom line: aspirin can be a handy, low‑cost tool in the early stages of plantar fasciitis, but it’s not a stand‑alone cure. Pair it with smart stretching, good shoes and a watchful eye on side effects, and you’ll give your heels a solid chance to heal.




Monika Pardon
October 26, 2025 AT 14:13Ah, the age‑old secret that the pharmaceutical industry doesn’t want you to know: aspirin is just a glorified placebo for heel pain, wrapped in a veneer of “science”. Of course, the conspiratorial elites would have you believe that a cheap tablet can replace proper biomechanics. Yet, your heel still screams in the morning, doesn’t it? In short, aspirin may dull the ache, but it won’t solve the underlying structural issues.
Rhea Lesandra
November 1, 2025 AT 06:13Hey folks, great thread! Let’s break this down so everyone feels empowered to tackle plantar fasciitis head‑on. First off, aspirin can be a handy stop‑gap, but think of it as a band‑aid rather than a cure. Pair that with consistent calf and fascia stretches-spend a few minutes each morning and evening, and you’ll see the tension melt away. Invest in supportive shoes or orthotic inserts; your foot architecture will thank you. Remember to stay hydrated and give your body the nutrients it needs to repair tissue. If you keep the routine consistent, you’ll likely notice a significant drop in pain within two weeks. Keep sharing your progress, and we’ll all celebrate the wins together!
Kasey Marshall
November 6, 2025 AT 22:13Aspirin works by inhibiting COX enzymes reducing prostaglandin synthesis which lowers inflammation and pain it’s useful for mild flare‑ups but should be combined with stretching and proper arch support for lasting relief
Dave Sykes
November 12, 2025 AT 14:13Listen up, if you’re relying solely on a pill you’re missing the bulk of the solution. Get your feet into shoes that actually support the arch, and schedule a quick stretch routine after every break. Make sure you’re taking aspirin with food to protect your stomach-don’t be reckless. Consistency beats occasional medication every single time. Keep pushing, your heels will thank you.
Erin Leach
November 18, 2025 AT 06:13I hear you-I’ve been there, wincing with that sharp heel sting first thing in the morning. It’s frustrating when a simple over‑the‑counter tablet seems like the only thing that offers relief. Try pairing the aspirin with gentle calf stretches and a supportive insole; many people find that the combination eases the pain more sustainably. Also, give yourself permission to rest when needed, your body knows what it needs. You’re not alone in this, and taking a balanced approach will get you back on your feet.
Erik Redli
November 23, 2025 AT 22:13Alright, let’s cut the nonsense-aspirin is not some miracle cure and the hype around it is pure marketing fluff. You think popping a cheap tablet will magically repair torn fascia? No way. The real issue is that most people ignore biomechanical fundamentals and blame a pill for everything. Sure, aspirin can dull the pain for a few hours, but as soon as it wears off the inflammation resurfaces, often worse. Why do we keep feeding this pharma‑driven narrative when evidence points to stretching, orthotics, and proper footwear as the true game‑changers? You’ll waste money on endless bottles while the underlying problem festers. Moreover, chronic aspirin use opens the door to gastrointestinal bleeding, ulcers, and even kidney strain-slowly turning a foot problem into a systemic health crisis. And let’s not forget the blood‑thinning effect; you could end up with a nasty bleed from a simple stubbed toe. The bottom line is that aspirin is a temporary band‑aid, not a fix, and treating it as such is a disservice to anyone serious about recovery. If you’re looking for lasting relief, ditch the pill‑first mentality and invest in a proper rehab protocol. That means daily calf stretches, night‑time ice packs, and shoes that actually support your arch. Consult a physiotherapist who can tailor a program; don’t let a pharmacist’s sales pitch dictate your health plan. Remember, the only thing you’re truly purchasing with aspirin is a false sense of security while the real work remains undone. So stop the pill‑popping parade and start treating the root cause.
Jay Campbell
November 29, 2025 AT 14:13Stretching daily really does make a difference.
Jacqui Bryant
December 5, 2025 AT 06:13Give your feet a break, wear comfy shoes and do the wall stretch each morning; it helps keep the pain from coming back.
Paul Luxford
December 10, 2025 AT 22:13It’s important to monitor pain levels and adjust the routine if you notice any worsening symptoms; consistency is key.
Nic Floyd
December 16, 2025 AT 14:13From a biomechanical standpoint the viscoelastic properties of the plantar fascia benefit from cyclic loading modulation via low‑impact activities such as swimming or cycling 🏊♂️ the anti‑inflammatory cascade triggered by NSAIDs like aspirin is transient whereas structured proprioceptive training augments tissue remodeling 🦶 therefore integrating periodized exercise protocols yields superior outcomes 📈
Johnae Council
December 22, 2025 AT 06:13Honestly, this “everything’s fine with a couple of pills” attitude is the worst kind of lazy health advice. People read the headline, grab a bottle, and think they’ve solved the problem while the fascia keeps tearing apart. You’re basically telling yourself a story that works in the short term but burns you out later. The article misses the fact that many of these “quick fixes” just mask the pain and let the damage accumulate. If you actually care about healing, get off the aspirin couch and start treating the root cause.
Manoj Kumar
December 27, 2025 AT 22:13Ah, the grand illusion that a tiny tablet can outsmart centuries of evolutionary design-how delightfully naive. One might argue that the universe itself is a giant aspirin, dulling the sting of existence, yet even the cosmos respects the law of cause and effect. So while you pop the aspirin, remember that the fascia’s rebellion is a reminder that shortcuts rarely honor true balance. Embrace the grind of stretches and proper shoes, and perhaps you’ll find a deeper sense of harmony beyond the fleeting buzz of a pill.
Hershel Lilly
January 2, 2026 AT 14:13I’m curious how many people have tried combining ice therapy with aspirin and noticed a measurable drop in pain scores; any data would be helpful.