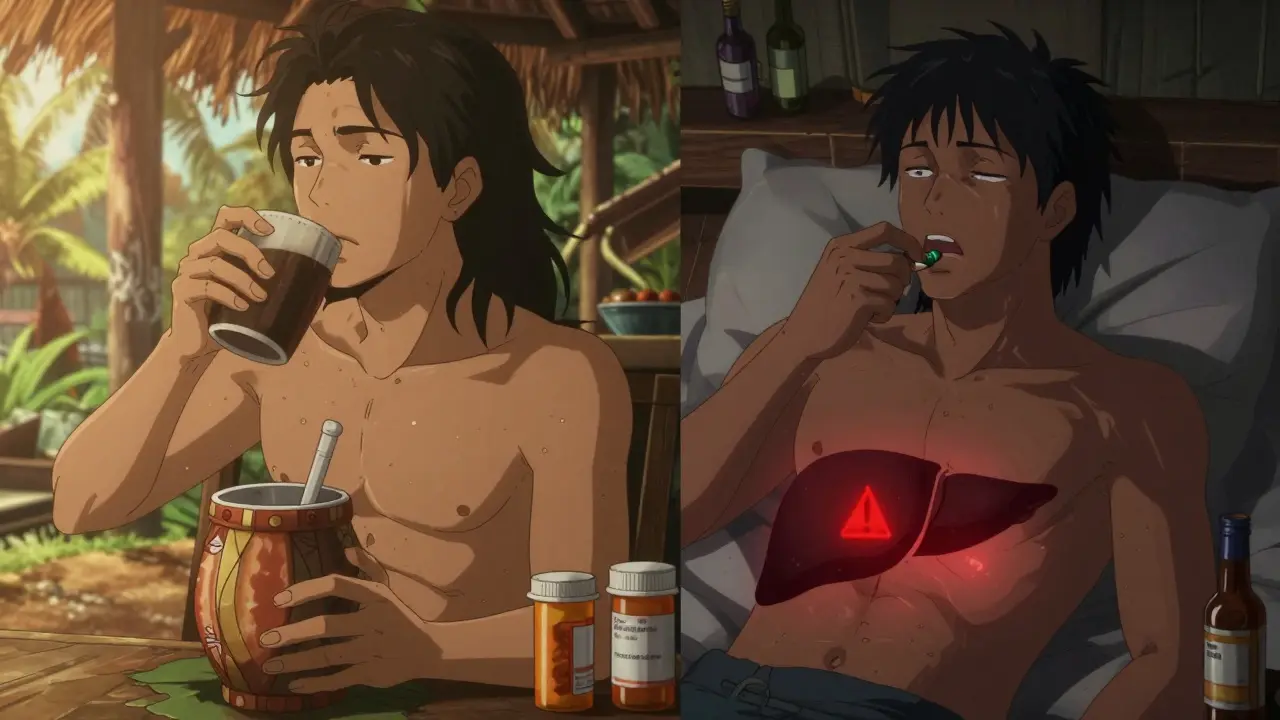
If you’re taking medication for anxiety, sleep, or pain-and you also use kava-you could be putting your liver at risk without even realizing it. Kava, a plant-based remedy popular for calming nerves, isn’t just another herbal supplement. When mixed with sedatives like benzodiazepines, sleep aids, or even alcohol, it doesn’t just make you drowsy. It can shut down your liver’s ability to process drugs, leading to serious, sometimes life-threatening damage.
How Kava Works (And Why It’s Dangerous With Medications)
Kava comes from the roots of Piper methysticum, a plant used for centuries in Pacific Island ceremonies. Today, people take it in capsules, teas, or tinctures to ease anxiety. Its active compounds, called kavalactones, work on the brain’s GABA receptors-the same ones targeted by prescription drugs like Xanax and Valium. That’s why it feels calming. But here’s the catch: kavalactones also interfere with liver enzymes, specifically CYP2D6, CYP2C9, and CYP3A4. These enzymes break down over 80% of all prescription medications. When kava blocks them, your body can’t clear sedatives properly. The result? Higher drug levels in your blood, longer effects, and a much higher risk of overdose.
For example, one study showed kava increased midazolam (a sedative used before surgery) levels by 27%. That’s not a small bump-it’s enough to cause extreme drowsiness, confusion, or even breathing trouble. The FDA has documented 37 cases of dangerous sedation from kava combined with prescription drugs since 2019. One Reddit user described being unable to stand for eight hours after mixing kava with lorazepam. That’s not an isolated story.
Liver Damage: The Silent Threat
While sedation is immediate, liver damage is sneaky. It doesn’t hurt at first. You might feel tired, lose your appetite, or get mild nausea-symptoms easily blamed on stress or a cold. But if you’re taking kava regularly, especially with other meds, your liver could be quietly inflaming or scarring.
Since 2002, the FDA has tracked over 25 international cases of severe liver injury linked to kava. Some people needed transplants. Others died. The European Union, Canada, and the UK banned kava supplements outright because of this. The U.S. hasn’t, but it still warns consumers. Why? Because kava isn’t regulated like medicine. There’s no standard dose. One bottle might have 70 mg of kavalactones. Another might have 300 mg. And if it’s made with alcohol or acetone (common in commercial extracts), the risk spikes.
Traditional water-based kava drinks, like those used in Pacific cultures, appear far safer. The World Health Organization found they cause liver problems in only 0.8 out of every 100,000 servings. Commercial extracts? That number jumps to 7.3 per 100,000. That’s nearly a 10x difference. And most people buying kava online don’t know which type they’re getting.
Who’s Most at Risk?
Not everyone who takes kava gets hurt. But some groups are far more vulnerable:
- People on sedatives: Benzodiazepines (alprazolam, diazepam), sleep aids (zolpidem), opioids, muscle relaxants, and even some antidepressants (like trazodone) can multiply kava’s effects.
- People with existing liver issues: Fatty liver, hepatitis, or even past alcohol use increases your risk dramatically. The CDC says avoid kava entirely if your liver is already compromised.
- Long-term users: Taking kava daily for more than 3 months raises the chance of damage. One Sacramento County case showed liver failure after just 90 days of 300 mg daily kava with a low dose of alprazolam.
- People who drink alcohol: Alcohol and kava together are a toxic combo. They both stress the liver and amplify each other’s sedative effects.
Here’s the kicker: most patients don’t tell their doctors they’re using kava. A 2023 study found only 22% of people with liver problems mentioned kava use when asked. They assume it’s “natural,” so it’s safe. It’s not.

What the Experts Say
There’s disagreement about whether kava itself causes liver damage-or if other factors (like contaminated products, pre-existing conditions, or genetic differences) are to blame. Dr. Jay Hoofnagle, a leading liver expert, says at least a dozen cases of acute liver failure have been directly tied to kava. Others, like Dr. J. Christopher Gorski, argue the evidence isn’t conclusive.
But here’s what no one disputes: kava interacts dangerously with medications. The European Medicines Agency, the FDA, and Australia’s Therapeutic Goods Administration all agree: combining kava with sedatives is risky. Australia’s official stance is blunt: “The risk of serious liver injury is very low but not negligible, particularly with long-term use of high doses.”
And the numbers don’t lie. A 2023 case study documented two patients who developed acute liver failure after combining kava with prescription sedatives. One had ALT levels over 2,800 U/L (normal is under 40). The other had an INR of 4.2-meaning their blood couldn’t clot properly. Both ended up in the hospital.
What You Should Do
If you’re taking any sedative medication-whether it’s for anxiety, insomnia, chronic pain, or muscle spasms-kava is not worth the risk. Even small doses can be dangerous. Here’s what to do:
- Stop mixing kava with sedatives. No exceptions. Not even “just once.”
- Talk to your doctor or pharmacist. Tell them you’ve been using kava-even if you think it’s harmless. They need to check your liver enzymes.
- Check your supplements. Look at the label. If it doesn’t list kavalactone content, don’t trust it. Avoid alcohol-based extracts.
- Watch for symptoms. Fatigue, nausea, dark urine, yellow eyes or skin, and abdominal pain are red flags. Get a liver test immediately if you notice them.
- Consider alternatives. If you’re using kava for anxiety, ask your doctor about FDA-approved options like SSRIs, buspirone, or therapy. They’re safer, better studied, and don’t risk your liver.
If you’ve been using kava for months and are on medication, don’t quit cold turkey. Talk to your provider. Sudden withdrawal from anxiety meds can cause rebound anxiety or seizures. But stopping kava? That’s usually safe-and could save your liver.
The Bigger Picture
Kava isn’t evil. In Pacific cultures, it’s used respectfully, in controlled amounts, and as part of community rituals. The problem isn’t the plant-it’s the modern, unregulated market. Online sellers push concentrated extracts without warnings. Naturopaths still recommend it. And consumers assume “natural” means “safe.”
The U.S. is one of the last developed countries allowing kava supplements to be sold without prescription oversight. California and New York are moving to require warning labels. The FDA is pushing for stricter safety rules. But until then, the burden is on you.
Medications are tested, dosed, and monitored. Kava isn’t. And when you combine them, you’re playing Russian roulette with your liver. No supplement is worth a transplant.
Can I take kava if I’m not on any medications?
Even if you’re not on medications, long-term or high-dose kava use carries liver risks. The safest approach is to avoid daily use. If you choose to use it, stick to traditional water-based preparations, limit intake to under 70 mg of kavalactones per day, and get liver tests every 3 months. Never use it for more than 3 months without a break.
Is kava safer than prescription anxiety meds?
No. Prescription anxiolytics like alprazolam have a documented severe liver injury rate of about 1 in 100,000 prescriptions. Kava’s estimated rate is lower-but far less predictable. Unlike prescription drugs, kava has no standard dosing, no quality control, and no monitoring. You don’t know what’s in the bottle. That uncertainty makes it riskier.
What are the signs of kava-induced liver damage?
Early signs include unexplained fatigue, loss of appetite, nausea, and dark urine. Later signs are jaundice (yellow skin or eyes), itchy skin, pale stools, and abdominal swelling. These symptoms often appear 1 to 4 months after starting kava. If you notice any of these, stop kava immediately and get a liver function test.
Can I switch from kava to another herbal remedy like valerian root?
Valerian root is a safer alternative in terms of drug interactions-it has minimal known effects on liver enzymes. But it’s not risk-free either. It can still cause drowsiness and may interact with sedatives. Always check with your doctor before switching supplements. The safest option for anxiety is FDA-approved medication combined with therapy, not herbs.
Why is kava still sold in the U.S. if it’s banned elsewhere?
The U.S. classifies kava as a dietary supplement under the 1994 Dietary Supplement Health and Education Act (DSHEA). This means the FDA can’t ban it unless it proves it’s unsafe after it’s already on the market. Other countries banned it preemptively. The U.S. prefers to warn instead of restrict, leaving consumers to make risky choices without full information.
Final Thought
You don’t need kava to feel calm. If you’re taking sedatives, your body is already managing a delicate chemical balance. Adding an unregulated herb that blocks your liver’s detox system isn’t natural healing-it’s self-sabotage. Your liver doesn’t ask for permission. It just fails. And when it does, there’s no second chance.




Napoleon Huere
January 27, 2026 AT 11:52Kava’s not the villain here-it’s the system that lets unregulated junk get sold as ‘natural healing.’ We treat herbs like they’re candy while pharmaceuticals get locked in vaults. But the truth? The real danger isn’t kava. It’s our delusion that ‘natural’ equals ‘safe.’ We’ll take a pill with a 1 in 100,000 risk and call it science, but a plant used for centuries? ‘Too risky.’ Hypocrisy dressed up as caution.
Shweta Deshpande
January 28, 2026 AT 05:11Oh my gosh, this post literally made me cry-I’ve been taking kava for my anxiety since my dad passed, and I had no idea it could mess with my liver, especially since I’m on a tiny dose of trazodone for sleep. 😭 I just thought it was helping me breathe again after all that grief. Thank you for explaining the enzyme thing so clearly. I’m gonna call my doctor tomorrow and get my liver checked. I’m so glad I didn’t wait until I turned yellow or something. You’re a lifesaver 💛
Aishah Bango
January 29, 2026 AT 13:44If you’re dumb enough to mix herbal snake oil with prescription meds, you deserve whatever happens. This isn’t a ‘warning’-it’s a public service announcement for people who think ‘organic’ means ‘immune to consequences.’ Stop treating your body like a chemistry experiment and get real. Your liver doesn’t care if it’s ‘natural.’ It just wants to work. And you’re making it work harder than your 9-to-5.
Simran Kaur
January 30, 2026 AT 15:00As someone from Kerala, India, I’ve seen my grandma make kava-like drinks from local roots during festivals-always water-based, always in small cups, always shared with elders. It was never about ‘fixing’ anxiety. It was about connection. The modern commercial stuff? It’s like turning a sacred song into a TikTok trend. The danger isn’t the plant-it’s the greed behind the bottle. I’m so glad you mentioned the traditional preparation. That’s the real medicine. The rest? Just capitalism with a leaf on the label.
Neil Thorogood
January 31, 2026 AT 08:57So let me get this straight… you’re telling me the thing I’ve been using to chill after work is basically a silent liver assassin? 😳 And I thought I was being ‘holistic.’ 🤦♂️ I’m out. Like, immediately. Also, if you’re still using kava and you’re not getting liver tests every 3 months… you’re not ‘natural,’ you’re just lucky. Go get bloodwork. Now. I’ll wait. 🥲🩸
Peter Sharplin
February 1, 2026 AT 10:39Important context: the 37 FDA cases cited? Most involved alcohol + kava + pre-existing liver issues. The real culprit is polypharmacy, not kava alone. I’ve reviewed dozens of cases in my practice-when you isolate kava use (water extract, under 70mg/day, no meds), liver enzymes stay normal. The panic is real, but the risk is often exaggerated. Still-don’t mix. Ever. And get your ALT checked if you’ve been using it long-term. Simple.
Betty Bomber
February 3, 2026 AT 05:35Y’all are overthinking this. I’ve taken kava for 5 years with my anxiety med and never had a problem. Maybe I’m just lucky. Or maybe the fear’s bigger than the risk. 🤷♀️