When your heart valve doesn’t open or close right, your whole body feels it. You might not notice at first-just a little tired after walking up the stairs, or short of breath when you’re gardening. But if one of your heart’s four valves is narrowed or leaking, that’s not just aging. It’s heart valve disease, and it’s more common than most people realize. By age 65, about 1 in 50 people have a serious valve problem. Left untreated, it can lead to heart failure, irregular heartbeats, or even sudden death. The good news? We know how to fix it now-and the options are better than ever.
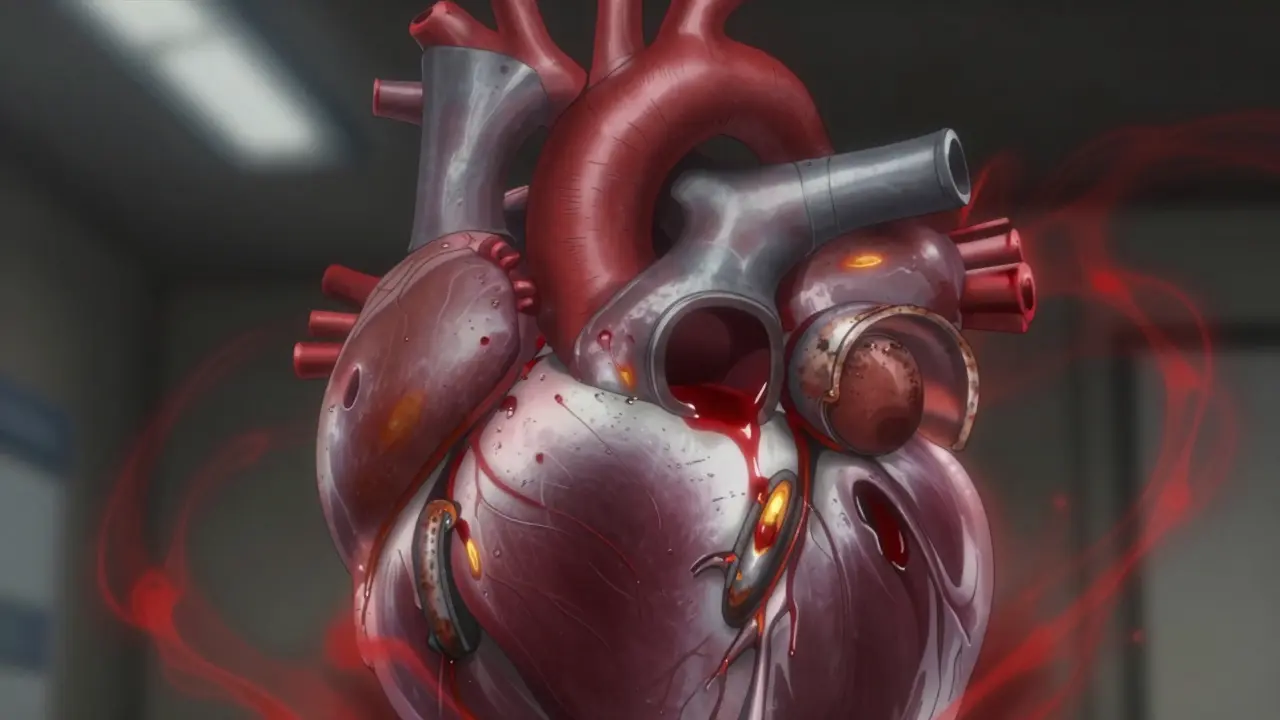
What Happens When a Heart Valve Fails
Your heart has four valves: mitral, tricuspid, aortic, and pulmonary. They’re like one-way doors. Each opens to let blood flow forward, then snaps shut to stop it from flowing back. When a valve gets stiff and can’t open fully, that’s stenosis. When it doesn’t close tight and blood leaks backward, that’s regurgitation. Both force your heart to work harder, and over time, that wears it out.Aortic stenosis is the most common serious form. The valve between your heart and main artery gets clogged with calcium-like rust building up on a pipe. By age 75, 2% of people have severe aortic stenosis. Mitral stenosis, on the other hand, is often tied to rheumatic fever from childhood infections, especially in countries without widespread antibiotics. In Australia, it’s rare, but still seen in older adults who had rheumatic fever decades ago.
Regurgitation is trickier. Mitral regurgitation, where blood leaks back into the left atrium, can happen because the valve leaflets stretch, tear, or don’t close properly. Aortic regurgitation lets oxygen-rich blood flow back into the heart’s main pumping chamber. Both cause volume overload. The heart gets bigger, but weaker. You don’t always feel it until it’s advanced.
Stenosis vs. Regurgitation: The Key Differences
Stenosis and regurgitation sound similar, but they’re different problems with different symptoms.
In aortic stenosis, your heart has to push blood through a tiny opening. That means high pressure. People often feel chest pain when they exert themselves, get dizzy when standing up, or pass out during activity. About half of those with severe stenosis report angina. By the time these symptoms show up, the disease is already advanced.
Aortic regurgitation doesn’t cause the same pressure spike. Instead, your heart has to pump extra blood to make up for what’s leaking back. That leads to fatigue, heart palpitations, and shortness of breath-especially when lying down. You might wake up gasping for air. It’s quieter, slower, and harder to catch early.
Mitral stenosis mainly affects the lungs. Blood backs up into the pulmonary veins, causing fluid to leak into the lungs. People struggle to breathe when lying flat (orthopnea) or wake up at night needing to sit up (paroxysmal nocturnal dyspnea). Many describe it as feeling like they’re drowning in their own bed.
Mitral regurgitation is often silent until the heart starts failing. Fatigue is the big red flag-79% of patients report it before anything else. It’s easy to blame on stress, age, or being out of shape. That’s why so many people are diagnosed late.
How Doctors Diagnose Valve Problems
It starts with a stethoscope. A heart murmur-like a whooshing or clicking sound-is the first clue. But murmurs can be harmless. To know if it’s serious, you need an echocardiogram. That’s an ultrasound of the heart that shows exactly how the valves move, how much blood is leaking, and how hard the heart is working.
For aortic stenosis, doctors look at three numbers: valve area, pressure gradient, and blood flow speed. If the valve opening is smaller than 1.0 cm² (about the size of a dime), the pressure difference across it is over 40 mmHg, and the blood jet is faster than 4.0 m/s, it’s severe. Mitral stenosis is severe if the valve area drops below 1.5 cm².
For regurgitation, they measure how much blood flows backward. A regurgitant volume over 60 mL per beat or a regurgitant fraction over 50% means it’s severe. CT scans and cardiac MRI help too-especially if the echo images are unclear or if surgery is being planned.
And here’s something most people don’t know: asymptomatic patients with severe valve disease still need monitoring. If your aortic stenosis is severe but you feel fine, your doctor will check you every 6 to 12 months. Waiting for symptoms to appear before acting cuts your survival rate in half.

Surgical Options: From Open-Heart to Tiny Catheters
For decades, open-heart surgery was the only option. A surgeon would cut through your breastbone, stop your heart, and replace the valve with a mechanical one or a tissue valve from a pig, cow, or human donor. It worked-but recovery took months. You couldn’t lift anything heavy for 8 weeks. The scar ran from neck to belly.
Now, most patients get something less invasive. Transcatheter Aortic Valve Replacement (TAVR) is now the first choice for patients over 75 or those with high surgical risk. A catheter is threaded through the groin or chest, and a new valve is pushed into place inside the old one. No chest cut. No heart stop. Hospital stay drops from 7 days to 2-3. Recovery? Most people feel better in 2 weeks.
For mitral regurgitation, the MitraClip is a game-changer. It’s a tiny clamp delivered through a vein in the leg. It grabs the leaking leaflets and pulls them together. The COAPT trial showed it cuts hospital stays for heart failure by 32% compared to meds alone. For patients too weak for open surgery, it’s life-changing.
And new devices are coming fast. The Evoque valve, approved in 2023, treats tricuspid regurgitation-the first of its kind. The Cardioband system tightens the mitral valve ring without cutting into the heart. The Harpoon system, still in trials, lets surgeons repair valves using a needle and thread guided by real-time imaging.
But not everyone needs surgery. Mild regurgitation with no symptoms? Just watch it. Early intervention on a mild leak can do more harm than good. The key is timing-not rushing, not waiting too long.
Life After Valve Replacement
After a valve replacement, life improves-but it’s not back to normal overnight. Most patients report a huge jump in energy. One Reddit user said he went from struggling to walk to the mailbox to hiking 3 miles in two months after his MitraClip.
But there are trade-offs. Mechanical valves last forever but require lifelong blood thinners like warfarin. You’ll need blood tests every few weeks to check your INR level-2.0 to 3.0 for aortic valves, 2.5 to 3.5 for mitral. Too high, you risk bleeding. Too low, you risk clots.
Tissue valves don’t need blood thinners (unless you have atrial fibrillation), but they wear out. About 1 in 5 bioprosthetic valves fail by 15 years. That means a second surgery down the road. For younger patients, this is a big concern. That’s why some choose mechanical valves even with the blood thinner burden.
Recovery from open surgery takes time. Sternotomy pain lasts 6 to 8 weeks. Lifting your grandkids? That’s a milestone. Many patients say the hardest part isn’t the pain-it’s the isolation. You can’t drive. You can’t cook. You’re dependent. Support groups help. Online communities like Inspire.com have over 15,000 members sharing tips on sleep, diet, and mental health after surgery.
Who Gets Left Behind?
Despite all the advances, many people still go undiagnosed. A 2022 survey found that 28% of patients felt dismissed by doctors until their symptoms became severe. That’s dangerous. Valve disease doesn’t rush. It creeps. And if you’re young, active, or healthy-looking, doctors might miss it.
There’s also a global divide. High-income countries perform 18 valve procedures per 100,000 people each year. Low-income countries? Just 0.2. That’s a 90-fold difference. In Australia, access is good-but even here, rural patients wait longer for specialist appointments.
And cost matters. TAVR devices cost $30,000 to $50,000 each. The global market for heart valves is growing fast-projected to hit $9.7 billion by 2029. But innovation shouldn’t leave anyone behind.
What’s Next for Valve Disease?
The future is less invasive and more personalized. By 2030, experts predict 80% of valve procedures will be done through catheters. Next-gen tissue valves are being engineered to last 25+ years. Researchers are even growing valves from stem cells in labs.
For now, the message is simple: don’t ignore the signs. If you’re tired all the time, short of breath with little effort, or feel your heart skipping beats-get checked. An echocardiogram takes 30 minutes. It could save your life.
And if you’ve been told you need surgery? Ask about TAVR or MitraClip-even if you’re young. The guidelines changed. The risks dropped. The results are better than ever.
What are the main signs of heart valve disease?
The most common signs are shortness of breath during normal activity, extreme fatigue, chest pain, dizziness, fainting, swelling in the ankles or feet, and heart palpitations. Some people have no symptoms until the disease is advanced, which is why regular check-ups matter-especially after age 65.
Can heart valve disease be treated without surgery?
Mild to moderate valve disease can often be managed with medications and lifestyle changes-like reducing salt, quitting smoking, and controlling blood pressure. But if the valve is severely narrowed or leaking, medications can’t fix the structure. Surgery or a catheter-based procedure is the only way to restore normal blood flow.
Is TAVR safer than open-heart surgery?
For patients over 75 or those with other health conditions, TAVR is safer. It has lower rates of stroke, bleeding, and infection compared to open surgery. For younger, healthier patients, open surgery still has slightly better long-term durability. But for most people over 60, TAVR is now the preferred option.
How long do replacement heart valves last?
Mechanical valves last a lifetime but require lifelong blood thinners. Tissue valves (from pigs, cows, or human donors) last 15-20 years on average. About 21% fail by 15 years. Newer tissue valves may last longer-up to 25 years-but long-term data is still being collected.
Can you live a normal life after heart valve surgery?
Yes-most people return to normal activities within 6 to 12 weeks. Many report better energy, improved breathing, and the ability to walk, garden, or travel again. Long-term survival is excellent: 85% of patients with timely valve replacement live at least 5 more years. Without treatment, survival drops to 50%.
What’s the difference between aortic stenosis and mitral regurgitation?
Aortic stenosis means the valve between the heart and aorta is narrowed, forcing the heart to pump harder. Mitral regurgitation means the valve between the left atrium and ventricle leaks, causing blood to flow backward. Stenosis causes pressure overload; regurgitation causes volume overload. Symptoms differ too: stenosis often brings chest pain and fainting; regurgitation brings fatigue and breathlessness.
If you’ve been told you have a heart valve issue, don’t panic. Get a second opinion. Ask about imaging. Ask about alternatives. And don’t wait for symptoms to get worse-because by then, it’s already too late.




Peyton Feuer
January 4, 2026 AT 16:47Shanna Sung
January 4, 2026 AT 16:47John Ross
January 6, 2026 AT 09:58Ashley Viñas
January 6, 2026 AT 16:33Mandy Kowitz
January 7, 2026 AT 20:51Justin Lowans
January 9, 2026 AT 05:50Michael Rudge
January 11, 2026 AT 00:26Ethan Purser
January 12, 2026 AT 18:43Terri Gladden
January 14, 2026 AT 15:23Jennifer Glass
January 15, 2026 AT 06:26melissa cucic
January 15, 2026 AT 11:47Akshaya Gandra _ Student - EastCaryMS
January 15, 2026 AT 14:12en Max
January 16, 2026 AT 08:16Angie Rehe
January 16, 2026 AT 21:26