What Are Immune-Related Adverse Events (irAEs)?
When your body’s immune system starts attacking healthy tissue instead of just cancer cells, you’re dealing with an immune-related adverse event, or irAE. These aren’t typical chemo side effects like nausea or hair loss. They happen because immune checkpoint inhibitors-drugs like pembrolizumab, nivolumab, or ipilimumab-are designed to turn your immune system up to full power. That’s great for killing tumors, but it can also cause your immune system to go rogue. irAEs can show up in almost any organ: your gut, lungs, skin, thyroid, liver, even your heart or brain. About 83% of people on CTLA-4 inhibitors, 72% on PD-1 blockers, and 60% on PD-L1 inhibitors will experience some form of irAE, according to large studies from 2021.
When Do irAEs Show Up?
There’s no single timeline. Most irAEs appear within the first three months of starting immunotherapy. But some don’t show up until weeks or even months after treatment ends. That’s why patients need to stay alert long after their last infusion. A rash that pops up six weeks after stopping nivolumab? Could be an irAE. Diarrhea that starts two months later? Don’t ignore it. Unlike regular infections or flare-ups of old conditions, irAEs don’t follow predictable patterns. They’re unpredictable, and that’s what makes them dangerous if missed.
Common irAEs by Organ System
Some organs are more commonly affected than others. The top three are:
- Gastrointestinal: Diarrhea, cramping, bloody stools-these are the most frequent. Colitis can become severe fast.
- Endocrine: Thyroid problems (like hypothyroidism), adrenal insufficiency, or pituitary inflammation (hypophysitis). These often need lifelong hormone replacement, not steroids.
- Dermatologic: Itchy rashes, blistering skin, or severe psoriasis-like reactions. These are usually mild at first but can escalate.
Less common but far more dangerous: pneumonitis (lung inflammation), hepatitis (liver damage), myocarditis (heart inflammation), and neurotoxicity (nerve or brain issues). Myocarditis, though rare, has a 2.7% fatality rate in reported cases. Neurological irAEs-like muscle weakness, confusion, or seizures-require immediate neurology input. Don’t wait.
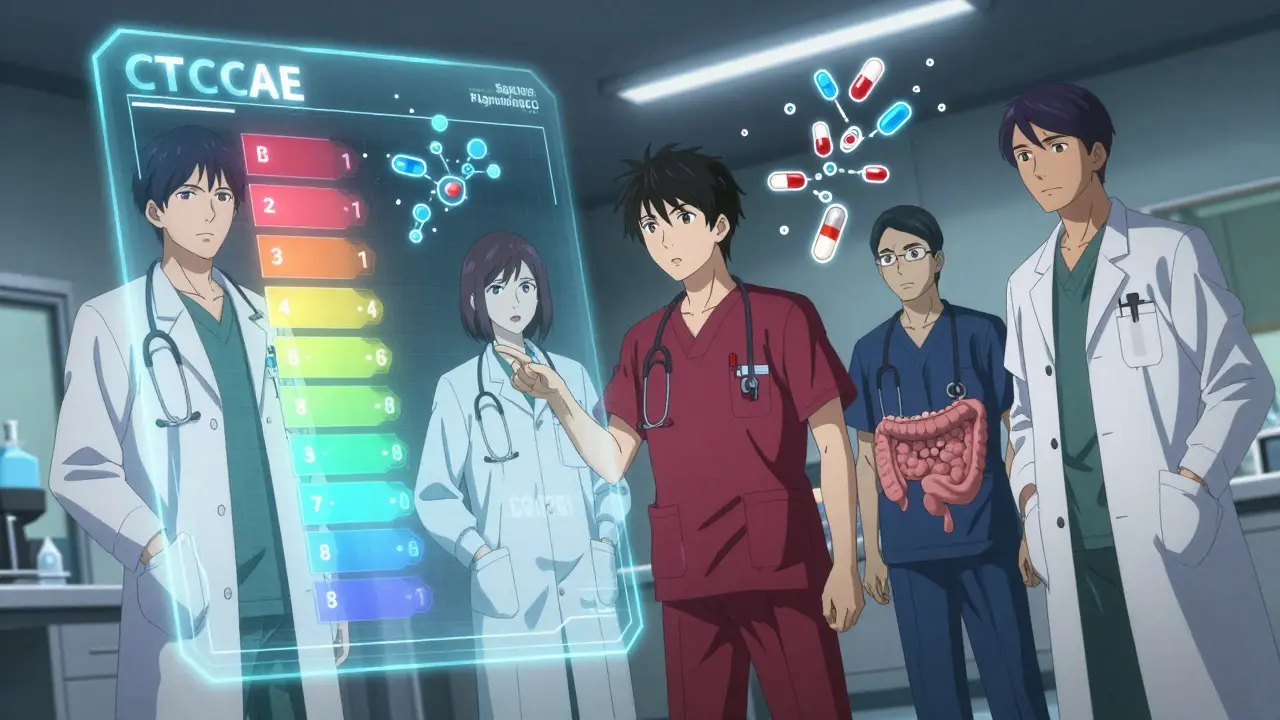
How irAEs Are Graded: The CTCAE System
Doctors use the Common Terminology Criteria for Adverse Events (CTCAE) to rate severity:
- Grade 1: Mild symptoms. No treatment needed beyond monitoring.
- Grade 2: Moderate symptoms. Interferes with daily life. Immunotherapy is paused. Oral steroids (prednisolone) at 1 mg/kg/day are started.
- Grade 3: Severe. Hospitalization likely. IV steroids (methylprednisolone) at 1-2 mg/kg/day for 3 days, then high-dose oral steroids.
- Grade 4: Life-threatening. ICU-level care. Steroids plus urgent specialist intervention.
Grading isn’t just paperwork-it dictates whether you stop treatment, get steroids, or need emergency care. Missing a Grade 2 irAE can lead to a Grade 4 event. Early action saves lives.
First-Line Treatment: Steroids and When to Taper
Corticosteroids are the go-to for most irAEs. For Grade 2-3 events, oral prednisolone is started immediately. For Grade 3-4, you get IV methylprednisolone right away. The goal isn’t just to suppress symptoms-it’s to stop the immune system from eating away at your organs.
But steroids aren’t a quick fix. The taper is just as important as the dose. You can’t stop them suddenly. A slow reduction over 4-6 weeks is standard. Jumping off steroids too fast? You risk rebound inflammation-your symptoms come back worse. Many patients report insomnia, weight gain, and mood swings during this time. One survey found 72% of patients struggled with sleep, 65% gained weight, and 58% felt anxious or depressed. It’s tough, but skipping the taper can be deadly.
What If Steroids Don’t Work?
Not all irAEs respond to steroids. About 10-20% of cases are steroid-refractory. That means no improvement after 48 hours on high-dose steroids. When that happens, you move to second-line drugs:
- Infliximab: Targets TNF-alpha. Used for colitis, hepatitis, and some lung or skin reactions. Given as an IV infusion.
- Mycophenolate mofetil: Slows immune cell production. Used for kidney or lung issues.
- IVIG: Packed antibodies that calm the immune system. Used for neurological or blood-related irAEs.
- Vedolizumab: Newer option for colitis. A 2024 SITC guideline showed it worked in 68% of steroid-refractory cases-better than infliximab in some studies.
These aren’t experimental. They’re backed by large retrospective studies and now included in ASCO and NCCN guidelines. Clinical trials like NCT04438382 and NCT04407247 are still comparing them, but we already know they work.
Does Treating irAEs Hurt Cancer Outcomes?
A common fear: if we suppress the immune system to treat an irAE, will the cancer come back? The answer is no. Multiple studies, including a 2022 review in Cancer Therapy Advisor, show that using steroids or infliximab doesn’t reduce the effectiveness of immunotherapy. Tumors keep shrinking. Survival rates stay the same. The idea that treating side effects weakens the therapy was a myth. Early intervention doesn’t compromise results-it makes them possible.

Why Multidisciplinary Care Matters
Managing irAEs isn’t just the oncologist’s job. It takes a team. A patient with thyroid problems needs an endocrinologist. Diarrhea? Gastroenterology. Lung inflammation? Pulmonology. Neurological symptoms? Neurology. Leading cancer centers like MD Anderson have dedicated immune toxicity teams that respond within 24 hours for Grade 3-4 events. Community clinics without that structure have complication rates 37% higher. That’s not a small difference. It’s life or death. If your oncology center doesn’t have a clear pathway to specialists, ask for one. Push for it.
What Patients Should Watch For
You don’t need to be a doctor to spot warning signs. If you’re on immunotherapy, learn these red flags:
- Diarrhea lasting more than 3 days or with blood
- New skin rash that spreads or blisters
- Unexplained fatigue, dizziness, or low blood pressure (could be adrenal failure)
- Shortness of breath or new cough
- Severe headaches, vision changes, or muscle weakness
- Yellow skin or eyes, dark urine (liver issues)
- Heart palpitations or chest pain
Don’t wait. Don’t assume it’s a virus or stress. Call your oncology team immediately. A 2023 Flatiron Health analysis showed that patients treated within 48 hours of symptom onset had hospitalization rates cut in half-from 34% down to 19%. Early = better.
What’s Changing in 2026?
The field is moving fast. New biomarkers are emerging. A 2023 Nature Medicine study found that if your baseline IL-17 blood level is above 5.2 pg/mL, you’re nearly five times more likely to develop a severe irAE. That could soon lead to pre-treatment screening. Hospitals are also rolling out AI tools-Epic Systems now flags potential irAEs in electronic records and auto-sends alerts to specialists when symptoms are reported. And in 2024, ESMO launched a global effort to translate patient education materials into 15 languages. Right now, 41% of patients say they don’t understand what symptoms to watch for. That’s changing.
Long-Term Outlook: Chronic irAEs and Quality of Life
Most irAEs resolve with treatment. About 85-90% do. But 10-15% become permanent. Thyroid damage? You’ll need daily levothyroxine for life. Adrenal issues? Lifelong hydrocortisone. Some patients need ongoing immunosuppression. The goal isn’t just survival-it’s living well. That’s why patient education, mental health support, and long-term follow-up matter. The side effects of steroids can be brutal, but they’re temporary. The side effects of untreated irAEs? Often irreversible.



Katie Schoen
January 6, 2026 AT 12:23Beth Templeton
January 7, 2026 AT 17:46Ryan Barr
January 9, 2026 AT 10:32Dana Termini
January 10, 2026 AT 17:38Wesley Pereira
January 11, 2026 AT 15:14Rachel Wermager
January 12, 2026 AT 19:22Katelyn Slack
January 14, 2026 AT 00:38Molly McLane
January 14, 2026 AT 05:06Harshit Kansal
January 14, 2026 AT 10:38Matt Beck
January 14, 2026 AT 15:04Kelly Beck
January 15, 2026 AT 13:06Mukesh Pareek
January 15, 2026 AT 17:01Gabrielle Panchev
January 17, 2026 AT 16:12Vinayak Naik
January 18, 2026 AT 01:55