
When your big toe explodes in pain, you don’t care about labels-you just want it to stop.
You wake up with your foot on fire. The swelling is so bad your sock feels like a noose. Walking is out of the question. This isn’t just a bad bruise. This is a gout flare, and it’s one of the most painful things your body can throw at you. If you’ve been through it once, you know the dread of it coming back. And if you’re reading this, you’re probably trying to figure out what actually works to kill the pain-fast.
There are three main tools doctors reach for: NSAIDs, colchicine, and steroids. All three can bring relief. But which one is right for you? It’s not about which is "best." It’s about which fits your body, your health, and your life.
NSAIDs: The Go-To, But Not for Everyone
NSAIDs-like naproxen, ibuprofen, and indomethacin-are the most common first choice for gout flares. They work by cutting down inflammation, which is what’s causing the swelling and burning pain. The American College of Rheumatology says they’re a solid starting point. But here’s the catch: you need to take them hard to get results.
For naproxen, you’re looking at 500 mg twice a day. Ibuprofen? 800 mg three times a day. Indomethacin? 50 mg three times daily. That’s a lot of pills. And that’s just the beginning. These drugs don’t just reduce pain-they also stir up trouble in your stomach, kidneys, and heart.
If you’ve got high blood pressure, kidney trouble, a history of ulcers, or you’re on blood thinners, NSAIDs can be dangerous. That’s not a small "maybe." It’s a hard stop. And if you’re over 65, which many gout patients are, your body handles these drugs less forgivingly. A study from the WVU School of Pharmacy found that while naproxen worked just as well as low-dose colchicine, it caused fewer side effects. But even "fewer" doesn’t mean "none."
Only three NSAIDs-indomethacin, naproxen, and sulindac-have FDA approval for gout. But in practice, doctors use almost any NSAID at high doses. The goal? Get pain under control within 24 hours. Delay treatment, and the flare lasts longer, hurts worse, and takes more to fix.
Colchicine: The Delicate Balancing Act
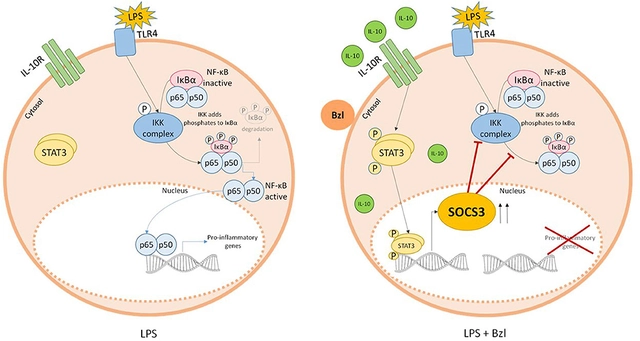
Colchicine has been used for gout for over a century. It doesn’t reduce inflammation like NSAIDs. Instead, it stops the immune system’s overreaction to uric acid crystals. Think of it as putting a lid on the fire instead of dousing it.
Here’s the big shift: the old dosing-4.8 mg over six hours-was brutal. Nausea, vomiting, diarrhea? Guaranteed. But new research changed everything. A 2023 analysis showed that 1.8 mg taken all at once works just as well, with way fewer side effects. That’s a game-changer. You’re not taking pills for hours-you’re taking one or two, and you’re done.
But colchicine has a narrow window. Too much, and you risk serious problems: muscle damage, nerve issues, even life-threatening toxicity. If your kidneys aren’t working well, your body can’t flush it out. That means dose adjustments are non-negotiable. And if you’re on statins or certain antibiotics, the interaction can be deadly.
One study found that colchicine and naproxen gave similar pain relief over seven days. But colchicine caused more stomach upset. It’s effective-but it’s like driving a sports car with no airbags. You need to know exactly what you’re doing.
Steroids: The Quiet Winner
Steroids-like prednisone-are often overlooked. People hear "steroid" and think bodybuilders or mood swings. But a short course of oral steroids for gout is nothing like that. It’s a precise, timed burst of anti-inflammatory power.
Typical dosing? 40-60 mg on day one, then slowly tapered over 10-14 days. That taper is critical. Skip it, and your flare can come roaring back. But get it right, and steroids are one of the most effective options out there.
Here’s why they’re gaining ground: they’re safer for people with kidney disease, heart problems, or stomach ulcers. A 2017 meta-analysis of six trials with 817 patients found steroids worked just as well as NSAIDs for pain relief. But they caused fewer serious side effects. For older patients with multiple health issues, that’s huge.
And if your flare is only in one joint-say, your big toe or knee-an injection right into the joint can be magic. No pills. No stomach upset. Just targeted relief. The AAFP recommends this for single-joint flares because it avoids the whole-body effects of oral meds.
One downside? Steroids can spike blood sugar. If you have diabetes, you’ll need to check your levels more often. But that’s manageable. And for many, the trade-off is worth it.
Who Gets What? It’s Not One-Size-Fits-All
There’s no universal winner. It’s about matching the drug to the person.
- If you’re young, healthy, and have no stomach or kidney issues? NSAIDs are fine. Just don’t delay-start within 24 hours.
- If you have kidney trouble, heart disease, or a history of ulcers? Skip NSAIDs. Colchicine might work, but only if your kidneys are stable and you’re not on other risky meds.
- If you’re older, on multiple medications, or have diabetes? Steroids are often the safest bet. Oral or injected, they get the job done without wrecking your gut or kidneys.
And here’s something most people don’t realize: sometimes, you need two. If one drug doesn’t fully control the pain, combining steroids with low-dose colchicine can be powerful. Or NSAIDs with colchicine. It’s not about being "stronger." It’s about covering more bases.
Dr. Robert T. Keenan, a rheumatologist at Duke, says it best: "Not all gout flares will respond to just one medication." He’s seen patients who need combinations. He also says: start treatment within 24 hours-ideally, "within 24 seconds of the onset of pain." That’s not hyperbole. The sooner you act, the faster it fades.
What Happens After the Pain Stops?
Fixing the flare is only half the battle. Gout doesn’t go away because the pain does. It’s a chronic condition. If you’re on a drug like allopurinol or febuxostat to lower uric acid long-term, you’re still at risk for flares-especially in the first few months.
That’s why guidelines say: if you’re starting urate-lowering therapy, you need to keep taking a low-dose anti-inflammatory for at least three months. If you’ve had tophi (those lumpy deposits under the skin), go for six months. This isn’t optional. It’s what keeps you from going back to square one.
And here’s a practical tip: keep a small supply of your go-to flare medication at home. Don’t wait until you’re in agony to run to the pharmacy. Have it ready. Gout doesn’t care about your schedule.
Bottom Line: Pick the Right Tool, Not the Trendiest One
NSAIDs? Fast, cheap, but risky if you’re not healthy. Colchicine? Effective, but tricky to dose right. Steroids? Safe for most, especially older adults, and just as powerful.
The real answer isn’t in a study or a guideline. It’s in your medical history. Your kidneys. Your stomach. Your other meds. Your age. Your lifestyle. Your doctor should help you pick-not just hand you a script.
And if your flare doesn’t improve in 48 hours? Go back. Something’s wrong. Maybe the diagnosis is off. Maybe you need a different approach. Don’t just suffer through it. Gout is treatable. You just need the right plan.
Can I take NSAIDs and colchicine together for a gout flare?
Yes, but only under a doctor’s supervision. Combining NSAIDs and colchicine can be more effective than either alone, especially for stubborn flares. But this combo increases the risk of side effects-especially stomach upset, kidney strain, and muscle damage. Your doctor will adjust doses based on your kidney function and other medications. Never combine them without medical guidance.
Are steroids safe for people with diabetes?
Short-term steroid use for gout is generally safe for people with diabetes, but it requires close monitoring. Steroids can raise blood sugar levels significantly, especially in the first few days. You’ll need to check your glucose more often-maybe four times a day-and adjust your diabetes meds as needed. Work with your doctor to plan ahead. The flare will pass, but uncontrolled blood sugar can cause lasting damage.
Why do I need to taper steroids instead of stopping them cold?
Stopping steroids suddenly can trigger a rebound flare-sometimes worse than the original. Your body temporarily shuts down its natural steroid production when you take external ones. If you stop abruptly, your body isn’t ready to take over, and inflammation can surge back. Tapering slowly (over 10-14 days) gives your system time to restart. Skipping the taper is a common mistake that leads to relapse.
Is colchicine safe if I have kidney disease?
Colchicine is risky if your kidneys aren’t working well. Your body can’t clear it properly, leading to dangerous buildup. If you have moderate to severe kidney disease, your doctor will lower your dose significantly-or avoid it entirely. For mild kidney issues, a reduced dose (like 0.3 mg once or twice daily) may be safe, but only with careful monitoring. Never take colchicine without checking your kidney function first.
What’s the fastest way to stop a gout flare?
The fastest way is to start treatment within 24 hours of the first sign of pain. Intra-articular steroid injections into the affected joint can bring relief in hours. Oral steroids or high-dose NSAIDs usually work within 24-48 hours. Colchicine takes a bit longer-often 12-24 hours for noticeable improvement. Speed matters more than the drug type. Delaying treatment by even a day can make the flare last twice as long.
Can I use over-the-counter ibuprofen for a gout flare?
You can, but it’s not ideal. Over-the-counter ibuprofen is usually 200 mg per pill. To match the dose used in studies, you’d need to take 800 mg three times a day-that’s 12 pills a day. That’s a lot, and it increases your risk of stomach bleeding and kidney damage. If you’re going to use ibuprofen, it’s safer to get a prescription for a higher dose or switch to a different option like naproxen or steroids. Don’t rely on OTC doses-they’re too low to be effective.
What to Do Next
If you’ve had a gout flare, talk to your doctor about your long-term plan. Don’t just treat the pain-think about prevention. Are you on a uric acid-lowering drug? Are you taking a low-dose anti-inflammatory to protect against future flares? Are your kidneys and liver being monitored regularly?
Keep a symptom journal: when the flare started, what you took, how long it lasted, and how you felt afterward. That info helps your doctor make better choices next time.
Gout isn’t just about diet or alcohol. It’s about the right medicine, at the right time, for your body. Get that right, and you’re not just surviving flares-you’re taking control.


Roshan Gudhe
February 3, 2026 AT 18:59Man, I remember my first gout flare like it was yesterday. Woke up screaming, thought I'd stepped on a nail. Turns out? Just uric acid crystals throwing a rave in my big toe. 😅
What blew my mind was how fast steroids worked. Not like NSAIDs where you're basically chugging pills like candy. One pill, tapering schedule, and boom-pain gone by day three. No stomach screaming, no kidney panic.
I'm diabetic, so I was terrified of steroids. But my rheumatologist walked me through it. Checked glucose four times a day, adjusted insulin, and honestly? It was smoother than I expected. The flare didn't come back. That's the win.
Colchicine? Tried it once. Felt like my insides were doing backflips. One pill and I was on the porcelain throne for six hours. Not worth it. Now I stick with low-dose prednisone. Simple. Effective. No drama.
And yeah-tapering? Non-negotiable. I skipped it once. Thought I was smart. Flare came back worse. Took two weeks to recover. Lesson learned: don't be the guy who thinks he knows better than the science.
Keep your meds handy. I keep a 5-day supply in my bathroom cabinet. No excuses when pain hits at 2 a.m.
Gout ain't about diet. It's about timing, tolerance, and knowing your body. Stop chasing trends. Start chasing relief that actually sticks.