When you or a loved one is taking multiple medications, it’s easy to feel overwhelmed. Maybe you’ve forgotten a dose. Maybe you’re not sure why you’re taking that pill. Or perhaps you’ve noticed new side effects - dizziness, confusion, or stomach upset - and aren’t sure if they’re normal. You’re not alone. In Australia, nearly 9 out of 10 adults over 65 take at least two prescription drugs. About 1 in 6 take five or more. That’s not just common - it’s risky.
Adverse drug reactions are one of the leading causes of hospital visits for seniors. In fact, studies show that up to 20% of hospital admissions for older adults are caused by medication errors or interactions. The good news? Most of these problems can be prevented with better communication. You don’t need to be a medical expert. You just need to know what to say, what to bring, and how to ask the right questions.
Bring Everything - Not Just Your List
Doctors don’t know what you’re taking unless you tell them. And most people don’t remember everything. That’s why bringing your actual medications to the appointment isn’t optional - it’s essential. Don’t rely on memory. Don’t trust a handwritten list alone. Bring the bottles. All of them.
This includes prescription drugs, over-the-counter pain relievers, herbal supplements, vitamins, and even eye drops or creams. Why? Because many seniors don’t realize that something as simple as a daily multivitamin or an herbal remedy like St. John’s Wort can interact dangerously with blood thinners or heart medications. A 2022 study found that when patients brought their real meds to appointments, doctors found discrepancies - like wrong doses, expired pills, or medications no longer needed - in 25% of cases.
Put everything in one bag. No need to organize. Just dump it out on the table. Let the pharmacist or doctor see exactly what’s in your medicine cabinet. It’s messy, but it’s honest. And honesty saves lives.
Prepare Before You Go
Going into an appointment with no plan is like walking into a storm without an umbrella. You’ll get wet. You’ll forget what you wanted to say. And you’ll leave with more questions than answers.
Take 10 minutes before your visit to write down:
- Any side effects you’ve noticed (even if they seem small - “I feel sleepy after lunch” or “I’m more forgetful lately”)
- Any missed doses or changes in how you take your meds
- Any new symptoms - headaches, rashes, nausea, mood changes
- Questions you want answered
Keep this list with you. Read it out loud if you need to. It’s okay to be nervous. But don’t let nerves silence you. Your doctor needs to hear this.
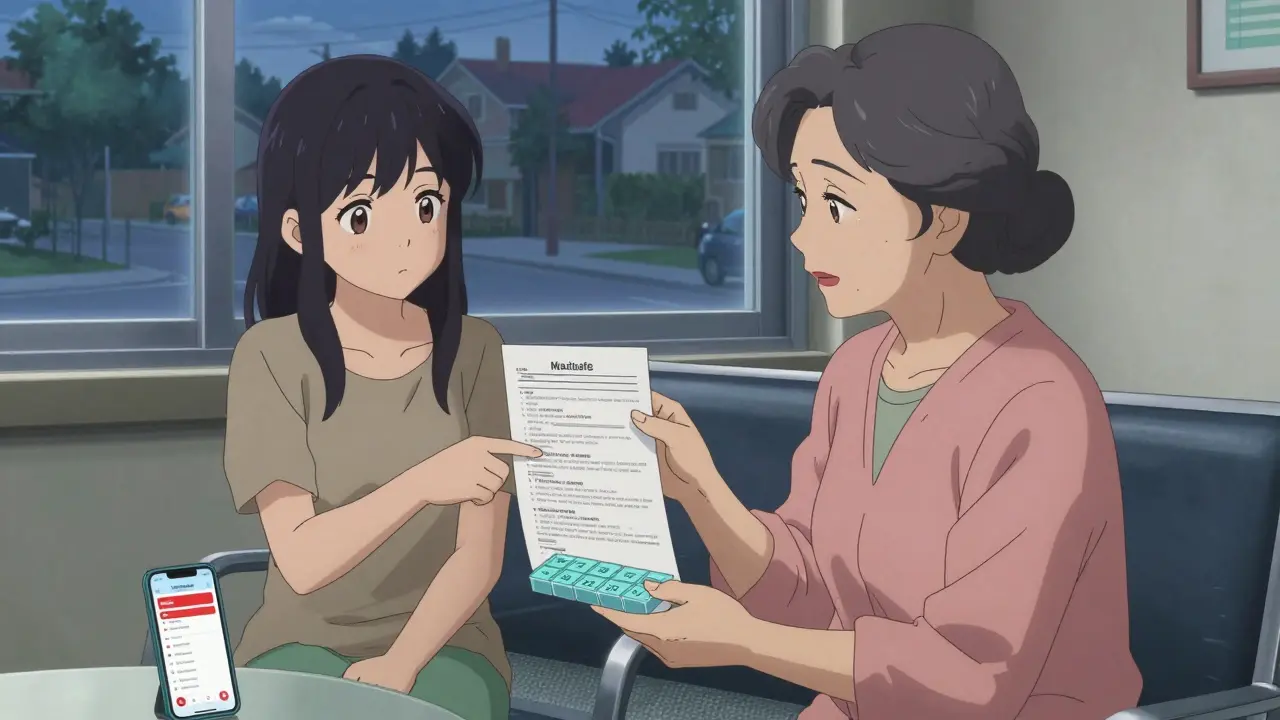
Also, consider bringing someone with you. A spouse, child, or friend. Not just to help carry bags. But to listen, remember what was said, and ask questions you might miss. Studies show seniors with a companion at appointments have 18% fewer adverse drug events.
Ask These Four Questions
Don’t just nod and say “yes” when the doctor says, “This is for your blood pressure.” Ask for clarity. Here are four simple, powerful questions every senior should ask:
- How does this medication specifically help manage my health condition? - Don’t accept vague answers like “It’s good for you.” Ask for the connection between the drug and your diagnosis.
- What are the potential side effects and adverse reactions? - Ask which side effects are common, which are serious, and which require immediate attention.
- What are the drug interactions and potential conflicts? - Especially if you’re taking five or more drugs. Ask if any of them clash with each other or with supplements you’re using.
- What should I do if I miss a dose? - This is often overlooked. Some meds need to be taken exactly on time. Others? Skipping one won’t hurt. Know the difference.
These aren’t hard questions. They’re basic. And if your doctor seems annoyed by them, it’s not you - it’s them. A good provider welcomes these questions. They’re signs of engagement.
Use Tools That Actually Work
Memory fails. Especially as we age. But tools don’t. And there are simple, affordable options that make a real difference.
Pill organizers - Get one with compartments for morning, afternoon, evening, and night. Fill it weekly. It’s visual. It’s tactile. You’ll know if you missed a dose.
Medication apps - Apps like Medisafe or Round Health let you log your meds, set alarms, and even notify a family member if you skip a dose. They’re free, easy to use, and work on any smartphone.
Automated dispensers - Devices that open at set times and dispense pills? They’re not sci-fi anymore. Some cost under $100 and can be set up in minutes. They’re especially helpful if you live alone.
And here’s a pro tip: link your meds to daily routines. Take your morning pills right after brushing your teeth. Take your evening ones before your nightly tea. These habits stick better than alarms.
Review Regularly - Don’t Wait for a Crisis
Polypharmacy - taking five or more medications - isn’t always avoidable. But it shouldn’t be automatic. Many seniors keep taking pills long after they’re needed. A 2022 study found that 27% of seniors could safely reduce their number of medications with a structured review.
Ask your doctor for a medication review at least once a year. Better yet, every six months. During this review, ask:
- “Is this medication still necessary?”
- “Can any of these be stopped or replaced?”
- “Are there simpler, safer options?”
Some drugs - like certain sleeping pills, anticholinergics, or long-term NSAIDs - are flagged in the updated 2023 Beers Criteria as high-risk for seniors. If you’re taking any of these, ask if there’s a safer alternative.
Also, ask about medication synchronization. Many pharmacies now offer this service - they align all your refill dates so you pick everything up in one visit. It cuts down on confusion and missed doses. Ask your pharmacist if it’s available.

Speak Up - Even If It Feels Awkward
Many seniors don’t complain because they don’t want to be a burden. But here’s the truth: your discomfort is the signal. Your silence is the risk.
If you feel foggy, tired, dizzy, or confused - say so. If you’ve stopped taking a pill because it made you feel worse - tell them. If you’re scared of side effects - voice it. Doctors can’t fix what they don’t know.
Use simple language. Say: “I’ve been feeling really tired since I started this new pill.” Not: “I’m experiencing somnolence secondary to pharmacological intervention.”
And if you’re not understood? Ask them to explain again. Use the “teach-back” method: “So, just to make sure I got it - you’re saying I should take this after food, not before?” That’s not being difficult. That’s being smart.
What Happens When You Do This Right?
When seniors communicate clearly about their medications:
- Hospital visits drop by up to 22%
- Medication errors fall by 35%
- Adherence rates rise from 50% to over 75%
- Quality of life improves - not just longevity
It’s not about being perfect. It’s about being consistent. Bring your meds. Ask your questions. Review your list. Use a tool. Speak up.
These aren’t medical procedures. They’re everyday actions. And they’re within your control.
Your health isn’t a mystery. It’s a conversation. And you’re the most important voice in it.
What should I do if I forget to take my medication?
Don’t double up unless your doctor says so. Check the label or call your pharmacist. For some medications, missing a dose isn’t dangerous - for others, it can cause serious issues. Always ask what to do ahead of time. Keep a log of missed doses to share at your next appointment.
Can I stop a medication if I think it’s causing side effects?
Never stop a prescribed medication on your own. Even if you think it’s causing problems, stopping suddenly can be dangerous - especially for blood pressure, heart, or mental health drugs. Instead, write down your symptoms and bring them to your next appointment. Your doctor can help you safely adjust or replace the medication.
Why do I need to bring all my supplements to the appointment?
Many seniors don’t realize supplements can interact with prescription drugs. For example, fish oil can increase bleeding risk when taken with blood thinners. Garlic or ginkgo can affect blood pressure meds. Even vitamin K can interfere with warfarin. Your doctor needs to see everything - not just the pills.
How often should I have a medication review?
At least once a year. But if you’re taking five or more medications, or if you’ve had a recent hospital stay or change in health, aim for every six months. Some pharmacies now offer free reviews - ask your pharmacist. Regular reviews reduce unnecessary pills and lower your risk of side effects.
Is it normal for seniors to take so many medications?
It’s common - but not always necessary. About 89% of seniors take at least two prescription drugs, and 15% take five or more. But many of these medications are taken long after their benefit has passed. That’s why reviews matter. The goal isn’t to take fewer drugs for the sake of it - it’s to take only what truly helps you stay healthy and safe.