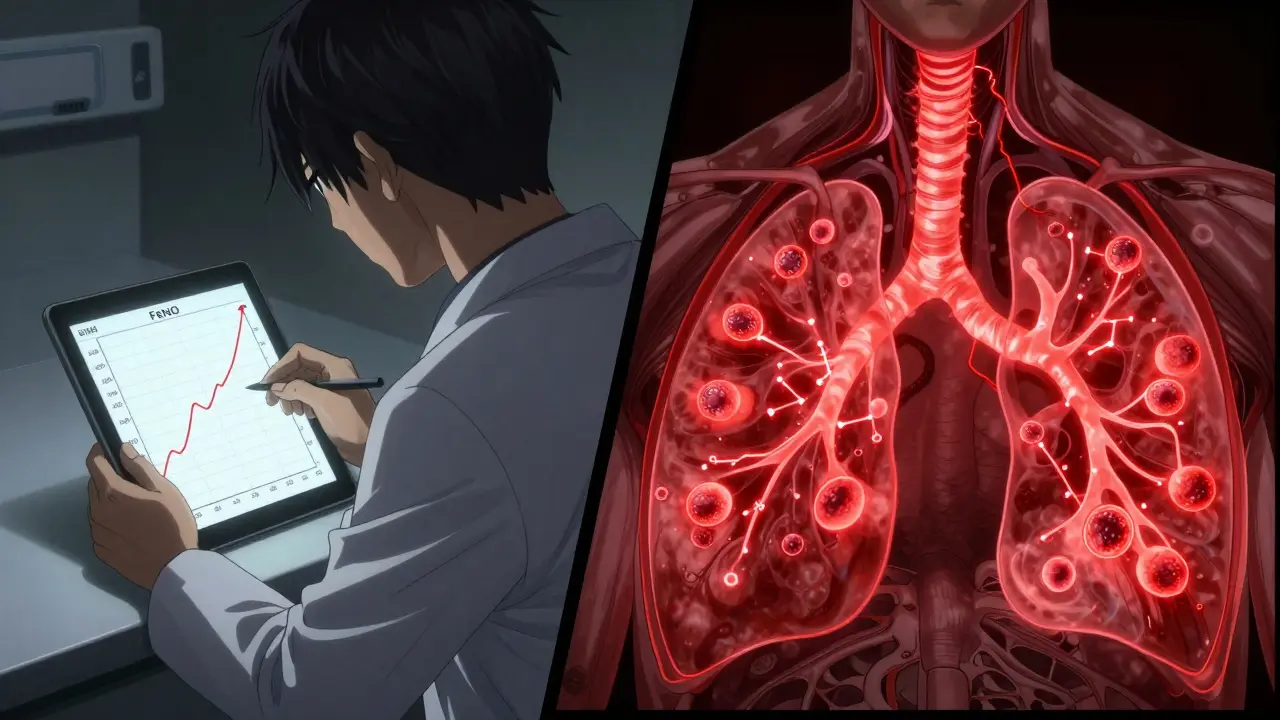
What FeNO Testing Actually Measures
FeNO testing stands for Fractional Exhaled Nitric Oxide testing. It’s a simple, painless way to measure how much nitric oxide is in your breath. This isn’t just any gas - in asthma, high levels of nitric oxide signal active inflammation in your airways. Think of it like a smoke alarm for your lungs. When your airways are swollen and irritated - often because of allergies or eosinophilic inflammation - your body produces more nitric oxide. The test catches that signal.
The device you breathe into looks like a small handheld gadget, similar to a breathalyzer. You take a deep breath through a filter that clears out outside air, then exhale slowly and steadily for about 10 seconds. No coughing, no straining. Just breathe out like you’re gently fogging a mirror. The machine reads the nitric oxide level in parts per billion (ppb). Results come back in under a minute.
Why Doctors Use FeNO for Asthma
Asthma isn’t one-size-fits-all. Some people have allergies triggering their symptoms, others have stress or exercise-induced flare-ups. But when inflammation is driven by eosinophils - a type of white blood cell - FeNO testing shines. High FeNO levels (≥25 ppb in adults, ≥20 ppb in kids 5-12) strongly suggest this type of inflammation.
That matters because corticosteroid inhalers work best on eosinophilic asthma. If your FeNO is high, your doctor can be more confident that your inhaler will help. If it’s low, they might look elsewhere - maybe you’re dealing with non-eosinophilic asthma, which doesn’t respond well to steroids. One study found that using FeNO to guide treatment cuts asthma attacks by up to 50%. That’s not a small win.
How It Compares to Other Tests
You’ve probably had spirometry - blowing hard into a tube to measure lung capacity. That tells you how well your lungs are working right now, but not why they’re not working. FeNO tells you what’s happening inside the airway lining.
Compared to blood tests for eosinophils, FeNO is faster, cheaper, and doesn’t need a needle. Sputum tests are even more accurate but require coughing up phlegm - something most people won’t do willingly. FeNO? Kids as young as five can do it. Elderly patients with weak lungs? No problem. It’s the least invasive way to see if inflammation is driving your symptoms.
But here’s the catch: FeNO won’t catch every kind of asthma. If your flare-ups come from cold air, pollution, or stress without eosinophil involvement, your FeNO level might be normal. That’s why doctors never use it alone. It’s always paired with your symptoms, lung function tests, and medical history.
What Your FeNO Numbers Mean
There’s no single number that says “asthma” - it’s about context. Here’s what the guidelines say:
- Below 25 ppb (adults): Low inflammation. Your asthma may be well-controlled, or you might not have eosinophilic asthma at all.
- 25-50 ppb: Moderate inflammation. This is where treatment adjustments often happen. Your doctor might increase your steroid inhaler dose or consider adding a biologic.
- Over 50 ppb: High inflammation. This strongly suggests uncontrolled eosinophilic asthma. It often means you’re at higher risk for an attack, especially if your symptoms haven’t improved.
These numbers shift if you’re taking steroids. If you’ve just started or stopped your inhaler, your FeNO can drop quickly - sometimes in just a few days. That’s why timing matters. Always do the test before using your rescue inhaler or eating/drinking anything besides water.
Real Stories: When FeNO Changed the Game
One patient in Sydney, 34, had been told for seven years she had chronic bronchitis. She was on antibiotics and cough suppressants - nothing helped. Her FeNO level came back at 48 ppb. That was the clue. She was re-diagnosed with asthma, switched to an inhaled corticosteroid, and within weeks, her nighttime cough vanished. She hasn’t needed an ER visit since.
Another guy on Reddit said his FeNO test showed his levels were rising even though he felt fine. His doctor bumped up his dose before he had a flare-up. He called it “a warning system for my lungs.”
But it’s not perfect. Some people get inconsistent results because they didn’t exhale steadily enough. Others got denied insurance coverage - even after multiple attacks. One woman spent six months fighting her insurer before they approved the test. “They said it wasn’t necessary,” she wrote. “But I was missing work every month.”
Who Should Get Tested - and Who Might Not Need It
FeNO testing is most useful if:
- You’re having trouble controlling asthma with standard inhalers
- Your symptoms don’t match your lung function test results
- You’re being considered for biologic therapy (like dupilumab or benralizumab)
- You’re a child who can’t do spirometry well
- You’ve had frequent asthma attacks despite treatment
It’s less helpful if:
- You smoke - nicotine lowers FeNO levels by 30-50%, masking inflammation
- You have non-allergic asthma triggered by exercise or cold air
- You’re already on high-dose steroids - levels may be artificially low
Also, if you have allergic rhinitis or eosinophilic bronchitis, your FeNO might be high even without asthma. That’s why your doctor needs the full picture.

What’s New in FeNO Testing
In early 2023, the FDA cleared the first smartphone-connected FeNO device. It’s called Breathometer Asthma - a small mouthpiece that plugs into your phone. You can track your levels at home, share trends with your doctor, and get alerts if your inflammation spikes. It’s not covered by insurance yet, but it costs $299 - less than one ER visit.
European guidelines now recommend FeNO to predict who will respond to expensive biologic drugs. That’s huge. These treatments cost over $20,000 a year. If FeNO can tell you ahead of time whether they’ll work, it saves money and avoids months of trial and error.
Still, access is uneven. In the U.S., only 41% of community clinics offer it. In the UK, where NICE guidelines require it, 85% of clinics do. Rural areas lag far behind cities. If your doctor hasn’t mentioned it, ask. It’s not magic - but it’s one of the clearest windows into what’s happening inside your airways.
How to Prepare for the Test
It’s easy - but small mistakes mess up results. Here’s what you need to do:
- Avoid eating, drinking (except water), smoking, or exercising for at least one hour before the test.
- Don’t use your rescue inhaler right before - wait at least 4 hours.
- Don’t do spirometry right before - FeNO must come first.
- Breathe out slowly and steadily. The machine gives you visual feedback - follow the line on the screen.
- Don’t cough or sniff during the exhale. It invalidates the result.
Most clinics will have you try twice. If the readings are close, they’ll average them. If they’re wildly different, they’ll repeat it. That’s normal. The goal is accuracy, not speed.
What Comes After the Test
Your doctor won’t just give you a number and send you home. They’ll look at your FeNO level alongside your symptoms, lung function, medication use, and history. If your FeNO is high and your asthma is still flaring, they might increase your daily steroid dose. If it’s low and you’re still wheezing, they might switch to a different class of drug.
Some patients get tested every 3-4 months. Others only when they’re adjusting treatment. The key is tracking trends over time. A single high reading means little. But if your FeNO climbs month after month, even with no symptoms, that’s a red flag.
There are free online tools - like the Asthma UK FeNO calculator - to help you track your numbers. Write them down. Bring them to every appointment. The more data you have, the better your care becomes.