
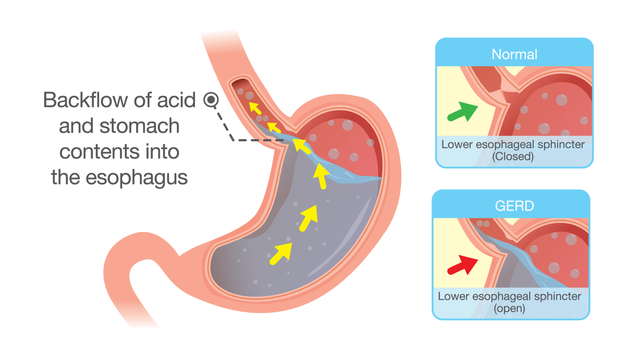
When you switch to a generic drug, you expect the same effect as the brand-name version. But what if your body reacts differently-not because the drug is weaker, but because of your genes? This isn’t science fiction. It’s happening right now, and your family history might hold the key.
Why Your Body Responds Differently to the Same Drug
Not everyone processes medication the same way. Two people taking the exact same generic pill at the same dose can have wildly different outcomes. One feels better. The other gets sick. Why? It’s not about the drug. It’s about your genes.The science behind this is called pharmacogenetics the study of how inherited genetic differences affect how your body responds to medications. Think of your genes as the instruction manual your body uses to break down and use drugs. Some people have manuals with typos. Those typos change how fast or slow your body processes medicine.
Take CYP2D6 a liver enzyme gene that metabolizes about 25% of all prescription drugs, including common antidepressants and painkillers. Over 80 different versions of this gene exist. Some make you a fast metabolizer-you break down the drug too quickly, so it doesn’t work. Others make you a slow metabolizer-you build up too much of the drug, leading to dangerous side effects. A person with two slow versions of CYP2D6 might get serotonin syndrome from a standard dose of sertraline. Their parent likely had the same gene variation.
Your Family’s Drug History Is a Clue
If your mom couldn’t tolerate the generic version of a blood pressure pill, or your dad had a bad reaction to a painkiller, that’s not coincidence. It’s inheritance. Pharmacogenetic traits often run in families. If multiple relatives had bad reactions to the same class of drugs, you’re more likely to have similar issues.For example, if your family has a history of severe side effects from warfarin a blood thinner whose dosing is strongly influenced by CYP2C9 and VKORC1 gene variants, your risk isn’t just higher-it’s predictable. Studies show that people with certain variants in these genes need 30% less warfarin than others. Without knowing this, switching to a generic version could mean a dangerous overdose.
Same goes for 5-fluorouracil a chemotherapy drug that can cause life-threatening toxicity in people with DPYD gene mutations. A patient in a 2023 Reddit thread shared that after their Color Health test revealed a DPYD variant, their oncologist cut their dose by one-third. They finished chemo without the severe diarrhea and low blood counts that killed others in their treatment group. That test didn’t come out of nowhere-it came from family history.
Population Differences Matter More Than You Think
Your ancestry isn’t just about where your family came from-it affects how your body handles drugs. A 2024 study in Nature Scientific Reports found that genetic variants affecting drug response vary dramatically between populations.For example, about 15-20% of Asians are poor metabolizers of proton pump inhibitors (like omeprazole) due to CYP2C19 variants. That means generic versions of these drugs often don’t work well for them. Meanwhile, 2-5% of Caucasians have the same issue. If your doctor prescribes the same dose based on average guidelines, you’re at risk.
African Americans typically need higher doses of warfarin than Europeans because of differences in VKORC1 and CYP2C9 genes. But many prescriptions still use one-size-fits-all dosing. Switching to a generic doesn’t change the drug’s chemistry-it just removes the brand name. Your body still responds based on your genes.
Genetic Testing Is Already Here-But Not Everyone Uses It
The FDA has updated over 300 drug labels to include pharmacogenetic information. That includes common generics like clopidogrel, statins, and antidepressants. But here’s the catch: most doctors don’t check your genes before prescribing.Why? Because it’s not routine. A 2022 survey of 1,247 clinicians showed that while 68% felt confident reading CYP2D6 results, only 32% felt confident about HLA-B*15:02 (which predicts severe skin reactions to carbamazepine). And 79% said they didn’t have time to use the data.
But some hospitals are changing that. Mayo Clinic’s preemptive testing program tested 10,000 patients and found 42% had at least one high-risk gene-drug interaction. Of those, 67% had their meds changed-and adverse events dropped by 34%. That’s not a small win. That’s life-saving.
Testing isn’t expensive anymore. Companies like Color Genomics and OneOme offer multi-gene panels for under $250. Some insurance plans cover it. And if you’ve had a bad reaction to a generic drug before, it’s worth asking your doctor: “Could this be genetic?”
What You Can Do Right Now
You don’t need a lab report to start protecting yourself. Here’s how to take control:- Ask your family: Who had bad reactions to medications? Which ones? Write it down. Even vague answers help.
- Check your prescriptions: Look at the drug label. If it mentions “CYP2D6,” “CYP2C19,” or “TPMT,” your genes matter.
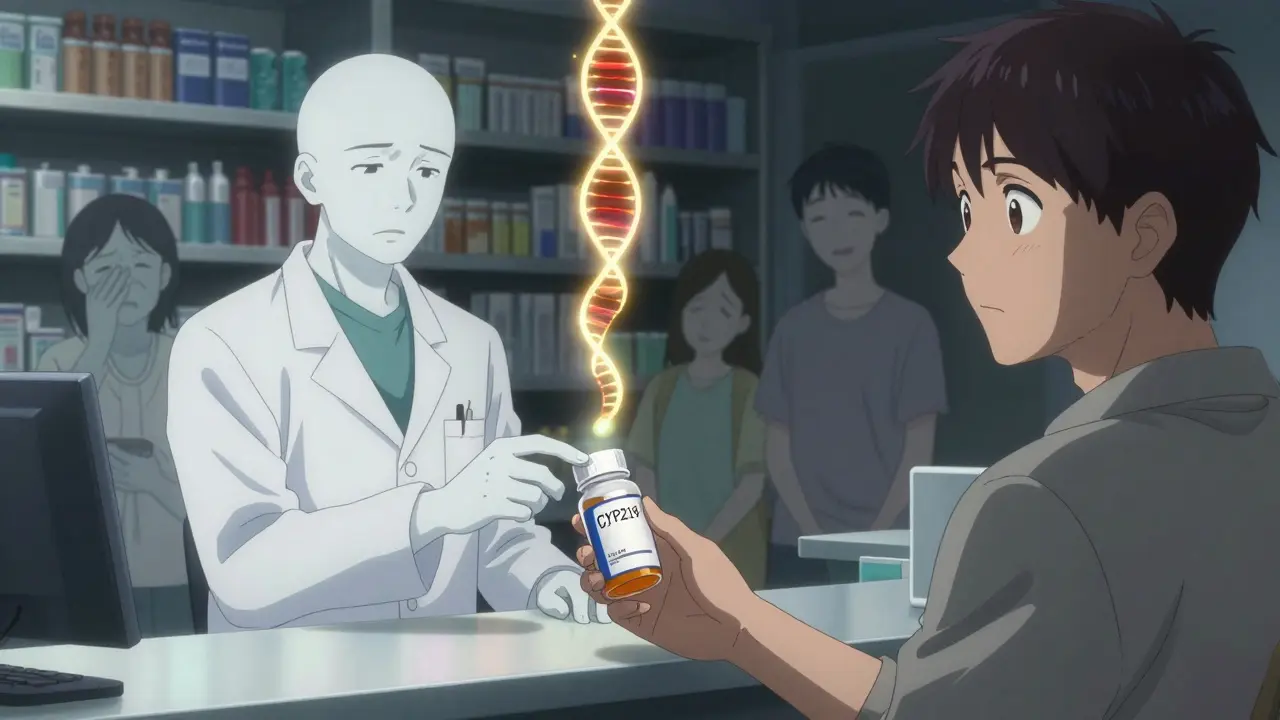
- Ask your pharmacist: They’re trained to spot gene-drug conflicts. Say: “I’m switching to a generic. Could my genes affect how it works?”
- Request testing if you’ve had side effects: If a generic made you dizzy, nauseous, or caused a rash, get tested. It’s not paranoia-it’s prevention.
- Keep a drug reaction log: Note the drug, dose, reaction, and date. This helps your doctor spot patterns over time.
The Future Is Personalized, Not Generic
The push for generic drugs was meant to save money. But if a cheap pill makes you sick, you’re not saving anything-you’re paying in hospital visits, missed work, and pain.Pharmacogenetics is shifting the game. Instead of guessing what dose you need, we can now know. Instead of hoping a generic works, we can predict whether it will.
By 2025, 92% of academic medical centers plan to expand genetic testing programs. The NIH spent $127 million in 2023 just to study how genes affect drug response in underrepresented populations. That’s not a trend. That’s a revolution.
Switching to generics isn’t wrong. But ignoring your genes? That’s risky. Your family history isn’t just stories-it’s a warning system. And if you’ve ever had a drug that didn’t work-or made you worse-you already know how important this is.
Can family history alone tell me how I’ll react to a generic drug?
Family history gives you strong clues-if multiple relatives had bad reactions to the same drug, you’re at higher risk. But it’s not a substitute for genetic testing. Some gene variants aren’t obvious from family patterns, especially if relatives didn’t take the drug or had mild reactions. Testing confirms what history suggests.
Do all generic drugs have the same genetic risks as brand-name ones?
Yes. Generic drugs contain the same active ingredient as brand-name versions, so they interact with your genes the same way. The difference is in inactive ingredients like fillers or dyes, which rarely affect metabolism. If your body reacts poorly to a brand-name drug because of your genes, the generic will likely do the same.
Is pharmacogenetic testing covered by insurance?
Sometimes. Medicare covers certain tests under the Molecular Diagnostic Services Program, especially for high-risk drugs like warfarin or chemotherapy agents. Private insurers vary-some cover testing if you’ve had a prior adverse reaction. Always check with your provider before ordering.
What if my doctor ignores my genetic test results?
Ask for a referral to a clinical pharmacist or pharmacogenetics specialist. Many hospitals have these experts. You can also share the Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines-these are the gold standard and are cited by the FDA. If your doctor refuses, consider switching providers.
How long does it take to get genetic test results for drug response?
Most commercial tests take 7-14 days. Some hospitals with in-house labs can return results in 3-5 days. If you’re starting a new medication with high genetic risk (like chemo or blood thinners), ask if expedited testing is available.




Patrick Jarillon
February 9, 2026 AT 20:33Okay, but let’s be real-this whole pharmacogenetics thing is just Big Pharma’s way of making you pay for tests so they can sell you MORE expensive drugs under a different label. 🤡
They don’t care if your genes are weird-they care if your wallet is full. I got my 23andMe results last year, and guess what? I’m a ‘super metabolizer’ of everything. So now I’m supposed to pay $200 for a test that tells me what my body already proved by surviving 12 different antibiotics in college? Nah. I’ll take my chances with the generic. The real conspiracy? They won’t tell you that generics are sometimes made in the same factories as brand names. Same pills. Different sticker.
Also, CYP2D6? Please. I’ve been on 7 antidepressants. I know my body better than any algorithm. If you’re scared of generics, maybe you’re just scared of saving money.
And don’t get me started on ‘family history.’ My uncle died from a heart attack after taking lisinopril. So now I’m supposed to believe my 17-year-old cousin’s future meds are pre-determined by that? That’s not science. That’s astrology with a lab coat.