Before you write a prescription, you need to know if the drug is covered - and how much the patient will actually pay. It’s not just about what’s clinically right. It’s about what’s covered, what requires prior authorization, and whether the patient can afford it at the pharmacy counter. Skipping this step leads to delays, abandoned prescriptions, and frustrated patients. In 2025, with Medicare Part D covering over 50 million people and commercial insurers constantly updating their drug lists, checking formularies isn’t optional - it’s part of the job.
What Exactly Is a Formulary?
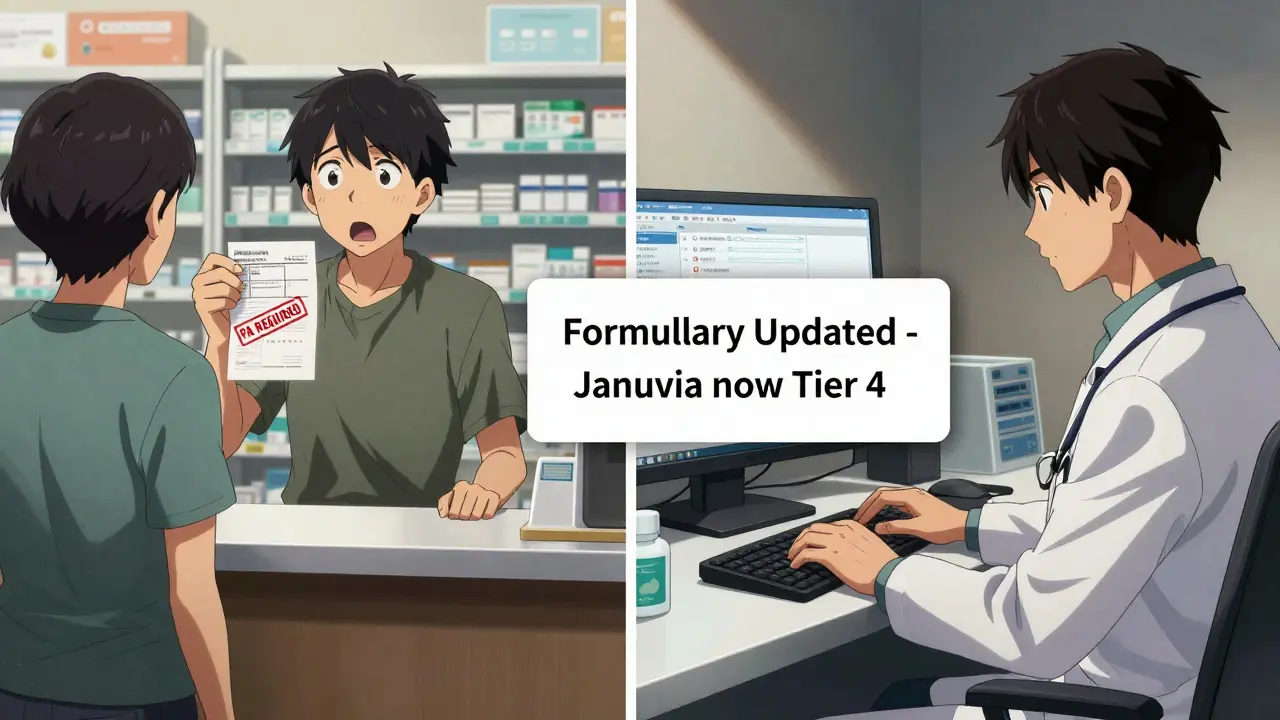
A formulary, also called a Preferred Drug List (PDL), is a list of medications that a health plan covers. It’s not random. Each drug is chosen by a committee of doctors and pharmacists who review clinical data, safety records, and cost. The goal? To make sure patients get effective drugs without unnecessary spending. These lists are updated regularly. Medicare Part D plans must give 60 days’ notice before removing a drug or raising costs. Many insurers like HealthPartners update theirs quarterly - in January, April, July, and October. That means a drug covered last month might need prior authorization next month. You can’t rely on memory. You need to check.How Formularies Are Structured: The Tier System
Most formularies use a tier system to show how much patients pay. The lower the tier, the cheaper the drug. Here’s how it typically breaks down:- Tier 1: Preferred generics - often $1 to $5 per prescription.
- Tier 2: Other generics - maybe $10 to $20.
- Tier 3: Preferred brand-name drugs - $30 to $60.
- Tier 4: Non-preferred brands - $70 to $150 or more.
- Tier 5: Specialty drugs - anything over $950/month. Patients pay a percentage, not a flat copay.
What Those Letters Mean: PA, ST, QL
Every drug on a formulary has symbols next to it. These aren’t random. They’re rules you must follow.- PA (Prior Authorization): The plan won’t cover the drug unless you submit paperwork proving it’s medically necessary. This can take hours - or days.
- ST (Step Therapy): You have to try a cheaper drug first. If it doesn’t work, then you can move up. Many patients get stuck because the first drug causes side effects or fails completely.
- QL (Quantity Limit): The plan only covers a certain amount per month. For example, you can only prescribe 30 pills of a painkiller, even if the patient needs 60.
How to Check a Formulary: 4 Reliable Methods
You don’t need to guess. There are clear, fast ways to check coverage before you write the script.- Use the insurer’s online drug search tool. Most major insurers - Aetna, UnitedHealthcare, Humana - have searchable databases. You need the patient’s plan name, zip code, and drug name. Aetna’s tool, for example, shows tier level, PA requirements, and alternatives in real time. In a July 2024 MGMA survey, 74% of providers called it "very helpful."
- Check your EHR system. Hospitals and large clinics use integrated tools like Epic’s Formulary Check. Northwestern Medicine cut prescription abandonment by 42% after adding it. If your practice has this, use it. It pops up as you type a drug name.
- Call the insurer’s provider line. Every Medicare Part D plan has a 24/7 provider hotline. You can ask: "Is this drug covered under plan XYZ? Does it need PA?" Most calls take under 3 minutes.
- Use CMS Plan Finder. For Medicare patients, this free tool covers 99.8% of Part D plans. Just enter the patient’s zip code, date of birth, and drug name. It shows cost, tier, and restrictions. It’s the most complete public resource.
Differences Between Medicare, Medicaid, and Commercial Plans
Not all formularies are the same. Knowing the differences saves you time.- Medicare Part D: Always five tiers. Must cover at least two drugs per therapeutic class. Must offer exceptions. Updates happen January 1 each year, with mid-year changes allowed if patients are notified 60 days ahead.
- Medicaid: Each state sets its own PDL. 42 states use closed formularies - meaning you can’t prescribe a non-listed drug without prior authorization. Minnesota’s DHS, for example, created a single statewide list for all Medicaid members.
- Commercial plans: More flexible. UnitedHealthcare uses four tiers. Some have no specialty tier. Others use step therapy more aggressively. They’re not bound by Medicare rules.
Why This Matters: Real Impact on Patients
A 2023 Sermo survey of 1,247 U.S. doctors found that 68% spend 10 to 20 minutes per patient just checking drug coverage. Primary care physicians spend nearly 19 minutes - almost a third of a typical 60-minute visit. But the real cost isn’t time. It’s outcomes. When a patient can’t afford their medication, they skip doses. Or stop entirely. A 2024 study showed that 34% of prior authorization delays led to serious adverse events - hospitalizations, worsening conditions, even deaths. On the flip side, clinics that use EHR-integrated formulary tools report fewer refills, fewer calls to the pharmacy, and higher patient satisfaction. It’s not just about compliance. It’s about keeping people healthy.What’s Changing in 2025 and Beyond
The Inflation Reduction Act’s $2,000 annual cap on out-of-pocket drug costs for Medicare Part D starts in 2025. That’s forcing insurers to rethink formularies. Already, 73% of 2025 Medicare formularies are moving more drugs to lower tiers to help patients hit the cap faster. New technology is coming too. Epic’s FormularyAI, launched in August 2024, uses machine learning to predict whether a drug will be approved - with 87% accuracy. It analyzes 10 million past prior authorization decisions. That’s not science fiction. It’s here. By January 1, 2026, CMS requires all Medicare Part D plans to offer real-time benefit tools (RTBT) that feed formulary data directly into EHRs. If you’re not using an EHR with this built-in, you’ll be at a disadvantage.
Pro Tips for Daily Practice
Here’s what works in real clinics:- Bookmark the formulary pages for your top 5 insurers. Keep them on your browser toolbar.
- Set calendar reminders for quarterly updates - January, April, July, October.
- Always check before prescribing - even if you’ve prescribed the same drug before. Plans change.
- Use alternatives when possible. If a Tier 4 drug needs PA, ask: "Is there a Tier 1 or 2 that works just as well?"
- Teach your staff to do the first check. Let them pull up the formulary while you’re with the patient.
What to Do When a Drug Isn’t Covered
If the drug your patient needs isn’t on the formulary, don’t just give up. You have options.- Submit a prior authorization request. Include clinical notes, failed alternatives, and evidence of need. Medicare requires a response within 72 hours - 24 hours if it’s urgent.
- Ask for a formulary exception. If the patient has a documented reason - like an allergy or previous failure - you can request the drug be added temporarily.
- Try a therapeutic substitute. Sometimes a different drug in the same class works just as well. Check the formulary for alternatives first.
- Connect with the pharmacy. Pharmacists often know about pending formulary changes or manufacturer coupons you didn’t know about.
Final Thought: This Isn’t Bureaucracy - It’s Care
Checking formularies isn’t paperwork. It’s part of prescribing. You’re not just choosing a drug. You’re choosing a treatment path that includes cost, access, and real-world barriers. The best medicine is the one the patient can actually take. In 2025, with drug costs still rising and rules constantly shifting, skipping this step isn’t efficiency - it’s negligence. Take the 3 minutes. Check the list. Save your patient from a surprise bill or a missed dose. That’s what good care looks like now.What is a formulary and why does it matter when prescribing?
A formulary is a list of medications covered by a patient’s health insurance plan. It’s created by doctors and pharmacists to balance effectiveness and cost. It matters because if a drug isn’t on the list, the patient may pay full price, get denied coverage, or face delays due to prior authorization. Prescribing without checking can lead to patients skipping doses or abandoning prescriptions entirely.
How often do formularies change?
Medicare Part D plans must update formularies by January 1 each year, with mid-year changes allowed if patients are notified 60 days in advance. Many commercial insurers update quarterly - typically in January, April, July, and October. HealthPartners and other major plans publish these updates publicly. Always verify before prescribing, even if you’ve prescribed the same drug last month.
What do PA, ST, and QL mean on a drug list?
PA means Prior Authorization - you need to submit paperwork before the plan will cover the drug. ST means Step Therapy - you must try a cheaper drug first. QL means Quantity Limit - the plan only covers a set amount per month, like 30 pills even if the patient needs 60. These are rules you must follow, or the prescription will be denied at the pharmacy.
Can I prescribe a drug that’s not on the formulary?
Yes, but the patient will likely pay full price unless you file a prior authorization or formulary exception. Some plans - especially Medicaid - are "closed," meaning non-formulary drugs are rarely approved. Always check the plan’s exceptions process first. If the drug is medically necessary and alternatives have failed, you can request coverage.
What’s the fastest way to check a formulary during a patient visit?
Use your EHR’s built-in formulary checker if available. If not, pull up the insurer’s online drug search tool on a second screen. For Medicare patients, CMS Plan Finder is free and covers nearly every plan. Aetna’s and UnitedHealthcare’s tools are highly rated for speed and clarity. Most checks take under 90 seconds if you have the patient’s plan name and zip code ready.
Are there tools that predict if a drug will be covered?
Yes. Epic Systems launched FormularyAI in August 2024, which uses machine learning to predict coverage likelihood with 87% accuracy based on 10 million past prior authorization decisions. It’s already integrated into some EHRs. By 2026, CMS requires all Medicare Part D plans to offer real-time benefit tools that push formulary data directly into your clinical workflow.
How does the $2,000 out-of-pocket cap in Medicare Part D affect formularies in 2025?
The cap means insurers are moving more drugs to lower tiers to help patients reach the limit faster. In 2025, 73% of Medicare Part D formularies have shifted brand-name drugs from Tier 4 to Tier 3 or even Tier 2. This reduces patient costs and increases adherence. It’s also making prior authorization less common for high-cost drugs, since plans now want patients to use them before hitting the cap.
What should I do if a patient can’t afford their medication even if it’s covered?
Ask the pharmacy about manufacturer coupons or patient assistance programs. Many drugmakers offer free or discounted medications for low-income patients. Also, check if a therapeutic alternative exists on a lower tier. Sometimes switching to a generic or another brand in the same class cuts costs dramatically without losing effectiveness. Never assume a patient will pay - always ask about affordability.




Blow Job
December 24, 2025 AT 06:19This is the kind of stuff that actually saves lives. I used to skip checking formularies because I thought it was bureaucracy, but after a patient ended up in the ER because they couldn't afford their insulin, I changed everything. Now I check before I even open the chart. Three minutes. That's all it takes. Do it.
niharika hardikar
December 24, 2025 AT 21:00It is imperative to underscore that the clinical governance of pharmaceutical formularies constitutes a non-negotiable pillar of evidence-based prescriptive practice. Failure to consult Preferred Drug Lists prior to initiating therapy constitutes a deviation from the standard of care, particularly in light of the escalating fiscal constraints imposed by third-party payers. The tiered structure, coupled with prior authorization mandates, is not an administrative inconvenience-it is a structural necessity for fiscal sustainability within the healthcare ecosystem.
John Pearce CP
December 26, 2025 AT 17:34Anyone who thinks checking formularies is "extra work" hasn't been paying attention. We're not in the business of giving patients prescriptions they can't afford. That's not medicine-that's malpractice dressed up as efficiency. The fact that we still have to beg insurers for basic coverage in 2025 is a national disgrace. If you're not using Epic's FormularyAI by now, you're not just behind-you're endangering people.
EMMANUEL EMEKAOGBOR
December 27, 2025 AT 17:56While I appreciate the comprehensive overview presented herein, I must respectfully note that the global applicability of these formulary systems remains limited to high-income healthcare contexts. In Nigeria, where formularies are often nonexistent or inconsistently enforced, the challenge lies not in navigating tiers but in securing any medication at all. Perhaps the conversation should expand to include equitable access beyond insurance frameworks.
suhani mathur
December 27, 2025 AT 23:00Oh wow, you mean I’m supposed to *check* before I write? What a wild concept. Next you’ll tell me I should wash my hands before surgery. /s
But seriously-this is the most useful thing I’ve read all year. I’ve been using CMS Plan Finder on my phone during rounds. My patients actually thank me now. Who knew?
Jillian Angus
December 28, 2025 AT 09:33Just checked my formulary tool and my favorite med for hypertension just got moved to tier 4
and it’s a $200 copay now
nope
not doing that to my 72 year old
Ademola Madehin
December 30, 2025 AT 07:24MY PATIENT GOT DENIED FOR HER CANCER DRUG AGAIN AND I HAD TO CALL THREE TIMES AND SEND SIX PAGES OF DOCUMENTS AND SHE CRIED IN THE CHAIR BECAUSE SHE THOUGHT SHE'D DIE BECAUSE THE INSURANCE WASN'T COOPERATING
AND NOW I HAVE TO DO THIS EVERY SINGLE DAY
WHY IS THIS ON ME
WHY
WHY
WHY
CHETAN MANDLECHA
December 31, 2025 AT 08:30Been doing this for 12 years. The real game-changer? Teaching your MA to run the formulary check while you're in the room. Saves 10 minutes per patient. You still get to make the call. They just do the grunt work. My clinic cut prescription abandonment by half. No magic. Just teamwork.