Low-FODMAP Food Checker
Identify which foods may be triggering both your IBS and eczema symptoms. Based on clinical evidence showing 20% reduction in eczema severity with FODMAP elimination.
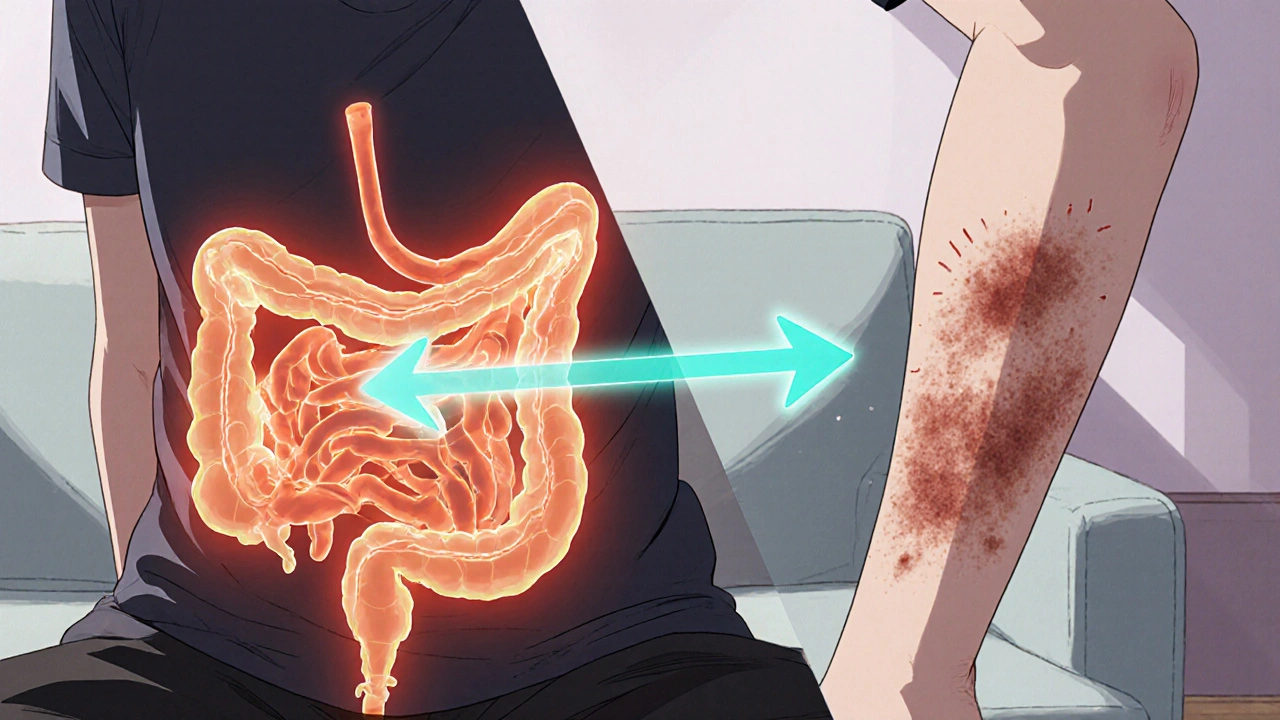
Ever wondered why a bad tummy day often ends with an itchy rash? Understanding the link between eczema and IBS can change how you treat both. The gut‑skin axis is a two‑way street: what happens in your intestines can flare up your skin, and skin inflammation can worsen digestive symptoms.
What Is Eczema?
Eczema is a chronic inflammatory skin condition marked by dry, red, and intensely itchy patches. It affects up to 20% of children and about 3% of adults worldwide. Triggers range from allergens and irritants to stress and temperature changes.
What Is Irritable Bowel Syndrome?
Irritable Bowel Syndrome is a functional gastrointestinal disorder causing abdominal pain, bloating, and altered bowel habits without a structural cause. Roughly 10‑15% of the global population lives with IBS, with women reporting symptoms more often than men.
The Gut‑Skin Axis: How the Gut Influences Eczema
Scientists call the communication pathway between the intestines and the skin the gut‑skin axis. Three major mechanisms drive the connection:
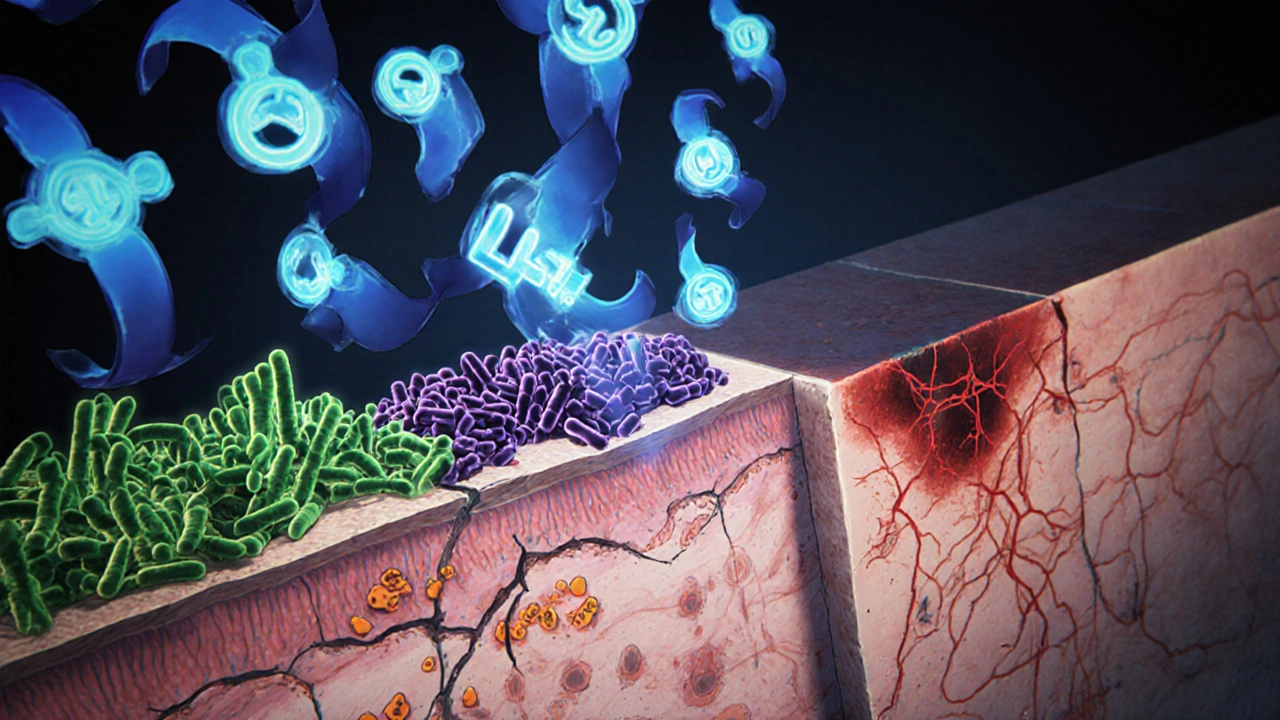
- Gut Microbiome - A healthy mix of bacteria ferments fiber, produces short‑chain fatty acids, and trains the immune system. Dysbiosis (an imbalance) can tip the immune response toward inflammation, which shows up on the skin.
- Leaky Gut - When the intestinal lining becomes more permeable, bacterial fragments and food antigens slip into the bloodstream, prompting systemic immune activation and the release of inflammatory cytokines that aggravate eczema.
- Inflammatory Cytokines - Molecules like interleukin‑4 (IL‑4) and interleukin‑13 (IL‑13) rise in both IBS flare‑ups and eczema outbreaks, creating a feedback loop that fuels both conditions.
Shared Triggers: Food Sensitivities, Stress, and More
Both conditions often react to the same external factors:
- Food Sensitivities - Lactose, gluten, and certain FODMAPs can provoke gut distress and also trigger eczema patches in susceptible people.
- Stress Hormones - Cortisol spikes increase gut permeability and skin itching, making stress a common aggravator.
- Environmental allergens - Dust mites and pet dander can irritate the skin while also affecting gut motility in some individuals.
Clinical Evidence Linking Eczema and IBS
Recent studies help cement the gut‑skin link:
- A 2023 longitudinal cohort of 5,000 adults found that those diagnosed with IBS had a 38% higher odds of developing eczema within three years (OR = 1.38, 95% CI 1.22‑1.55).
- Microbiome sequencing in 2022 revealed that IBS patients with eczema shared a depletion of Bifidobacterium and an overgrowth of Staphylococcus aureus on the skin.
- Intervention trials using a low‑FODMAP diet showed simultaneous improvement in abdominal pain scores and a 20% reduction in eczema severity index (EASI) after eight weeks.
Practical Steps to Manage Both Conditions
Here’s a road‑map you can start today:
- Identify Food Triggers - Keep a 2‑week food and symptom diary. Note any correlation between meals, bloating, and skin flare‑ups.
- Try a Low‑FODMAP Diet - Under a dietitian’s guidance, eliminate high‑FODMAP foods (wheat, onions, garlic, beans) for 4‑6 weeks. Re‑introduce one at a time to see what sticks.
- Boost the Gut Microbiome - Incorporate fermented foods (yogurt, kefir, kimchi) and consider a probiotic containing Lactobacillus rhamnosus GG or Bifidobacterium infantis. Aim for 10‑12 billion CFU daily.
- Mind the Skin Care Routine - Use gentle, fragrance‑free cleansers. Apply a moisturizer within three minutes of showering to lock in moisture. For flare‑ups, a short course of topical steroids or calcineurin inhibitors can break the itch‑scratch cycle.
- Manage Stress - Mind‑body practices like yoga, meditation, or deep‑breathing reduce cortisol, improve gut motility, and calm itching.
- Stay Hydrated - Aim for at least 2 L of water a day; proper hydration supports both gut barrier function and skin elasticity.

When to Seek Professional Help
If you notice any of the following, schedule an appointment with a dermatologist or gastroenterologist:
- Rapidly spreading rash or signs of infection (pus, fever).
- Severe abdominal pain, unintentional weight loss, or blood in stool.
- Persistent symptoms despite lifestyle changes for more than 8 weeks.
These red flags may indicate an underlying condition that needs prescription‑level treatment or further testing.
Quick Reference Table: Common Triggers for IBS vs. Eczema
| Trigger | IBS Impact | Eczema Impact |
|---|---|---|
| Gluten | Cramping, bloating | Itching, flare‑up |
| Lactose | Diarrhea, gas | Dry patches |
| Stress | Increased motility | Heightened itch |
| Dust mites | May worsen gut motility | Direct skin allergen |
| Spicy foods | Irregular bowel movements | Heat‑induced redness |
Frequently Asked Questions
Can probiotics really help both IBS and eczema?
Yes. Strains like Lactobacillus rhamnosus GG have been shown in randomized trials to reduce abdominal pain scores by 30% and lower eczema severity scores by about 15% after 12 weeks.
Is the low‑FODMAP diet safe for children with eczema?
When overseen by a pediatric dietitian, a low‑FODMAP approach can be safe. It should be short‑term (4‑6 weeks) and followed by a gradual re‑introduction phase to prevent nutritional gaps.
Do I need to eliminate dairy completely?
Not always. Start with a trial elimination of lactose‑containing products for two weeks. If symptoms improve, re‑introduce them slowly while monitoring both gut and skin responses.
How long does it take to see skin improvement after diet changes?
Most people notice a reduction in itching within 2‑4 weeks, with visible redness fading after 6‑8 weeks, provided the trigger has been removed.
Should I still use topical steroids while fixing my gut?
Short‑term use (1‑2 weeks) of low‑potency steroids can control acute flare‑ups, but the goal is to wean off them as gut‑focused treatments take effect.





Marrisa Moccasin
October 22, 2025 AT 15:16Don't trust the mainstream narrative-your gut is being manipulated by hidden chemicals in processed foods!!!
Caleb Clark
October 22, 2025 AT 16:06I totally get how overwhelming it can feel when you realize that the gut‑skin axis is basically a constant battle zone in your own body.
First off, start logging everything you eat, even the tiniest snacks, because the patterns are usually hidden in the details.
You’ll be shocked when that late‑night pizza shows up right before a nasty eczema flare‑up the next morning.
I recommend grabbing a simple notebook or a phone app-whatever keeps you consistent, even if you miss a day.
Next, give the low‑FODMAP diet a serious shot, but do it under the guidance of a qualified dietitian so you don’t miss out on essential nutrients.
While you’re at it, toss in some fermented goodies like kefir or kimchi; those probiotic powerhouses can actually shift the microbiome balance toward the good guys.
Don’t forget to stay hydrated-water is the unsung hero that helps keep your gut lining airtight, which in turn protects your skin.
Stress is another sneaky player, so try meditating for five minutes a day or even a quick breathing exercise when you feel the itch coming on.
If you’re into yoga, the restorative poses can calm both the gut and the nerves, making the whole system less reactive.
When it comes to skin care, keep it simple: fragrance‑free cleansers, a thick moisturizer right after showering, and a short course of low‑potency steroids only if the rash is out of control.
I’ve seen people cut their eczema severity in half just by pairing diet changes with a steady skincare routine, so don’t underestimate the synergy.
Also, keep an eye on hidden triggers like gluten or dairy; sometimes a two‑week elimination can reveal a culprit you never suspected.
If you’re skeptical about probiotics, look for strains like Lactobacillus rhamnosus GG-studies show they can lower both gut pain and skin itchiness.
Remember, consistency is key; you won’t see dramatic results overnight, but a month of diligent tracking will give you solid data.
And finally, be kind to yourself-this isn’t a punishment, it’s a journey toward feeling better both inside and out.
Stick with it, and you’ll probably notice that your skin calms down before your gut even fully settles, which is a huge win.
Oliver Johnson
October 22, 2025 AT 17:13All this talk about gut health is just another excuse to push a foreign agenda on our bodies. It’s nothing but hype.
Mary Keenan
October 22, 2025 AT 18:20Honestly, this whole diet thing sounds like a scam-why would anyone waste time on fad foods when creams work?
Kelly Brammer
October 22, 2025 AT 19:43While topical treatments provide temporary relief, addressing underlying inflammation through diet yields more sustainable outcomes.
Ben Collins
October 22, 2025 AT 21:06Sure, because adding kimchi to your lunch is definitely easier than just slapping on another steroid.
Denver Bright
October 22, 2025 AT 23:03I get that, but even a tiny tweak in your gut can calm the itch without the endless pharmacy trips.
Kelli Benedik
October 23, 2025 AT 01:16OMG, I've been battling this nightmare for months!!! 😩 The flare‑ups feel like fire on my skin and the belly pain is relentless!!! 🌶️
cariletta jones
October 23, 2025 AT 04:03Try a short low‑FODMAP trial and see if it eases both symptoms.
Kevin Hylant
October 23, 2025 AT 06:50Tracking food and symptoms is the best way to spot patterns and make real changes.
Holly Green
October 23, 2025 AT 09:36Absolutely, a systematic diary can reveal hidden triggers and empower you to take control.