
Why Diabetic Foot Care Isn’t Just a Checklist - It’s a Lifesaver
Every year, over 82,000 people in the U.S. lose a foot or leg to diabetes-related amputation. Most of these aren’t sudden tragedies. They’re the end result of a small cut, blister, or sore that went unnoticed - because the nerves in the foot stopped sending pain signals. This isn’t rare. About 1 in 4 people with diabetes will develop a foot ulcer in their lifetime. The good news? Almost all of them are preventable - if you know what to look for, when to look, and how to act.
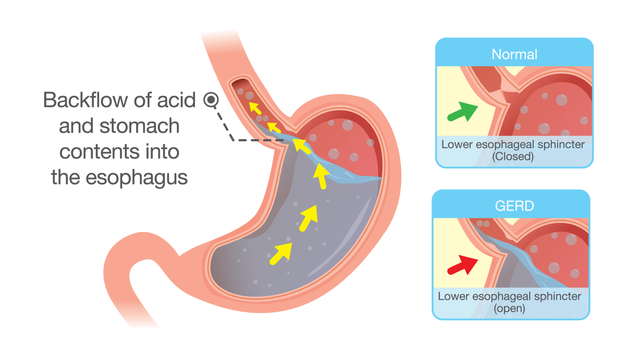
The Real Risk: It’s Not Just About Blood Sugar
High blood sugar damages nerves and blood vessels over time. That’s why people with diabetes lose feeling in their feet - a condition called peripheral neuropathy. You might step on a sharp rock, develop a blister from tight shoes, or scratch your skin while scratching an itch - and feel nothing. At the same time, poor circulation means even small wounds don’t heal well. What starts as a tiny crack in the skin can turn into a deep ulcer in days.
The International Working Group on the Diabetic Foot (IWGDF) classifies risk into four levels:
- Risk 0: No nerve damage, no history of foot problems - annual checkups are enough.
- Risk 1: Nerve damage but no foot deformities - check every 6 months.
- Risk 2: Nerve damage plus foot deformities (like bunions or hammertoes) - check every 1-3 months.
- Risk 3: Past ulcer or amputation - check monthly or more, and treat every change like an emergency.
If you’re in Risk 2 or 3, daily inspection isn’t optional. It’s your last line of defense.
Your Daily Foot Inspection Checklist (The 7-Step Protocol)
There’s no magic tool or app that replaces a careful, consistent look at your feet. The standard from NYU Langone and the CDC is simple, but it must be done right - every single day.
- Wash in lukewarm water. Use water between 90-95°F (32-35°C). Test it with your elbow or a thermometer. Hot water burns skin that can’t feel heat.
- Dry thoroughly. Pay special attention to the spaces between your toes. Moisture there invites fungal infections, which can crack the skin and lead to ulcers.
- Look at every surface. Use a hand mirror or ask someone to help. You need to see the soles, heels, and between toes. Don’t guess. Look. The University of Michigan found that 92% of plantar ulcers form under the ball of the foot - right where pressure builds when you walk.
- Spot the warning signs. Look for:
- Blisters larger than 3mm
- Cuts or scrapes deeper than 1mm
- Redness spreading beyond 1cm
- Swelling that makes your foot feel tighter than usual
- Warmth in one spot - if one foot feels hotter than the other, that’s a red flag
- Ingrown toenails or thick, yellow nails (signs of fungus)
- Moisturize - but not between toes. Dry skin cracks. Use unscented lotion on tops and soles. Never put it between toes - that traps moisture and invites infection.
- Trim nails straight across. Cut them so they’re just above the skin fold - about 1-2mm. Don’t round the edges. Don’t dig under the nail. If you can’t see well or have thick nails, see a podiatrist.
- Do it at the same time every day. The CDC found that 68% of ulcers start from unnoticed injuries because inspections are inconsistent. Do it in the morning, after your shower, or before bed - but stick to it. Natural light between 10 a.m. and 2 p.m. gives the clearest view of color changes.

Footwear: The Silent Enemy (And Your Best Protector)
Shoes are the #1 cause of diabetic foot ulcers. Not because they’re bad - but because most people wear the wrong ones.
The IWGDF says 87% of forefoot ulcers and 79% of midfoot ulcers come from shoes that press too hard. You don’t need expensive orthopedic shoes unless you’re at high risk - but you do need the right fit.
- Leave at least 0.5 inches (12.7mm) between your longest toe and the front of the shoe.
- Your toes should be able to wiggle sideways - no squeezing.
- Heels should be firm, not floppy. A good heel counter holds your foot without pinching.
- Never walk barefoot - even indoors. The CDC says walking barefoot for just 5 minutes a day increases ulcer risk by 11 times.
- Avoid flip-flops, sandals, or open-back shoes. They offer no support and expose your feet to cuts and burns.
And don’t be fooled by summer heat. When temperatures hit 89°F+, many people switch to sandals. Pressure mapping studies show this increases ulcer risk by 4.3 times. Wear breathable, closed-toe shoes even in summer.
What Not to Do (The Myths That Hurt)
There’s a lot of bad advice out there.
- Don’t use corn removers or chemical peels. These can burn your skin. Even over-the-counter wart removers are dangerous.
- Don’t soak feet for long periods. Soaking dries out skin and softens it too much, making it easier to tear.
- Don’t try to cut calluses yourself. Calluses are your body’s way of protecting pressure points. If they’re thick, see a podiatrist. Cutting them can create deep wounds.
- Don’t rely on feeling pain. If you have neuropathy, pain isn’t a reliable warning. No pain doesn’t mean no problem.
- Don’t use antibiotics for uninfected wounds. The IDSA says antibiotic prophylaxis doesn’t help healing - and increases the risk of drug-resistant infections.
When to See a Professional - Don’t Wait
You don’t need to panic over every little bump. But if you see any of these, call your doctor or podiatrist within 24 hours:
- Redness that spreads
- Swelling that doesn’t go down after a day
- Drainage or pus
- A wound that doesn’t start healing in 2-3 days
- Any change in foot shape (new arch, bent toe)
For people at Risk 2 or 3, a full foot exam by a podiatrist should happen every 1-3 months. If you have poor circulation (ankle-brachial index below 0.9), you need a vascular specialist too.

Barriers Are Real - But You Can Beat Them
Studies show only 42% of people with diabetes do daily foot checks. Why? Vision problems, nerve damage, lack of help, or just forgetting. If you can’t see your feet well, get a mirror with a long handle. Ask a family member to help. Set a daily phone alarm. Put your inspection checklist on the bathroom mirror.
Cost is another issue. Smart socks or pressure-sensing mats can detect ulcers before they form - but they cost $150-$300 a year. Most insurance doesn’t cover them. If you can’t afford them, stick to the free, proven method: daily inspection with your eyes and a mirror.
What’s Working: Integrated Care Works
The best results come from teams - not solo efforts. The CDC and IWGDF now recommend integrated foot care: your primary doctor, a podiatrist, a diabetes educator, and a shoe specialist all working together. Programs like this cut ulcers by 36% and amputations by 42% in Medicare patients.
If your doctor doesn’t offer this, ask. Request a referral to a podiatrist. Ask if your clinic has a foot care program. You deserve coordinated care - especially if you’re at higher risk.
The Bottom Line
Diabetic foot ulcers don’t happen overnight. They grow from neglect - not bad luck. Every day you skip your inspection, you’re gambling with your mobility, your independence, and your life.
But here’s the truth: if you do the 7-step check every day, wear the right shoes, and act fast on any sign of trouble, your risk of amputation drops to near zero. It’s not about perfection. It’s about consistency. One day off can cost you everything. Make it non-negotiable.



rachel bellet
January 17, 2026 AT 21:20The fact that 82,000 amputations happen annually in the U.S. alone is a systemic failure of patient education and healthcare accessibility. Peripheral neuropathy isn't just a complication-it's a biomarker of institutional neglect. The IWGDF risk stratification is clinically sound, but if patients can't afford podiatry visits or proper footwear, we're just performing triage on a dying system. The CDC's 68% inconsistency rate isn't about laziness-it's about socioeconomic entropy.
Moisturizing between toes? That’s not advice-it’s negligence. Fungal colonization thrives in occlusive environments, and the literature is unequivocal: interdigital moisture = biofilm incubator. The 7-step protocol is textbook, but without addressing access barriers, it’s performative medicine.
And let’s not romanticize 'daily inspection.' For a diabetic with visual impairment, carpal tunnel, or chronic fatigue, this is a Herculean task. The assumption that mirror use solves everything ignores neurodiversity and disability justice. We need policy-level interventions, not guilt-tripping.
Pat Dean
January 19, 2026 AT 03:20People in this country think they can eat their way out of everything. Diabetes isn't a 'lifestyle choice'-it's a consequence of a broken food system. But you still have to take responsibility. If you're too lazy to check your feet, don't blame the system when you lose a leg. This isn't a privilege, it's a basic survival skill. You want to keep your foot? Then do the damn checklist. No excuses.
Jay Clarke
January 20, 2026 AT 13:18Let’s be real-this whole foot thing is like a metaphor for modern life. We numb ourselves to pain, ignore the cracks in our foundation, and then wonder why everything collapses. You don’t need a checklist to save your foot-you need to stop living like a ghost in your own body. The shoes? They’re not just footwear-they’re the armor you forgot to put on. And that mirror? It’s not for your toes. It’s for your soul.
Why do we treat diabetes like it’s a moral failing? Because we’re terrified of our own mortality. But here’s the truth: you’re not broken because you have neuropathy. You’re broken because you were never taught how to be gentle with yourself.
Selina Warren
January 20, 2026 AT 16:10THIS IS YOUR LIFE. Not your foot. Not your socks. Not your doctor’s appointment. YOUR LIFE. Every single day you skip this check, you’re telling your future self: 'I don’t care if you walk again.' Stop waiting for motivation. Stop waiting for perfect conditions. Do it. Right now. Before you scroll away. Do it. Do it. DO IT. Your future self is begging you. Don’t make them beg twice.
Robert Davis
January 22, 2026 AT 14:49Interesting how the article ignores the role of insulin resistance in microvascular damage. The real issue isn’t just inspection-it’s glycemic variability. HbA1c above 7.5% accelerates axonal degeneration exponentially. Also, the 'lukewarm water' recommendation is dangerously vague. 90-95°F is meaningless without context-ambient temperature, duration of exposure, and skin perfusion matter. And no mention of autonomic neuropathy affecting thermoregulation? That’s a glaring omission.
Plus, the 'don’t soak feet' advice contradicts some European guidelines. In Germany, controlled hydrotherapy is used for wound debridement. One-size-fits-all protocols are outdated. We need personalized, biomarker-driven care.
Nishant Sonuley
January 23, 2026 AT 10:45Man, I read this and thought about my uncle back in Mumbai-he had diabetes for 20 years, walked barefoot in the house, never checked his feet, and lived to 82. So maybe this checklist isn't for everyone? I mean, culture matters. In some places, feet are just… feet. You wash them, you wear sandals, you live. The fear-mongering here is intense. Is this really about health, or is it about American medical capitalism selling us fear as a product? Also, $300 smart socks? Bro, my cousin in Delhi uses a $2 mirror and checks his feet with his phone flashlight. He’s fine. Maybe the real problem isn’t the patient-it’s the profit motive behind every 'protocol'.
Chuck Dickson
January 24, 2026 AT 01:06Hey everyone-just wanted to say this post saved my life. I was in Risk 3 after my toe amputation last year. I skipped inspections for months because I was depressed. Then I saw this checklist. I started doing it every morning after coffee. I use a $5 mirror from Walmart. I wear the same $40 sneakers I bought at Costco. No fancy gear. Just consistency. I haven’t had a single blister since. You don’t need perfection. You just need to show up. One day at a time. You got this. 💪❤️
Robert Cassidy
January 24, 2026 AT 03:15Let’s be honest-this entire movement is a distraction. The real enemy is Big Pharma and the medical-industrial complex that profits from amputations. Why do you think they push 'daily inspections'? Because if you don’t inspect, you get an ulcer. If you get an ulcer, you get a hospital stay. If you get a hospital stay, they bill Medicare $50K. It’s not about care-it’s about cash flow. The checklist is a placebo for guilt. The real solution? Universal healthcare. And maybe, just maybe, stop poisoning our food supply with high-fructose corn syrup.
Dayanara Villafuerte
January 24, 2026 AT 07:40Okay but can we talk about how the 'no flip-flops' rule is literally the only thing I follow? 😅 I wear Crocs like a queen and they’re the only thing that doesn’t crush my toes. Also, I use a phone flashlight and a selfie stick to check my soles. 📸✨ I’m not a podiatrist, but I’m a damn good selfie artist. And my feet? Still attached. 🙌
Andrew Qu
January 24, 2026 AT 23:29For anyone feeling overwhelmed-start small. Pick one step from the checklist and do it for a week. Maybe just wash and dry. Then add moisturizing. Then the mirror. You don’t have to do it all at once. Progress isn’t linear. I’ve coached dozens of patients through this. The hardest part isn’t the foot-it’s the guilt. Let go of the guilt. Just show up. That’s enough. You’re not failing. You’re learning.