
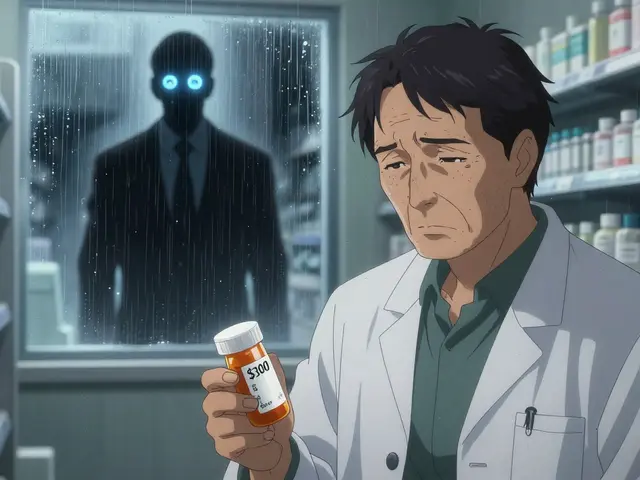
Every year, millions of people take generic medicines because they’re affordable, effective, and widely available. But what if the bottle in your hand isn’t what it claims to be? Counterfeit generic drugs are a growing threat - not just in far-off countries, but right in your local pharmacy. The World Health Organization estimates that up to 10% of medicines worldwide are fake, and in some regions, that number climbs to 30%. These aren’t just poor-quality copies. Some contain no active ingredient. Others have too much - or the wrong - drug inside. The result? Treatment failure, dangerous side effects, and even death.
Why Generic Medicines Are Targeted
Generic drugs make up 90% of prescriptions in the U.S., but they account for only 22% of total drug spending. That’s because they’re cheap. And that’s exactly why counterfeiters love them. Branded drugs like Lipitor or Nexium have strong packaging, clear serial numbers, and advanced security features. Generic manufacturers, especially smaller ones, often cut corners to stay competitive. They skip expensive security inks, skip serialization, or use generic labels that look close enough to fool the eye.Pharmacists report that verifying generics is 3 times harder than verifying branded drugs. Why? Because there’s no consistent standard. One generic metformin might have a hologram. Another might have a UV mark. A third might have nothing at all. Without a reference sample or a reliable database, how are you supposed to know?
The Three Layers of Verification
Real verification isn’t about one trick. It’s about layers. Think of it like a lock with three tumblers - you need all three to open it.Layer 1: Overt Features - What You Can See
These are the obvious signs: color-shifting ink, holograms, raised text, special fonts. Pfizer’s Viagra uses Optically Variable Ink that shifts from green to blue when tilted. Johnson & Johnson’s Tylenol uses microtext only visible under magnification. These features are meant for patients and pharmacists to spot at a glance. But here’s the catch: modern counterfeiters can replicate these with 80-90% accuracy. INTERPOL’s 2021 Operation Pangea found that fake packaging now often looks flawless to the naked eye. A pharmacist on Reddit spotted a fake Nexium generic because the expiration date font was slightly thinner. That’s the kind of detail you need to train your eye for.
Layer 2: Covert Features - What You Need a Tool For
These are hidden clues. UV inks glow under a $15 blacklight. RFID tags beep when scanned with a handheld reader. Chemical taggants like Lumilink® are invisible unless you use a $300 handheld detector. These are harder to copy because counterfeiters don’t know what to look for. But they’re useless if you don’t have the tools. Most community pharmacies don’t carry UV lights or scanners. Hospitals and large chains do - but even then, staff need training. A 2023 Drug Topics survey found pharmacists using handheld spectrometers reported 94% satisfaction - but only 12% of independent pharmacies have access to them.
Layer 3: Track-and-Trace - The Digital Trail
This is the backbone of modern drug safety. Every package gets a unique serial number following the GS1 standard. In the U.S., the Drug Supply Chain Security Act (DSCSA) requires this for all prescription drugs by November 2023. In the EU, the Falsified Medicines Directive (FMD) has required it since 2019. The system works like this: when you scan the barcode, it checks against a central database. If the serial number is valid and hasn’t been used before, the drug is real. The European system handles over 2.5 billion verifications a year with 99.998% uptime. Sounds perfect, right? Not so fast. A 2023 study found that barcode scanning fails 40-50% of the time with generics. Why? Because many generic manufacturers don’t serialize properly. Or they use inconsistent formats. Or their database isn’t linked. In Nigeria, mobile verification apps work only 65% of the time due to poor internet. So even the best digital system fails without reliable data.
How Professionals Detect Fakes in the Lab
When visual checks and barcodes aren’t enough, labs turn to science. Two tools dominate: NIR and Raman spectroscopy.NIR Spectroscopy
Handheld devices like the Thermo Fisher TruScan® RM use near-infrared light to measure how a tablet absorbs energy. Every drug has a unique chemical fingerprint. If the active ingredient is wrong, or the coating is off, the machine knows. It’s fast - 10 to 30 seconds per test - and accurate 92-97% of the time. A 2020 study used NIR to catch fake Plavix generics by spotting moisture differences invisible to the eye. It’s the gold standard for field use because it doesn’t destroy the sample and works through packaging.
Raman Spectroscopy
This tool, like the B&W Tek NanoRam®, uses laser light to detect molecular vibrations. It’s great for identifying specific chemicals. But it struggles with dark-colored pills because the dye interferes with the signal. It’s also more expensive and heavier than NIR. Still, when it works, it’s powerful. One pharmacist in Ohio used a NanoRam® to catch fake metformin that looked identical to the real thing. The fake had the wrong salt form - a detail that could’ve killed a diabetic patient.
These machines cost $15,000 to $50,000. Hospitals can afford them. Small pharmacies? Not so much. That’s why the FDA recommends starting simple: a UV light, a magnifying glass, and a reference sample from the manufacturer.

What Works Best - The Data Says
No single method catches everything. But combining them? That’s where the real protection lies.A 2023 study in the Journal of Pharmaceutical Analysis found that using both overt features and spectroscopy together caught 98.7% of counterfeits. Single-method approaches only caught 82.4%. That’s a huge gap.
Here’s what experts agree on:
- Dr. Paul Newton (Oxford): “Track-and-trace reduces wholesale counterfeiting - but 80% of clinics in Africa can’t use it.”
- Dr. Maria Kresal (EDQM): “Packaging can be copied with 95% accuracy. You must test the medicine inside.”
- U.S. FDA: “No single method gives 100% protection. Use a layered approach.”
Bottom line: If you’re a pharmacist, don’t rely on the hologram. Don’t trust the barcode alone. Use visual checks, then confirm with a spectrometer if you can. If you’re a patient, know the signs.
What Patients Can Do
You don’t need a lab to protect yourself. Here’s what you can do:- Check the packaging. Is the font different? Is the color slightly off? Is the expiration date smudged?
- Compare your current bottle to the last one. Even small changes in label layout matter.
- Ask your pharmacist: “Is this the same generic as before?” If they hesitate, ask why.
- Don’t buy from online pharmacies that don’t require a prescription. The FDA warns 96% of these sites are illegal.
- Report anything suspicious. Use the FDA’s MedWatch program or your local health department.
One woman in Texas noticed her generic blood pressure pill tasted bitter. The real one didn’t. She called her pharmacist. It turned out to be a fake batch with no active ingredient. She saved herself from a stroke.

The Future: AI, Blockchain, and Global Standards
The fight against fake drugs is evolving. The FDA is testing blockchain systems to track generics through every step of the supply chain. Early results show 99.2% accuracy. The EU will require cryptographic 2D barcodes on all generics by January 2025. By 2026, the U.S. aims to serialize 100% of generics.But technology alone won’t fix this. The real problem is inequality. Rich countries have labs and scanners. Poor countries have nothing. As long as counterfeiters can profit in places with weak oversight, the problem won’t disappear. The WHO says global cooperation is essential - no single country can solve this alone.
For now, the best defense is awareness. Know your medicine. Question inconsistencies. Demand transparency. Because when it comes to your health, you can’t afford to guess.
How can I tell if my generic medicine is fake?
Start with a visual check: look for differences in font, color, packaging texture, or expiration date formatting. Compare it to your last bottle. Use a UV light to check for hidden marks. If the pill looks, smells, or tastes different, or if the bottle feels cheap, be suspicious. Always ask your pharmacist to verify the source. If you’re unsure, report it to the FDA’s MedWatch program.
Are all generic drugs safe?
Yes - if they’re authentic. Generic drugs approved by the FDA or equivalent agencies are required to be bioequivalent to the brand-name version. But counterfeit generics - the ones made illegally - are not. These fake products can contain no active ingredient, the wrong ingredient, or toxic fillers. The problem isn’t the generic label - it’s the lack of oversight in the supply chain. Stick to licensed pharmacies and avoid unregulated online sellers.
Why don’t all generic manufacturers use security features?
Cost. Generic drugs are sold at low margins, and adding holograms, UV inks, or serialization adds 1.2-1.8% to production costs. Many manufacturers, especially smaller ones, skip these features to stay competitive. Branded drugs invest more because they have higher profits and stronger brand protection. Regulatory pressure is increasing - the U.S. aims for 100% serialization by 2026 - but until then, inconsistency remains a major problem.
Can I trust barcode scanners on my phone for generic drugs?
Not always. While barcode scanners work well for branded drugs with consistent serialization, they fail 40-50% of the time with generics. Many generic manufacturers don’t follow GS1 standards properly, or their databases aren’t updated. Network issues in rural areas also cause failures. Use scanners as a first check - never as the only one. Always combine with visual inspection and, if possible, professional verification tools.
What should I do if I suspect a fake medicine?
Don’t take it. Return it to the pharmacy immediately. Ask them to contact the manufacturer or distributor. Report the incident to the FDA’s MedWatch program at fda.gov/medwatch or by calling 1-800-FDA-1088. Provide the product name, lot number, expiration date, and where you bought it. Your report could help stop a dangerous batch from reaching others.
What’s Next for You
If you’re a patient: Keep your eyes open. Compare bottles. Ask questions. Don’t be afraid to push back if something feels off.If you’re a pharmacist: Start with the basics - UV light, magnifier, reference samples. Advocate for access to handheld spectrometers. Push for better training and standardized labeling across generics.
If you’re a policymaker or manufacturer: Invest in serialization. Support small producers. Push for global standards. The cost of inaction is measured in lives.
Generic medicines saved billions in healthcare costs. But they can’t do that if they’re fake. Verification isn’t optional - it’s essential.


Andrew Forthmuller
November 11, 2025 AT 18:44My pharmacy gave me a generic pill that tasted like ash. I didn’t say anything till my hand started tingling. Turned out it was fake. Don’t ignore weird tastes.
Renee Ruth
November 13, 2025 AT 11:53They say ‘holograms are easy to fake’ but no one talks about how the damn bottle caps are different. My last bottle had a slightly different ridge pattern. I noticed because I’m obsessive. I called the manufacturer. They confirmed it was counterfeit. They didn’t even know it was in circulation. This isn’t just about pills - it’s about trust.
I keep a photo of my last prescription bottle on my phone. Every time I get a refill, I compare. Font size. Spacing. Even the shade of white on the label. It’s insane that I have to do this. But I will - because I almost died once from a fake antibiotic.
Pharmacists aren’t trained for this. They’re rushed. They assume the distributor got it right. But the distributor doesn’t check either. It’s a chain of negligence. And we’re the ones swallowing the consequences.
I once reported a fake to MedWatch. Got an automated reply. No follow-up. No call. Nothing. So now I post photos online. I tag the brand. I tag the pharmacy. I tag the FDA. If silence is complicity, then I’m loud.
And yes - I’ve been called paranoid. I’ve been told I’m overreacting. But when your life depends on a pill, you don’t get to be ‘kinda sure.’ You get to be 100% certain. Or you get to stop taking it.
Nicole M
November 15, 2025 AT 07:21I use a UV keychain light now. It’s $8 on Amazon. I shine it on every new bottle. If nothing glows, I ask. No shame. Better safe than sorry.
Elizabeth Buján
November 17, 2025 AT 00:05Y’know… I used to think fake meds were a third-world problem. Then my grandma got a batch of fake metformin that had lead in it. She didn’t know. She just thought she was ‘feeling off.’ We almost lost her. And the pharmacy? They said ‘it’s probably just stress.’
It’s not just about money. It’s about how we treat each other’s lives. If you can’t trust your medicine, what can you trust? Your doctor? Your pharmacy? The system?
I started keeping a little notebook - brand, lot number, date, how the pill looked. I don’t care if it’s weird. I care that I’m alive. And if I’m weird for doing that, then fine. I’ll be the weird one who lived.
My mom says I’m too careful. But I’d rather be careful and alive than ‘normal’ and dead.
People say ‘just buy from big pharmacies.’ But even CVS has had recalls. Even Walgreens. The system’s broken. And we’re all just trying to survive it.
Arpita Shukla
November 18, 2025 AT 00:21Actually, most of the counterfeit drugs in India come from unlicensed online sellers - not local pharmacies. You’re overestimating the risk in regulated markets. The real issue is the black market in Southeast Asia and Africa. In the US, the FDA’s supply chain controls are actually quite robust. The 10% global counterfeit stat is misleading because it’s skewed by low-income countries with zero oversight. You’re not getting fake pills from your CVS unless you’re buying them from a sketchy kiosk in a gas station parking lot.
Also, NIR spectroscopy? That’s not something you bring to a small pharmacy. It’s a lab tool. The FDA’s recommendation of UV + magnifier is correct. You don’t need a $50k machine to spot a fake if you know what to look for. The real problem is people don’t educate themselves. They assume the pill is safe because it’s labeled ‘generic.’ That’s the flaw - not the system.
And yes, serialization fails sometimes. But that’s because manufacturers cut corners. The system works - if everyone follows the rules. The problem isn’t the tech. It’s the people who refuse to pay for it.
Samantha Wade
November 18, 2025 AT 19:24As a pharmacist with over 20 years of experience, I can confirm: the layered verification approach outlined in this post is not just theoretical - it’s the standard of care in accredited institutions. We use UV lights daily. We compare reference samples from the manufacturer’s batch. We log every discrepancy. And yes - we have trained staff to operate handheld spectrometers in our central pharmacy.
However, the reality for independent pharmacies is dire. Most operate on thin margins and cannot afford $20,000 devices. The FDA’s guidance is sound, but without funding, training, or regulatory enforcement, it remains aspirational. We need federal subsidies for small pharmacies to acquire verification tools - not just recommendations.
Additionally, the inconsistency in generic labeling is a systemic failure. There should be a mandatory visual standard for all generics - font, color, layout - enforced by the FDA. No more ‘looks close enough.’ If it doesn’t match the approved specification, it’s not allowed on the shelf.
Patients: You are not being paranoid. You are being vigilant. And you should never be made to feel foolish for asking, ‘Is this the same as last time?’ That question saves lives.
Manufacturers: Stop cutting corners. Your profit margin is not worth a patient’s life. And regulators: Stop relying on voluntary compliance. Enforce. Audit. Punish. The cost of inaction is measured in ICU beds - not balance sheets.
manish kumar
November 19, 2025 AT 18:45Let me tell you something from India - we have a huge problem with fake medicines, but it’s not because of the pharmacies. It’s because of the distributors. Most of the counterfeit drugs enter through third-party wholesalers who mix fake batches with real ones. The pharmacies don’t even know. They’re just taking delivery from their usual supplier. And the government? They’re too busy with bureaucracy to crack down. We have over 10,000 unregistered drug manufacturers operating in rural areas. No inspections. No traceability. No accountability.
But here’s what’s worse: patients in villages don’t know how to check. They buy from whoever sells it cheapest. They don’t have UV lights. They don’t have smartphones. They don’t even have electricity to charge them. So when a fake pill kills someone, it’s just another statistic. No headlines. No outrage.
The blockchain solution? Sounds great on paper. But in a village where internet speed is 2G and the nearest pharmacy is 20km away, how’s that going to help? We need low-tech solutions - like color-coded caps, tactile markings, or even QR codes that work offline. Something that doesn’t require a network or a $300 device.
And let’s stop pretending this is just a US problem. This is a global crisis. The WHO says 1 in 10 medicines is fake. That’s 100 million people a year. We need a global registry - not just for serialization, but for accountability. Every manufacturer, every batch, every shipment - traceable. No exceptions. No loopholes.
And yes, I know it’s expensive. But how expensive is a child’s death? How expensive is a mother losing her husband because his blood pressure pill had no active ingredient? Money is not the barrier. Willpower is.
Mark Rutkowski
November 21, 2025 AT 07:14There’s a quiet horror in this story - not because pills are fake, but because we’ve normalized the idea that our medicine should be a gamble. We accept that our health is subject to supply chain opacity, corporate cost-cutting, and regulatory lag. We don’t protest. We don’t demand change. We just take the pill, hope it works, and move on.
But here’s the truth: your body is not a testing ground. Your life is not a cost-benefit analysis. And your trust should not be a commodity sold to the lowest bidder.
Every time you buy a generic, you’re not just buying a drug - you’re buying into a system. And that system is built on silence. On assumption. On the quiet resignation of millions who don’t know any better.
So when you notice the font is off - don’t shrug. When the pill tastes strange - don’t ignore it. When your pharmacist hesitates - don’t let it go. Because in a world where profit outweighs principle, the only thing standing between you and death is your willingness to ask: ‘Is this real?’
And if the answer is ‘I don’t know’ - then you’ve already lost.
Benjamin Stöffler
November 22, 2025 AT 07:31Let’s be brutally honest: the entire pharmaceutical supply chain is a house of cards built on trust, opacity, and regulatory capture. The FDA? They’re underfunded. The manufacturers? They’re incentivized to cut corners. The consumers? They’re conditioned to believe that ‘generic’ means ‘safe.’ And yet - we’re surprised when the system fails? Of course it fails. It was designed to fail - just slowly enough that no one notices until someone dies.
Blockchain? AI? Spectrometers? These are not solutions - they’re distractions. They make us feel like we’re doing something, while the root cause - profit-driven negligence - remains untouched. You don’t fix a broken system by adding more layers of technology. You fix it by dismantling the incentives that created the problem in the first place.
Why do generics lack security features? Because the market rewards the cheapest bidder. Why do pharmacists lack tools? Because insurance companies won’t reimburse for verification. Why do patients accept this? Because they’re told, ‘It’s just a pill.’
Until we stop treating medicine like a commodity - and start treating it like a human right - all the UV lights and barcodes in the world won’t matter. We’re not fighting counterfeit drugs. We’re fighting a culture that values profit over life.
And until that changes - we’re all just waiting for the next pill to kill us.
vanessa k
November 23, 2025 AT 18:37I used to think this was all hype - until my brother had a seizure because his fake epilepsy pill had no active ingredient. He was 22. He didn’t even know he was taking a fake. The pharmacy swore it was the same as before. But the color was lighter. The number on the pill was different. He trusted them. We all did.
Now I check every bottle. I take a picture. I compare. I ask. I don’t care if I sound crazy. I care that he’s still here.
And if you think this doesn’t happen in the US - you’re wrong. It happens every day. And no one’s talking about it. Until it’s your kid. Your mom. Your best friend.
Don’t wait for a crisis to care. Start now. Ask. Check. Report. You have no idea how much power you have.