Uremic Symptoms: What They Are, Why They Matter, and How to Recognize Them
When your kidneys stop working properly, waste builds up in your blood—that’s uremia, a toxic condition caused by kidney failure where waste products like urea and creatinine accumulate in the bloodstream. Also known as uremic syndrome, it’s not a disease itself but a red flag that your body can’t filter toxins anymore. If you have chronic kidney disease, a gradual loss of kidney function over time, often from diabetes or high blood pressure and you start feeling off, it’s not just aging—it could be uremic symptoms creeping in.
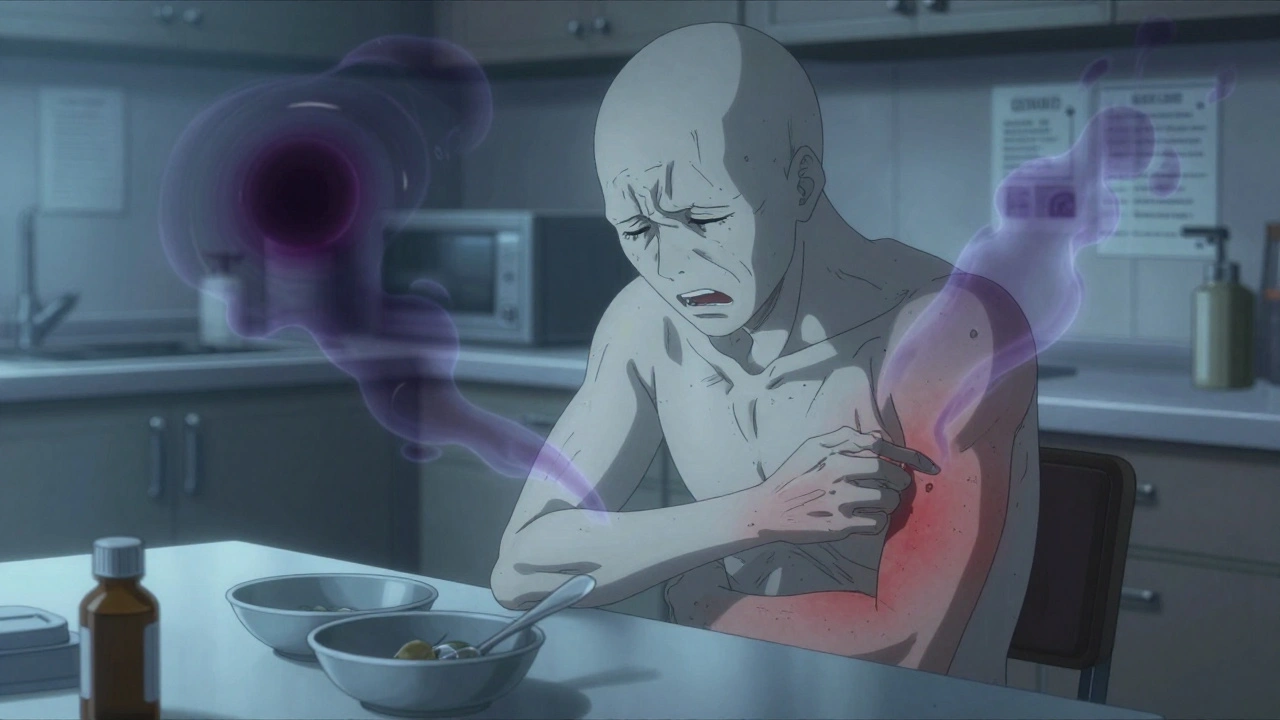
These symptoms don’t show up all at once. They sneak in slowly: constant tiredness, loss of appetite, nausea that won’t go away, or a metallic taste in your mouth. You might notice swelling in your legs, itchy skin, or trouble concentrating. Some people get confused or even have seizures in advanced stages. These aren’t random side effects—they’re your body screaming that it’s drowning in its own waste. And if you’re on dialysis, a treatment that artificially removes waste and excess fluid from the blood when kidneys fail, missing sessions or not sticking to your diet can make these symptoms worse fast.
Uremic symptoms often get mistaken for the flu, stress, or depression. But if you have kidney disease and you’re feeling worse than usual—especially with vomiting, confusion, or shortness of breath—you need to act. It’s not about waiting to see if it passes. Every hour counts. The good news? Catching these signs early means you can adjust your treatment, avoid hospitalization, and protect your brain and heart from further damage. Below, you’ll find real-world advice from people who’ve lived through this, tools to track symptoms, and clear info on how medications, diet, and dialysis interact with uremia. No fluff. Just what you need to know to stay ahead of it.