Uremic Pruritus: Causes, Treatments, and What Really Works
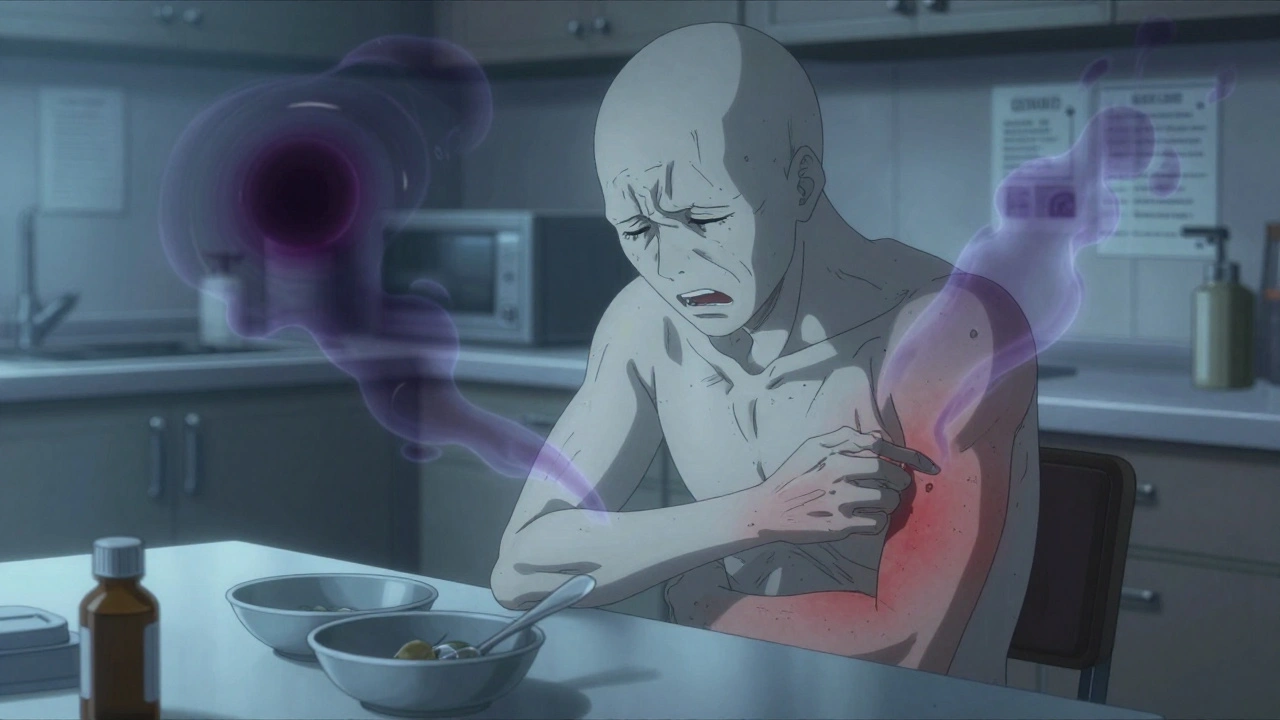
When your kidneys fail, toxins build up in your blood—and one of the most frustrating results is uremic pruritus, a severe, chronic itching caused by kidney disease that doesn’t respond to typical anti-itch creams. Also known as dialysis itch, it affects up to 40% of people on long-term dialysis and can make sleep, work, and daily life nearly impossible. This isn’t dry skin. It’s not allergies. It’s a neurological and systemic problem tied directly to how your body handles waste when kidneys can’t filter it anymore.
Chronic kidney disease, the underlying condition driving uremic pruritus changes more than just your blood chemistry. It disrupts immune signaling, alters nerve sensitivity, and triggers inflammation in the skin. Even when dialysis removes urea and creatinine, other toxins like parathyroid hormone, histamine, and opioids linger—each one feeding the itch cycle. That’s why antihistamines and moisturizers often do nothing. You’re treating a symptom, not the root cause.
What actually helps? Some patients find relief with pruritus treatment, targeted therapies like gabapentin, nalfurafine, or phototherapy—options that act on nerve pathways, not skin. Others benefit from adjusting dialysis type or frequency, or even switching from certain phosphate binders. But most doctors still treat it like a skin issue, leaving patients frustrated. The truth? Uremic pruritus needs a medical strategy, not a lotion.
Below, you’ll find real, evidence-based posts on how this condition connects to medication safety, drug interactions, and long-term kidney care. You’ll see why some drugs make it worse, how to track symptoms like you would blood pressure, and what alternatives exist when standard treatments fail. No fluff. Just what works for people living with this relentless itch every day.