Steroid-Induced Diabetes: Causes, Risks, and What You Can Do
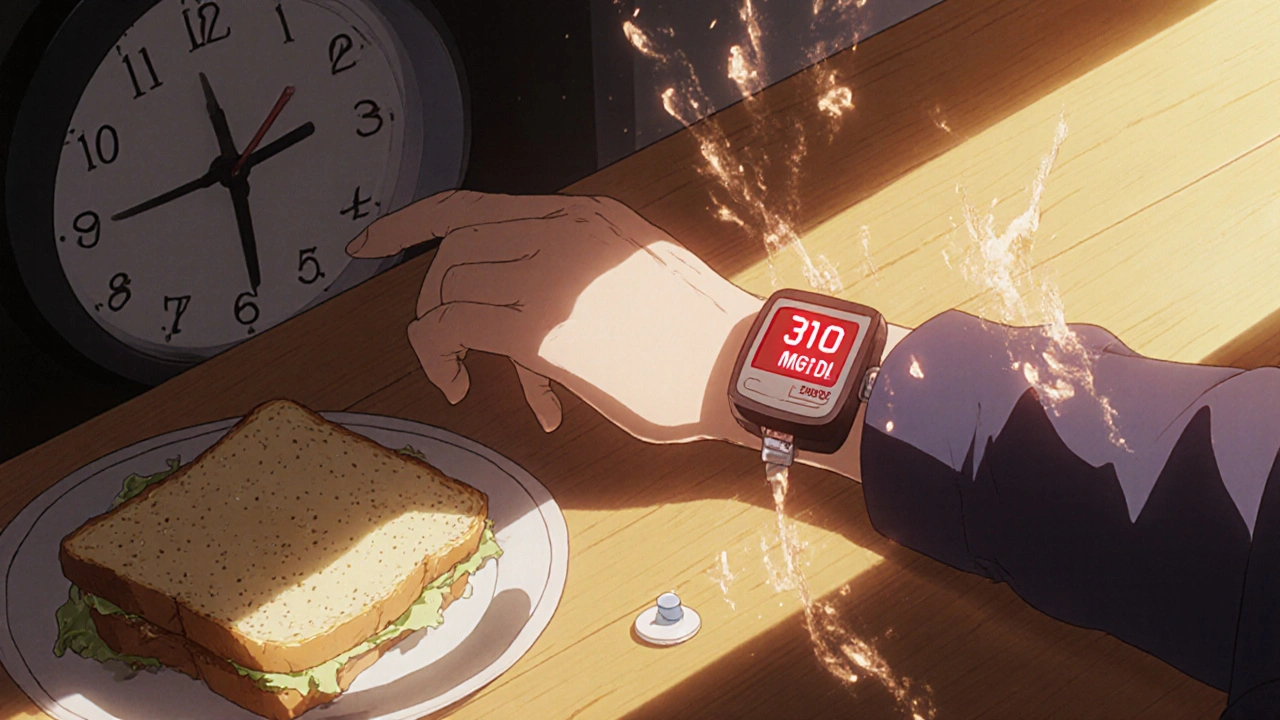
When you take steroid-induced diabetes, a type of high blood sugar triggered by corticosteroid medications. It's not the same as type 1 or type 2 diabetes—it’s a side effect, not a lifelong condition. Also known as glucocorticoid-induced hyperglycemia, it shows up when your body can’t handle the flood of sugar from steroids, even if you’ve never had diabetes before. This isn’t rare. People on long-term prednisone, dexamethasone, or other corticosteroids for asthma, arthritis, or autoimmune diseases often see their blood sugar climb. It’s not your fault. It’s chemistry.
What’s happening? corticosteroids, powerful anti-inflammatory drugs that alter how your body uses sugar. Also known as glucocorticoids, they tell your liver to dump more glucose into your bloodstream while making your muscles and fat cells less responsive to insulin. That’s insulin resistance, when your cells stop listening to insulin’s signal to absorb sugar. Your pancreas tries to keep up by pumping out more insulin—but eventually, it can’t. Blood sugar rises. You might feel thirsty, tired, or need to pee more. These aren’t just side effects—they’re warning signs.
Not everyone gets it. Risk goes up if you’re overweight, have a family history of diabetes, are over 45, or take high doses for more than a few weeks. Even short courses can spike numbers in sensitive people. The good news? Once you stop the steroids, blood sugar often returns to normal. But while you’re on them, you need to pay attention. Monitoring your sugar at home, cutting back on sugary foods, and staying active can help. Some people need temporary insulin or metformin. Your doctor can help you decide.
You’ll find posts here that break down how steroids mess with your metabolism, what to watch for, and how to protect your health without stopping necessary treatment. You’ll also see how other medications—like statins or proton pump inhibitors—can interact with your sugar levels, and how to spot hidden risks when you’re on multiple drugs. This isn’t about fear. It’s about control.