Steroid Hyperglycemia: How Steroids Raise Blood Sugar and What to Do
When you take steroid hyperglycemia, a rise in blood sugar caused by steroid medications. Also known as corticosteroid-induced hyperglycemia, it happens because these drugs interfere with how your body uses insulin—making even healthy people suddenly struggle with high glucose levels. This isn’t just a side effect you can ignore. It’s a real metabolic shift that can last as long as you’re on the meds—and sometimes longer.
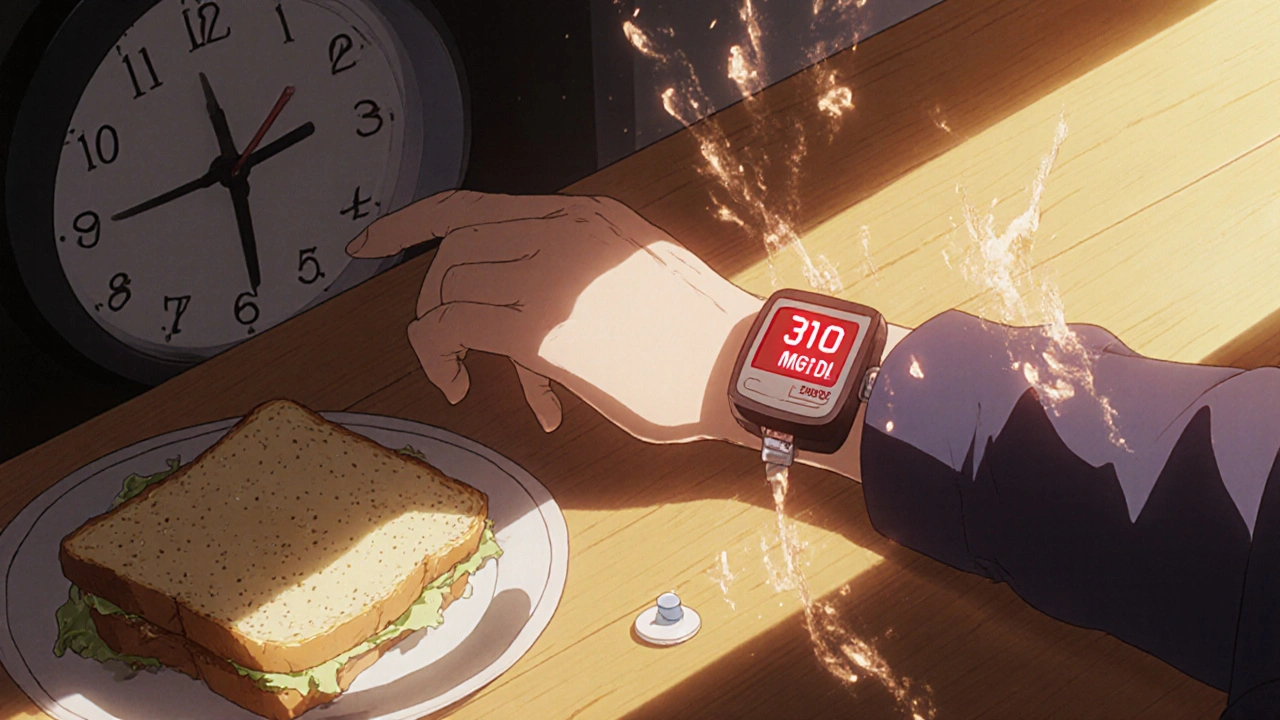
It’s not just people with diabetes who get hit. Even if you’ve never had high blood sugar before, a short course of prednisone or dexamethasone can push your numbers into dangerous territory. Why? Steroids tell your liver to dump more glucose into your bloodstream while making your muscles and fat cells less responsive to insulin. The result? Your body can’t clean up the sugar fast enough. Studies show up to 30% of non-diabetic patients on oral steroids develop glucose levels above 200 mg/dL. That’s not a fluke—it’s biology.
This isn’t just about numbers on a screen. High blood sugar from steroids can cause fatigue, blurry vision, frequent urination, and dry mouth. In older adults or those with existing heart or kidney issues, it can lead to hospitalization. And if you’re on long-term steroids for conditions like lupus, asthma, or rheumatoid arthritis, you’re not just managing inflammation—you’re managing a hidden metabolic burden.
What helps? Monitoring your glucose daily is the first step. Some people need temporary insulin. Others just need to cut back on carbs and stay hydrated. It’s not about avoiding steroids—they’re often life-saving—but about knowing how to work with them, not against your body. You don’t need to guess. You need a plan.
Below, you’ll find real, practical advice from people who’ve dealt with this exact problem. From how to spot early signs to what medications to avoid mixing with steroids, these posts give you the tools to take control—not just survive the side effects, but manage them with confidence.