Respiratory Depression: Causes, Risks, and What to Do When It Happens
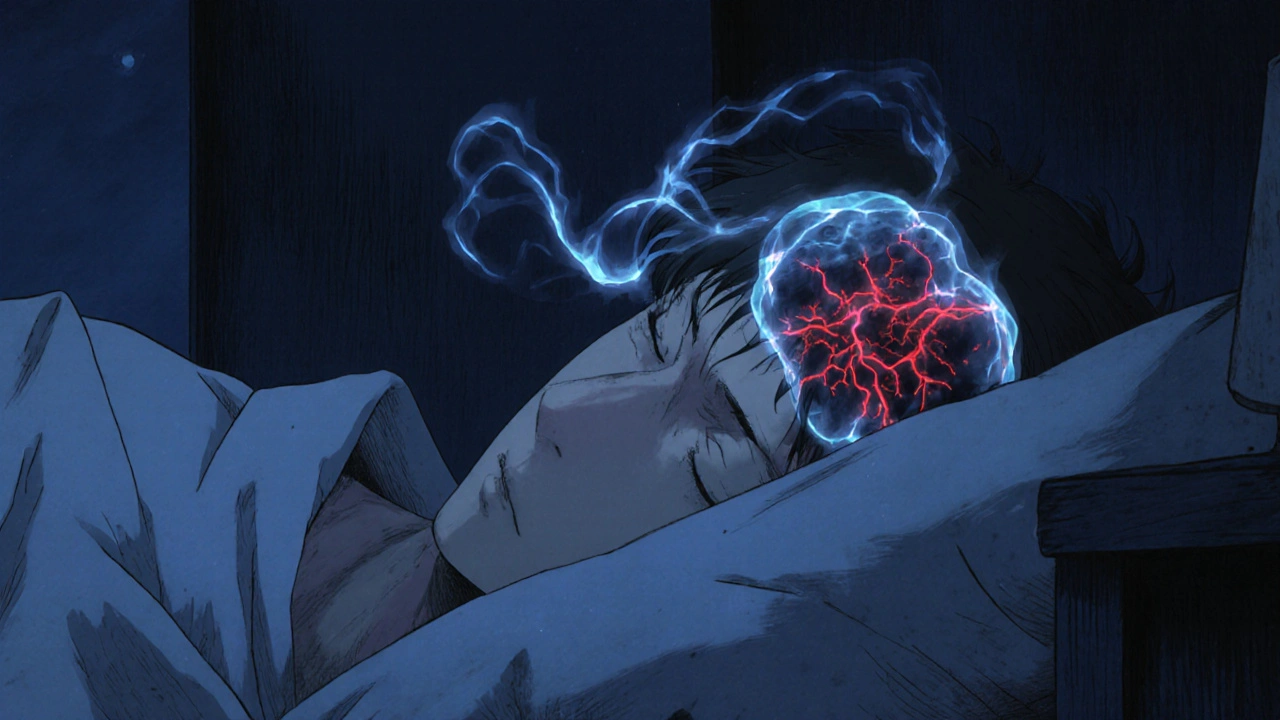
When your breathing slows down too much, it’s called respiratory depression, a dangerous drop in breathing rate or depth that reduces oxygen intake and increases carbon dioxide in the blood. Also known as hypoventilation, it’s not just a side effect—it’s a medical emergency that can lead to coma or death if not acted on quickly. This isn’t rare. It happens often with opioids like oxycodone, morphine, or fentanyl, especially when mixed with alcohol, benzodiazepines, or sleep aids. Even people taking prescribed doses can slip into respiratory depression without realizing it.
It’s not just about painkillers. Sedatives like barbiturates, certain antipsychotics, and even high doses of muscle relaxants can trigger it. People with sleep apnea, COPD, or kidney/liver problems are at higher risk. Older adults and those on multiple medications are especially vulnerable. You won’t always feel it coming. Someone might seem drowsy, then their breathing becomes shallow, then slow, then stops. That’s why knowing the signs matters more than ever.
There’s a reason naloxone is now carried by first responders and even some families. It reverses opioid-induced respiratory depression fast—but only if you act. If someone’s breathing less than 8 times a minute, has blue lips, or can’t wake up, call emergency services immediately. Don’t wait. Don’t assume they’re just asleep. Time is oxygen.
The posts below cover real cases and practical advice. You’ll find guides on recognizing early warning signs of breathing trouble from common meds, how to avoid dangerous drug combos, what to do if a loved one is at risk, and how naloxone fits into home safety plans. These aren’t theoretical—they’re based on emergency reports, clinical experience, and patient stories. Whether you’re managing chronic pain, caring for someone on opioids, or just want to understand the hidden risks of everyday prescriptions, this collection gives you the facts you need to stay safe.