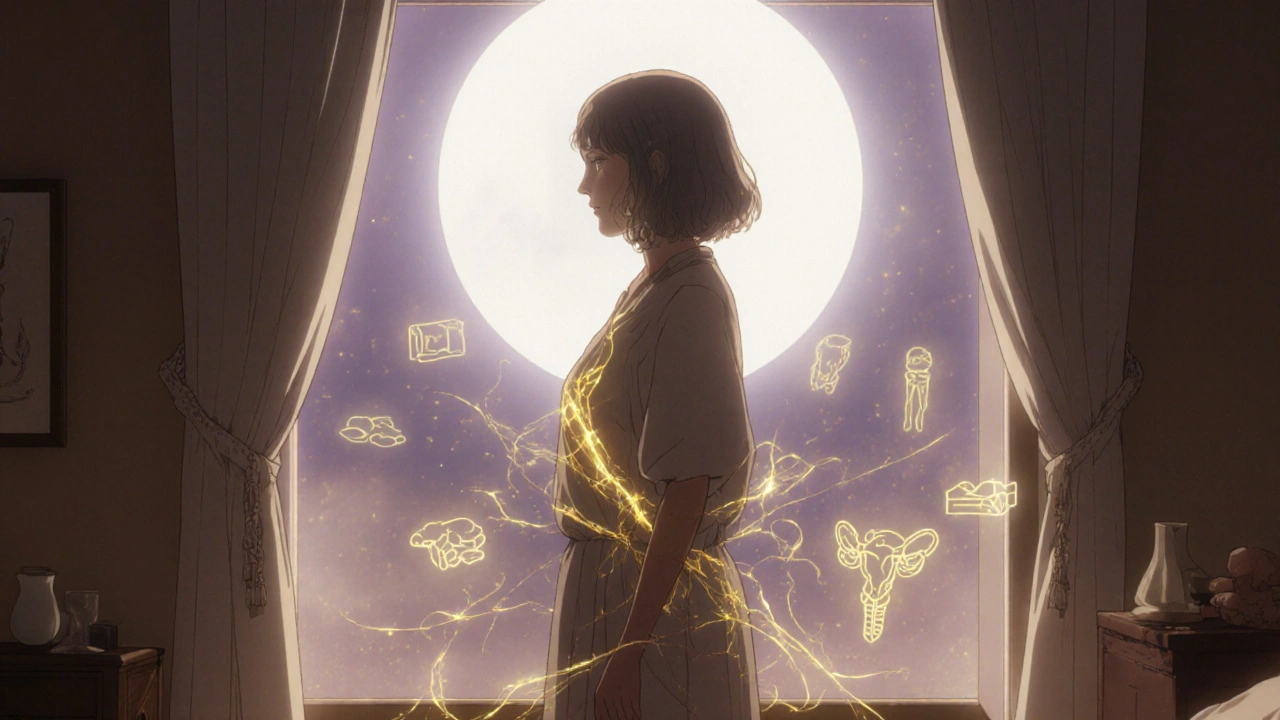
Progesterone Decline: What Happens When Levels Drop and How It Affects Your Body
When progesterone decline, a drop in the hormone that supports pregnancy, regulates the menstrual cycle, and calms the nervous system. Also known as low progesterone, it’s not just a menopause issue—it can start in your 30s, after stress, or following birth control use. This isn’t about being "hormonally imbalanced" as a buzzword. It’s about real changes in your body: trouble sleeping, mood swings, heavier periods, or unexplained weight gain around the belly.
Progesterone works with estrogen, the primary female sex hormone that drives ovulation and builds the uterine lining. When progesterone drops, estrogen dominates—leading to what’s called estrogen dominance, a condition where estrogen isn’t properly balanced by progesterone, even if estrogen levels are normal. This imbalance shows up as breast tenderness, bloating, or fibroids. It’s not rare. Studies tracking women over 40 show nearly 70% report symptoms tied to this shift, even before full menopause.
Low progesterone also affects your brain. It’s a natural calming agent—similar to how benzodiazepines work, but made by your body. When levels fall, anxiety spikes, insomnia gets worse, and you might feel like you’re on edge for no reason. It’s not "just stress." Your brain chemistry has changed. And because progesterone helps regulate blood sugar and thyroid function, its decline can make you feel tired even after sleeping enough.
You don’t need a lab test to suspect this. If you’ve noticed your period becoming unpredictable, your PMS turning into full-blown mood crashes, or you’re gaining weight despite eating the same way, progesterone decline could be the hidden cause. The good news? It’s treatable—with lifestyle changes, targeted supplements, or, in some cases, bioidentical hormone support under medical supervision.
Below, you’ll find real, evidence-based guides on how low progesterone connects to sleep problems, medication interactions, and even how other hormones like cortisol and thyroid function play into the mix. No fluff. Just what works.