As you get older, your body changes in ways you might not expect. One of the quietest but most impactful shifts happens deep inside your endocrine system - your progesterone levels start to drop. This isn’t just a footnote in menopause. It’s a major player in fatigue, mood swings, sleep troubles, and even bone thinning. And it starts earlier than most people think.
Progesterone isn’t just a ‘female hormone’ - it’s a master regulator
Many people think progesterone is only about pregnancy. But it does far more. It balances estrogen, supports thyroid function, calms the nervous system, helps you sleep, and even protects your bones and brain. In fact, progesterone turns on genes that help repair tissue and reduce inflammation. When it drops, those systems start to slow down.
Women see the biggest shift after 35, but it’s not just a women’s issue. Men produce progesterone too - in smaller amounts - and it helps with stress response, muscle maintenance, and even prostate health. As both men and women age, progesterone production declines, often before estrogen or testosterone do.
When does progesterone start to fall?
The real drop begins in your mid-30s. By 40, many women are producing less than half the progesterone they did in their 20s. This isn’t sudden. It’s a slow leak. The ovaries, which make most of your progesterone, start to age. They become less responsive to signals from the brain. Ovulation becomes irregular or stops altogether. No ovulation? No progesterone. That’s the simple math.
In men, the adrenal glands are the main source of progesterone. As stress increases and adrenal function slows with age, progesterone levels follow. By 50, men may have 30-40% less progesterone than they did in their 30s. That’s why older men often report increased anxiety, poor sleep, and reduced muscle recovery - all linked to low progesterone.
What happens when progesterone drops too low?
Low progesterone doesn’t just mean you miss your period. It creates a cascade of symptoms:
- Insomnia - Progesterone boosts GABA, the brain’s natural calming chemical. Less progesterone = more racing thoughts at night.
- Anxiety and irritability - Without progesterone to balance estrogen, your brain gets overstimulated. You might feel on edge for no reason.
- Weight gain around the midsection - Low progesterone makes your body hold onto fat, especially in the belly. It also slows metabolism.
- Bone loss - Progesterone stimulates bone-building cells. Without it, osteoporosis risk climbs, even in people who exercise and eat well.
- Brain fog and memory lapses - Progesterone protects neurons and supports hippocampal function. Low levels are tied to faster cognitive decline.
A 2023 study tracking over 2,000 women aged 35-65 found that those with the lowest progesterone levels were 2.3 times more likely to report severe sleep disruption and 1.8 times more likely to have measurable memory decline over a 3-year period - even after adjusting for estrogen levels.

Why standard hormone tests miss the problem
Most doctors test estrogen and testosterone. Progesterone? Often ignored. And when they do test it, they use the wrong timing. Progesterone spikes mid-cycle - around day 21 in a 28-day cycle. If you test on day 5 or day 25, you’re not getting the real picture.
Even worse, many labs use “normal” ranges based on young, healthy women. But what’s normal for a 25-year-old isn’t normal for a 55-year-old. Your body’s needs change. A progesterone level of 1.5 ng/mL might be “normal” on paper, but if you’re feeling exhausted, anxious, and sleeping poorly - that’s not normal for you.
What you need is a saliva or dried blood spot test done during your luteal phase (days 19-23). These tests show what’s actually happening in your tissues, not just your blood. They’re more accurate for tracking hormone activity in aging bodies.
What you can do about it
You can’t stop aging. But you can support your body’s ability to make and use progesterone.
- Manage stress - Cortisol (the stress hormone) steals the raw materials your body needs to make progesterone. Meditation, walking in nature, and deep breathing can help lower cortisol and free up resources.
- Eat more magnesium-rich foods - Spinach, pumpkin seeds, almonds, and dark chocolate help your body convert cholesterol into progesterone. Magnesium deficiency is common in older adults and directly limits hormone production.
- Get enough zinc - Found in oysters, beef, and lentils, zinc supports the adrenal glands and ovarian function. A 2022 trial showed that 30 mg of zinc daily improved progesterone levels in 68% of women over 45 with low levels.
- Avoid excess sugar and processed carbs - Blood sugar spikes trigger insulin surges, which block progesterone receptors. That means even if you have some progesterone, your body can’t use it.
- Consider bioidentical progesterone cream - If lifestyle changes aren’t enough, a low-dose, compounded bioidentical progesterone cream applied to the skin (5-20 mg daily) can help restore balance. It’s not for everyone, but for many women and men over 45, it’s life-changing. Always work with a doctor who understands hormone physiology - not just prescriptions.
What doesn’t work
Don’t waste time on over-the-counter “hormone balancers” that say they boost progesterone. Most are just herbs like chasteberry or black cohosh. They might help with PMS in younger women, but they don’t raise progesterone in aging bodies. Your ovaries or adrenals aren’t producing it - no herb can force them to.
And don’t assume estrogen replacement fixes everything. If you take estrogen without enough progesterone, you increase your risk of breast tissue overgrowth, blood clots, and mood crashes. Progesterone isn’t the sidekick - it’s the safety net.
When to get tested
If you’re over 35 and noticing any of these, it’s time to check your progesterone:
- Difficulty falling or staying asleep
- Unexplained anxiety or panic attacks
- Weight gain despite eating clean and exercising
- Hot flashes or night sweats
- Memory lapses or trouble concentrating
- Low libido that doesn’t improve with time
Don’t wait for your doctor to bring it up. Ask for a progesterone test - specifically during your luteal phase. If they say it’s not necessary, find someone who understands hormonal aging. This isn’t vanity. It’s metabolic health.
The bigger picture
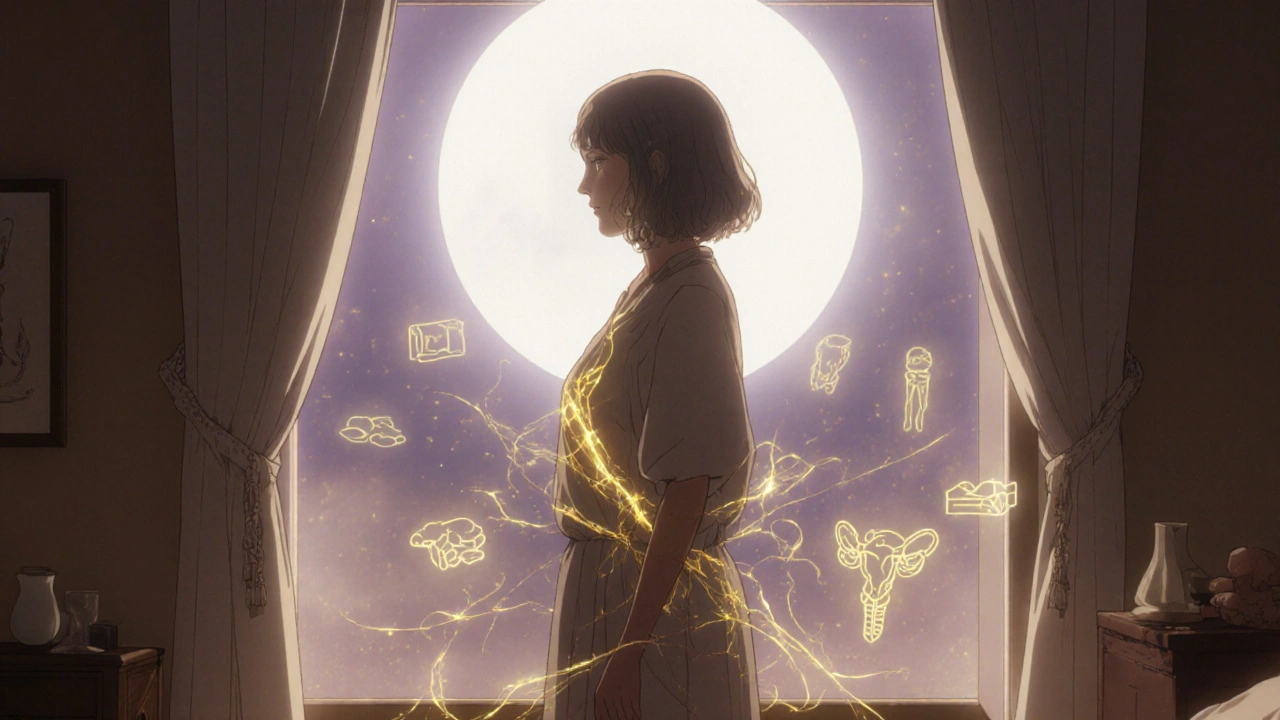
Progesterone decline isn’t just about hormones. It’s about how your body adapts to decades of stress, sleep loss, poor nutrition, and environmental toxins. The drop in progesterone is a symptom - not the root cause. But fixing it can unlock improvements in energy, mood, sleep, and even cognition.
Think of it like this: your body is a house. Estrogen is the paint. Progesterone is the foundation. If the foundation cracks, the paint will chip, no matter how beautiful it looks. Rebuilding the foundation doesn’t mean going back to your 20s. It means creating a new, stable structure that works for who you are now.
Does progesterone decline affect men too?
Yes. Men produce progesterone in their adrenal glands and testes. Levels drop steadily after age 35, contributing to fatigue, anxiety, poor sleep, and reduced muscle recovery. Low progesterone in men is often overlooked because it’s not linked to reproduction, but it plays a key role in stress balance and brain health.
Can I boost progesterone naturally without supplements?
Yes - but only if your body still has the capacity to make it. Focus on reducing stress, eating magnesium and zinc-rich foods, avoiding sugar, and getting good sleep. These support your adrenal and ovarian function. For many people over 45, natural methods help - but they may not be enough on their own.
Is bioidentical progesterone safe for long-term use?
When used correctly under medical supervision, bioidentical progesterone is considered safe for long-term use. Unlike synthetic progestins (like those in birth control pills), bioidentical progesterone matches your body’s own molecule. Studies show it doesn’t increase breast cancer risk the way synthetic versions can. Always get tested before starting and monitor levels every 3-6 months.
Why does my doctor say my progesterone is ‘normal’ when I feel awful?
Standard lab ranges are based on young, healthy women - not aging adults. A level of 1.0 ng/mL might be labeled “normal,” but if you’re 52 and not ovulating, your body needs more than that to function well. Functional medicine looks at what’s optimal for your symptoms, not just what’s statistically average.
Will progesterone help with hot flashes?
It can. Hot flashes are often caused by estrogen dominance - when estrogen is high relative to progesterone. Even if estrogen isn’t high, low progesterone leaves estrogen unchecked. Restoring progesterone helps balance the system, and many women report fewer and milder hot flashes within 4-8 weeks of using bioidentical progesterone cream.





Saket Sharma
November 19, 2025 AT 05:16Progesterone isn't just a 'female hormone'-it's the silent guardian of metabolic integrity. Drop below 1.5 ng/mL post-35, and you're running on fumes. Cortisol hijacks pregnenolone, the mother hormone, and your adrenals start producing anxiety instead of progesterone. This isn't aging-it's endocrine collapse. Fix it with transdermal bioidentical cream, not herbal tea.
Shravan Jain
November 20, 2025 AT 11:27Therapeutic progesterone? Hardly. The entire narrative is a pharmaceutical Trojan horse. Labs manipulate 'normal' ranges to sell tests. Your body isn't broken-it's adapting. You're being sold a solution to a problem they invented. Progesterone cream? It's just synthetic estrogen in disguise. Wake up.
Emily Entwistle
November 21, 2025 AT 18:09This hit me right in the feels 😭 I’m 41 and have been sleeping 3 hours a night for 2 years. My doctor said ‘it’s just stress.’ But this? THIS explains everything. I started bioidentical cream last month and I’m actually smiling again. Thank you for writing this. 🙏
Duncan Prowel
November 21, 2025 AT 19:12While the physiological mechanisms described are largely accurate, the diagnostic protocol recommended lacks standardization. Salivary progesterone assays exhibit significant inter-individual variability and are not universally validated against serum free hormone concentrations. A longitudinal, multi-point sampling regimen would be necessary to establish clinical relevance beyond anecdotal correlation.
malik recoba
November 22, 2025 AT 22:25i read this and thought ‘ohhh this is why i feel like a zombie after 3pm’... i’ve been eating spinach and pumpkin seeds for a week now and my brain feels less foggy. not magic, but better. thanks for sharing.
Sarbjit Singh
November 24, 2025 AT 07:06brothers and sisters-this is the truth we’ve been ignoring. progesterone isn’t optional. it’s the glue holding your mind and body together as you age. magnesium + sleep + stress management = your free hormone therapy. no pills needed. just consistency. you got this ❤️
Sameer Tawde
November 24, 2025 AT 22:35Stop waiting for doctors to save you. Your hormones don’t care about insurance codes. Test on day 21. Use cream. Eat nuts. Breathe. That’s it. No fluff. No hype. Just action.
Erica Lundy
November 26, 2025 AT 04:44There’s a metaphysical dimension here: progesterone decline mirrors our societal neglect of rest, cyclical rhythms, and embodied wisdom. We’ve pathologized aging instead of honoring its wisdom. The body doesn’t fail-it signals. Are we listening? Or are we still chasing youth as a moral imperative?
Kevin Jones
November 26, 2025 AT 05:33THIS. IS. THE. TRUTH. I’ve watched my dad turn into a snarling, sleep-deprived shell after 50. No one told him progesterone was crashing. Now he’s on cream. He’s laughing again. This isn’t medicine-it’s liberation.
Premanka Goswami
November 27, 2025 AT 02:34Big Pharma invented progesterone deficiency to sell creams. The real cause? Fluoride in the water. Glyphosate in your food. They don’t want you to know your adrenals can heal themselves if you just stop eating GMOs and drinking tap water. Progesterone cream? A trap. Go raw. Go alkaline. Go free.
Alexis Paredes Gallego
November 28, 2025 AT 17:27They’re lying. Progesterone doesn’t drop-it’s suppressed. The government, the FDA, the AMA-they all work for the estrogen pill companies. They don’t want you to know that a $20 cream can undo decades of hormonal manipulation. This is control. This is oppression. Wake up.
Brandon Lowi
November 30, 2025 AT 13:26Progesterone is the last bastion of biological sovereignty. While the woke left screams about gender fluidity, the one thing they can’t erase is the biochemical truth: your body remembers its roots. This isn’t ‘women’s health’-it’s human resilience. And if you’re not addressing it, you’re surrendering your vitality to the machine.
Joshua Casella
November 30, 2025 AT 22:30I’ve been telling people for years: if you’re tired, anxious, or gaining weight for no reason, check your progesterone. Not estrogen. Not testosterone. PROGESTERONE. I’m 47, on 10mg cream nightly, and I sleep 7 hours straight. My wife says I’m ‘less grumpy.’ That’s the real win.
Saket Sharma
December 2, 2025 AT 13:49@4192 - Exactly. And don’t fall for the ‘natural’ herb nonsense. Chasteberry won’t fix adrenal burnout. You need the real molecule. Topical is safer than oral. 5mg at night. Test before, test after. No more guessing.