Opioids and Sleep Apnea: Risks, Signs, and What You Need to Know
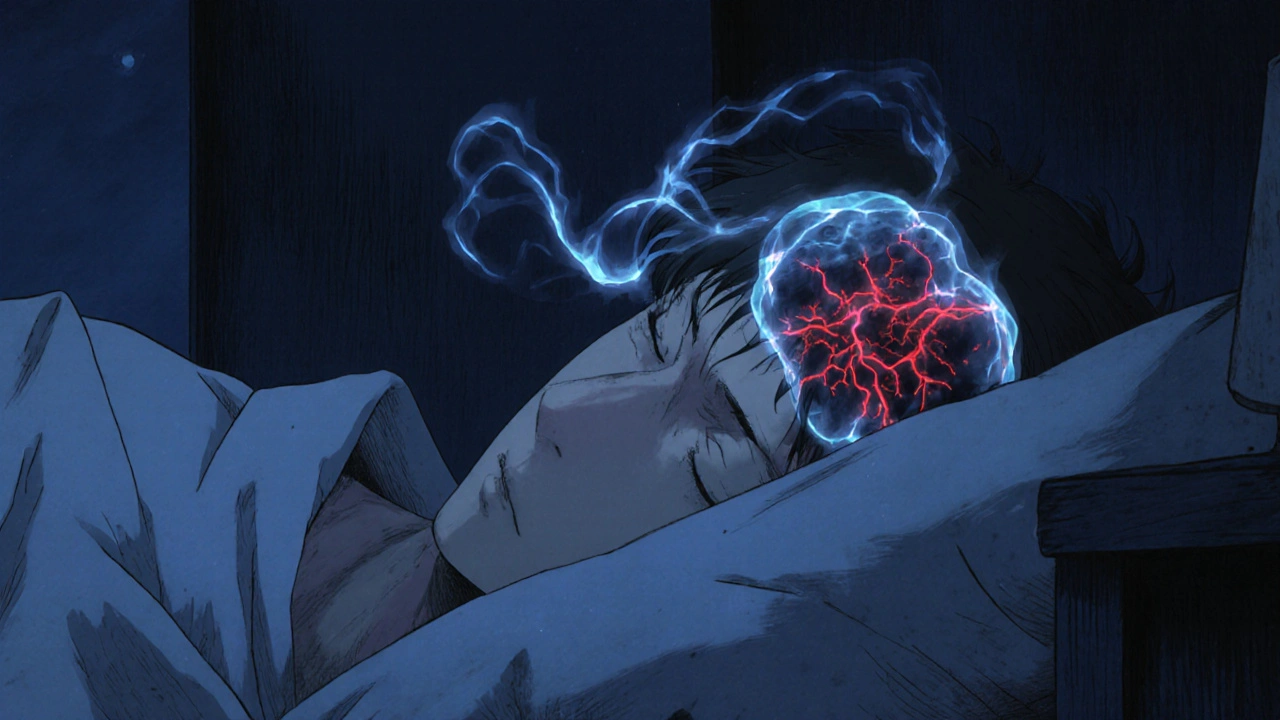
When you take opioids, a class of pain-relieving drugs that include oxycodone, hydrocodone, morphine, and fentanyl. Also known as narcotics, they work by slowing down your nervous system to reduce pain—but that same effect can turn deadly during sleep. Many people don’t realize that opioids don’t just dull pain; they also suppress the brain’s natural drive to breathe, especially at night. This isn’t just a side effect—it’s a well-documented risk that can lead to sleep apnea, a condition where breathing repeatedly stops and starts during sleep. Also known as obstructive sleep apnea, it’s not just about snoring. With opioids, it becomes a life-threatening issue.
People on long-term opioid therapy are up to three times more likely to develop sleep apnea than those who don’t take these drugs. The problem gets worse with higher doses or when opioids are mixed with alcohol, benzodiazepines, or sleep aids. Your body doesn’t wake up to take a breath like it should. Over time, your blood oxygen levels drop, your heart works harder, and your risk of heart attack, stroke, or sudden death climbs. Even if you don’t feel sleepy during the day, your sleep could still be dangerously disrupted. If you’ve been prescribed opioids and your partner says you stop breathing at night, or you wake up gasping, that’s not normal—it’s a red flag.
It’s not just about the drug itself—it’s about how your body responds. Some people are more sensitive to opioid-induced breathing changes because of age, weight, or existing lung or heart conditions. If you’re on opioids and also have obesity, chronic lung disease, or a history of snoring, your risk is even higher. Doctors often miss this link because they focus on pain control, not sleep quality. But if you’re taking opioids long-term, your breathing during sleep matters just as much as your pain level.
There’s no magic fix, but awareness helps. If you’re on opioids, ask your doctor about a sleep study. Simple changes—like avoiding alcohol, sleeping on your side, or using a CPAP machine—can make a big difference. In some cases, switching to a different pain medication or lowering the dose can restore normal breathing. The goal isn’t to stop pain relief—it’s to make sure it doesn’t cost you your sleep, or worse, your life.
Below, you’ll find real-world guides and clinical insights on how opioids affect breathing, what to watch for, and how to protect yourself if you’re using these medications. These aren’t theoretical discussions—they’re practical tools from people who’ve seen the consequences firsthand.