On-Target Side Effects: When Medications Cause Expected but Unwanted Reactions
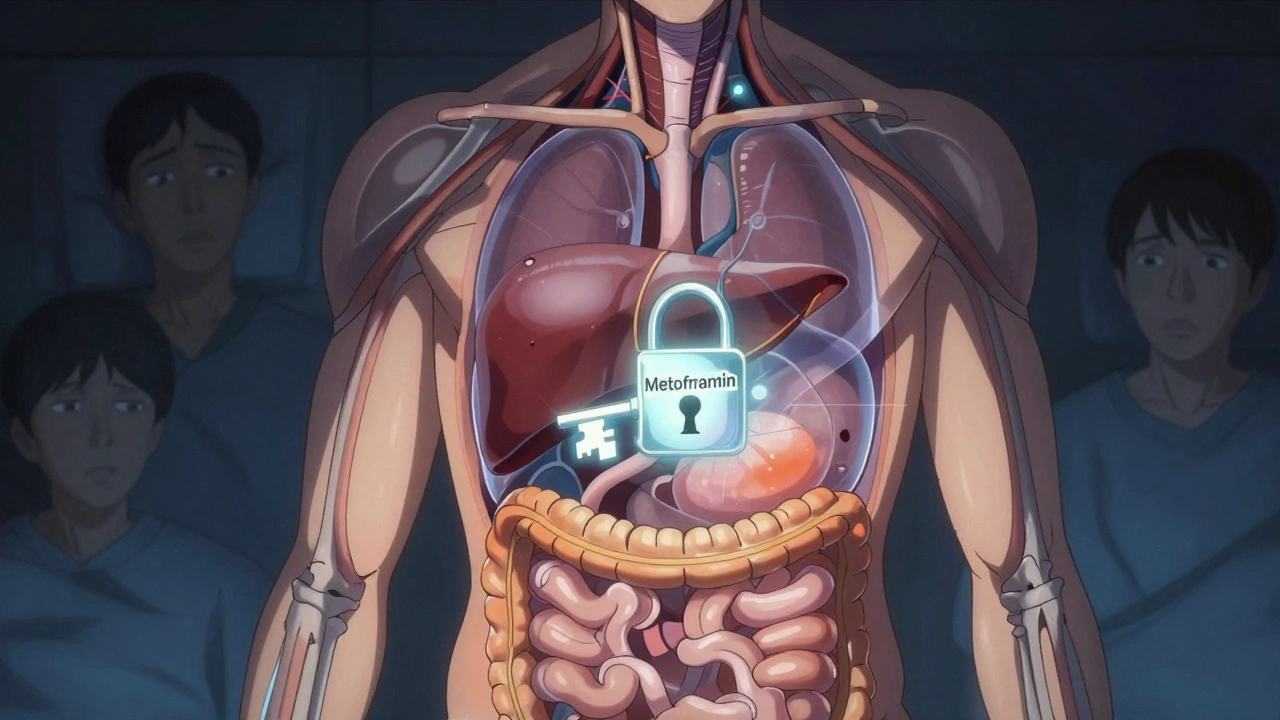
When a drug does exactly what it’s supposed to do—but still makes you feel awful—that’s an on-target side effect, an unintended consequence caused by a drug’s intended mechanism of action. Also known as pharmacological side effects, these aren’t mistakes or accidents. They’re the predictable result of how the drug interacts with your body’s own systems. Think of it like turning up the volume on a speaker too high: the sound works perfectly, but it’s painfully loud. This is different from random side effects, like a rash from a drug you’ve never had before. On-target effects happen because the drug hit its target… too well.
Take statins, cholesterol-lowering drugs that block an enzyme in the liver. Their job is to reduce LDL, which protects your heart. But that same enzyme is also involved in making muscle energy. So when statins block it, some people get muscle pain—not because the drug is faulty, but because it’s working too well in the wrong place. That’s an on-target side effect. The same thing happens with proton pump inhibitors, drugs that shut down stomach acid production to treat heartburn. Less acid helps your esophagus heal… but it also makes it harder for your body to absorb calcium and vitamin B12. Over time, that can weaken bones. Again, the drug is doing exactly what it’s designed to do—just with consequences you didn’t plan for.
These effects aren’t rare. In fact, they’re common enough that doctors expect them. That’s why you see warnings about steroid hyperglycemia, a spike in blood sugar from corticosteroids that suppress inflammation—even in people without diabetes. Or why opioids, painkillers that bind to nerve receptors to block pain signals almost always cause constipation. The pain relief? On-target. The slowed digestion? Also on-target. It’s the same mechanism. And that’s why simply switching drugs won’t always fix it—you might just trade one on-target effect for another.
Knowing the difference between on-target and off-target effects changes how you manage your meds. If your muscle pain from a statin is an on-target effect, stopping the drug might be the only real solution. But if your nausea from a blood pressure pill is off-target, there might be a better option in the same class. That’s why understanding your drug’s mechanism matters. It’s not just about avoiding bad reactions—it’s about predicting them, preparing for them, and working with your doctor to minimize their impact without losing the benefit.
What you’ll find in the posts below are real-world examples of these predictable-but-annoying reactions—and how to handle them. From melasma caused by hormone drugs to ileus from pain meds, these aren’t glitches. They’re side effects built into the design. And the good news? There are ways to live with them, reduce them, or sometimes even turn them to your advantage.