Off-Target Drug Effects: Unexpected Side Effects and How to Spot Them
When a drug works the way it’s supposed to, that’s called the on-target effect, the intended biological action of a medication. But sometimes, drugs hit the wrong targets—activating or blocking pathways they weren’t designed for. That’s an off-target drug effect, an unintended biological response caused by a drug interacting with non-target molecules. These aren’t rare glitches. They’re baked into how drugs work at a molecular level, and they’re behind many of the side effects patients report—like muscle pain from statins, skin darkening from antimalarials, or sudden blood sugar spikes from steroids.
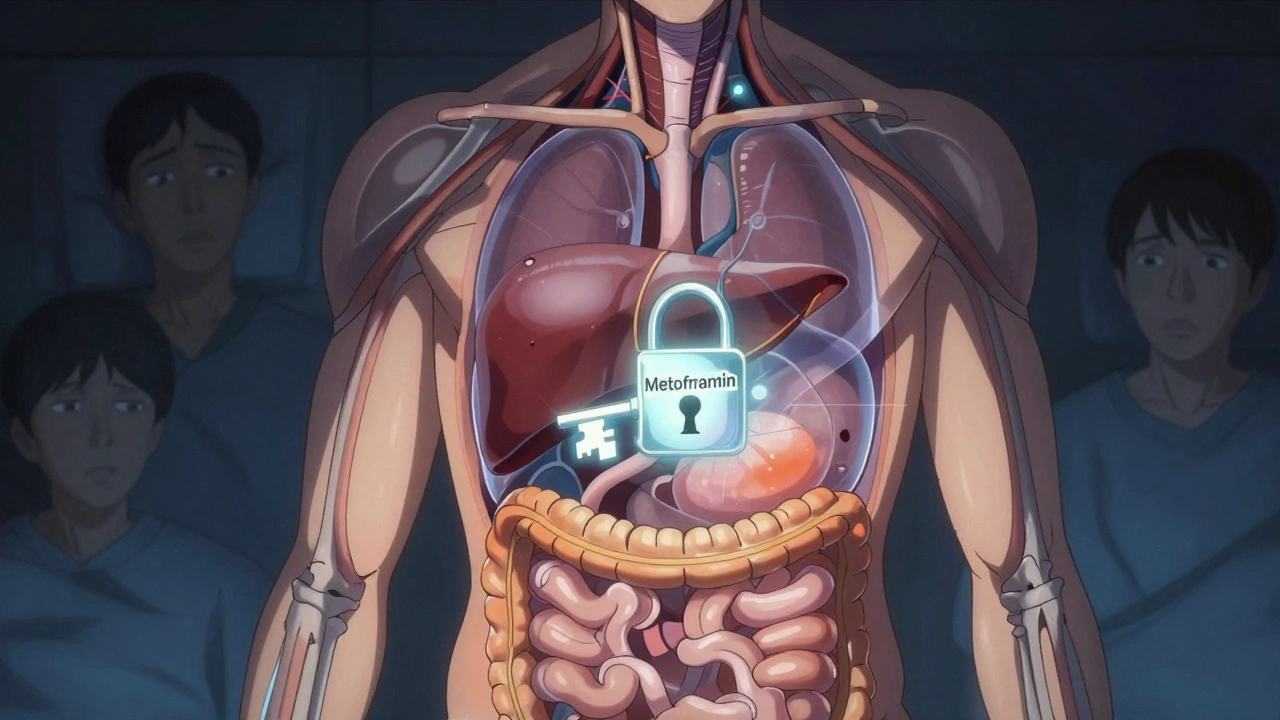
These effects happen because drugs don’t read instruction manuals. They bind to proteins, enzymes, or receptors based on shape and chemistry. If a drug molecule looks similar enough to another compound in your body, it might latch on accidentally. For example, clarithromycin, an antibiotic that inhibits CYP3A4 liver enzymes can accidentally boost levels of statins, leading to dangerous muscle damage. Or proton pump inhibitors, medications meant to reduce stomach acid, may interfere with calcium absorption over time, raising fracture risk. Even common substances like caffeine, a stimulant found in coffee and energy drinks can clash with blood thinners or thyroid meds, turning a harmless habit into a health risk.
What makes off-target effects tricky is that they often look like new diseases. A patient on a blood pressure pill starts feeling dizzy—was it the drug, or did they just get the flu? A woman on antidepressants gains weight—could it be metabolism, or an off-target effect on appetite hormones? The truth is, many side effects aren’t caused by the drug itself, but by your brain expecting them. That’s the nocebo effect, when fear of side effects triggers real physical symptoms. Studies show up to 90% of statin side effects vanish when patients take a sugar pill, proving that expectation plays a huge role.
But not all off-target effects are psychological. Some are predictable, and some are deadly. Fentanyl patches left in trash can kill a child. Missing a dose of seizure meds can trigger a crisis. Steroids can send blood sugar through the roof in diabetics. That’s why knowing your meds isn’t optional—it’s survival. You don’t need to be a scientist to spot trouble. Track what you take, note how you feel, and ask: "Could this be the drug?" Keep a log. Talk to your pharmacist. Use trusted resources like DailyMed or the FDA Orange Book. The posts below give you real-world examples: how statins cause muscle pain, why some generics trigger unexpected reactions, how caffeine messes with your pills, and what to do when a drug does more than it promises. You’ll find practical steps to protect yourself—not theory, not jargon, just what works.