Nausea from Kidney Disease: Causes, Management, and What You Can Do
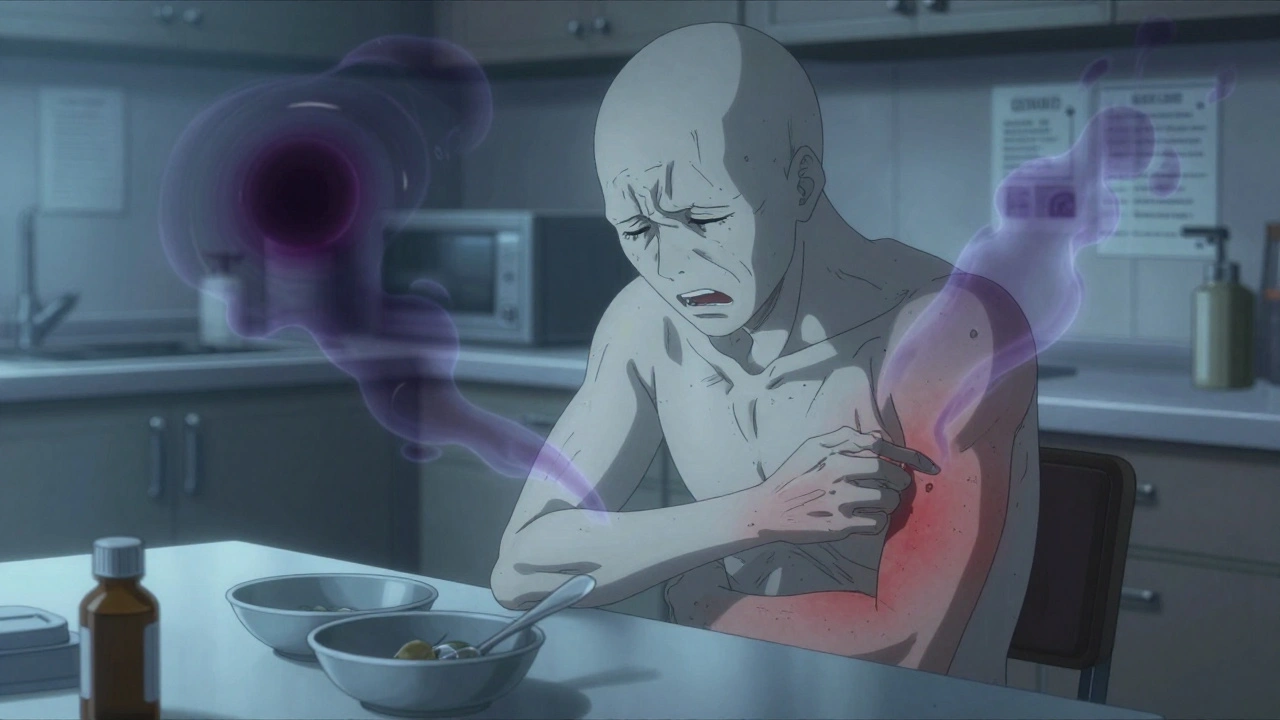
When your kidneys aren’t working right, nausea from kidney disease, a frequent and distressing symptom caused by waste buildup in the blood. Also known as uremic nausea, it’s not just an upset stomach—it’s your body signaling that toxins like urea and creatinine are piling up because your kidneys can’t filter them out. This isn’t something you can just push through with ginger tea or antacids. It’s a direct result of chronic kidney disease, a progressive condition where kidney function declines over time, often unnoticed until it’s advanced.
As kidney function drops below 30%, the body starts holding onto fluids and waste that should be flushed out. These toxins irritate the stomach lining and trigger the brain’s vomiting center. Many people mistake this for food poisoning or stress—until they realize it happens after every meal, even when they haven’t eaten anything unusual. It’s worse for those on dialysis, a treatment that removes waste from the blood when kidneys fail, especially if sessions are skipped or too short. Nausea after dialysis isn’t normal—it’s a red flag that the treatment isn’t doing its job well enough.
It’s not just about the kidneys. Other factors make nausea worse: high phosphate levels, low iron, acid buildup in the blood, and even some medications used to manage kidney disease. People often take pills for high blood pressure or anemia, not realizing some of them can irritate the stomach or interact with how the body handles waste. And because kidney disease often comes with other conditions—like diabetes or heart failure—the symptoms pile up, making it hard to tell what’s causing what.
What helps? It starts with getting your labs right. Regular checks for creatinine, urea, potassium, and phosphate tell your doctor if your treatment needs adjusting. Sometimes, a change in dialysis schedule or type can make a big difference. Diet matters too—cutting back on processed foods, salt, and high-phosphate additives reduces the toxin load. And while anti-nausea meds exist, many are risky for people with kidney issues. Always talk to your provider before taking anything new.
Some patients find relief with small, frequent meals instead of three large ones. Avoiding strong smells, staying hydrated without overloading fluids, and even mild walking after eating can help. It’s not about fixing the nausea—it’s about fixing the root cause: the failing kidneys. That’s why tracking your symptoms, sharing them honestly with your care team, and asking questions about your lab results is so important.
Below, you’ll find real, practical advice from people who’ve lived through this—how they managed nausea while on dialysis, what medications helped (and which didn’t), and how they learned to spot warning signs before things got worse. No fluff. Just what works.