Medication Understanding: How to Navigate Drug Interactions, Generics, and Safety
When you take a pill, you’re not just swallowing a chemical—you’re entering a complex system of biology, regulation, and corporate decisions. Medication understanding, the ability to know how, why, and when a drug affects your body and how it interacts with everything else you take. Also known as drug literacy, it’s not about memorizing pharmacology—it’s about asking the right questions so you don’t get hurt. Most people don’t realize that the same drug can behave totally differently depending on what else is in their system. A statin might cause muscle pain because of an antibiotic you’re taking, or caffeine might block your thyroid medication. This isn’t rare—it’s routine. And if you don’t know how to spot these risks, you’re playing Russian roulette with your health.
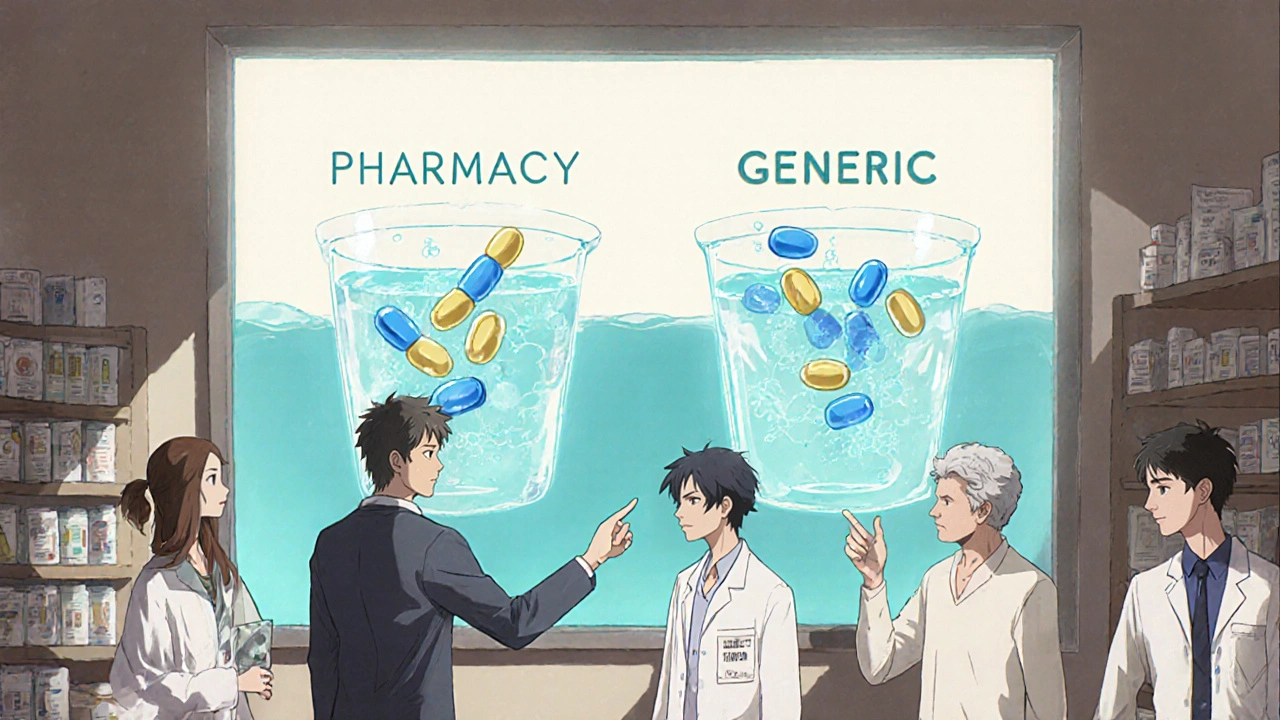
Generic drugs, identical versions of brand-name medications approved by the FDA after patents expire. Also known as off-patent drugs, they make up 90% of prescriptions in the U.S. but cost just 12% of total spending. Yet many still fear they’re inferior. They’re not. The same active ingredient. Same dosing. Same results. But big pharma uses tricks like evergreening—making tiny changes to old drugs to lock out generics—and legal barriers like the TRIPS agreement to keep prices high. Understanding this helps you push back when your pharmacy tries to upsell you a more expensive brand. You’re not just saving money—you’re fighting a system designed to keep you dependent.
Drug interactions, when one medication changes how another works in your body, often dangerously. Also known as medication conflicts, they’re the #1 cause of preventable hospital visits in older adults. Think clarithromycin raising statin levels until your muscles start breaking down. Or St. John’s wort making birth control useless. These aren’t edge cases—they’re everyday risks. And the nocebo effect makes it worse: if you believe a drug causes side effects, your brain can make you feel them—even if it’s just a sugar pill. That’s why knowing the science behind your meds isn’t optional. It’s survival.
Medication safety isn’t about following a doctor’s order blindly. It’s about knowing what’s in your medicine cabinet, how it affects your body over time, and what to do when things go wrong. Miss a dose of blood thinner? Don’t double up. Taking PPIs for years? Watch your bones. Using steroids and have diabetes? Adjust your insulin before the spike hits. These aren’t abstract concepts—they’re life-or-death decisions you’ll face, probably more than once.
Below, you’ll find real, practical guides that cut through the noise. No marketing. No jargon. Just what you need to know to take control: how to verify if your generic is real, how to avoid deadly interactions, why your statin side effects might be in your head, and how to survive when your meds don’t behave as expected. This isn’t theory. It’s what works.