Insulin Adjustment: How to Safely Modify Doses for Better Blood Sugar Control
When you need to insulin adjustment, the process of changing your insulin dose to match your body’s needs. It’s not just about numbers on a meter—it’s about matching food, activity, stress, and even sleep to keep your blood sugar in a safe range. Many people think insulin is set and forget, but that’s not true. Your body changes. Your life changes. Your insulin dose should too.
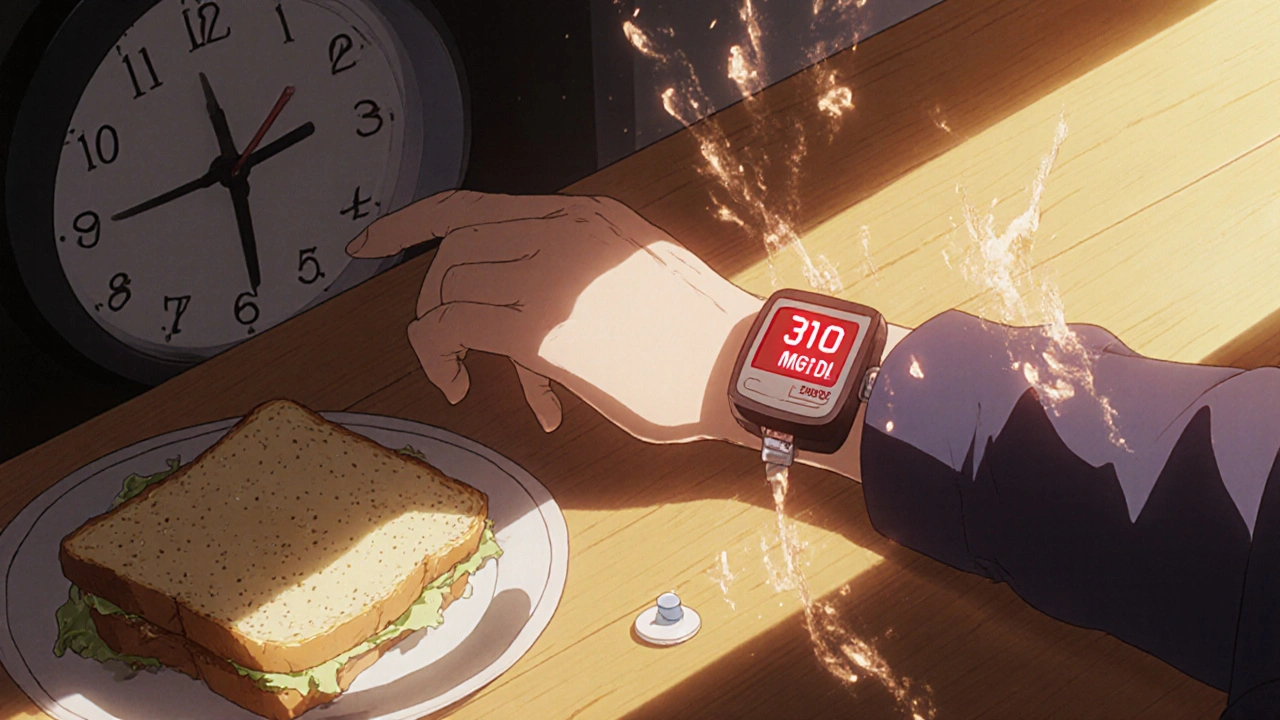
Blood sugar control, the goal of keeping glucose levels stable throughout the day depends heavily on how well you adjust insulin. Too little, and your sugar stays high—risking nerve damage, kidney issues, and fatigue. Too much, and you crash into low blood sugar, which can mean shaking, confusion, or even passing out. Insulin dosing, the specific amount of insulin you take at each meal or time of day isn’t one-size-fits-all. It shifts with weight, activity level, illness, hormones, and even the time of year. People on multiple daily injections or insulin pumps adjust constantly. Even small changes—like adding 1 unit before dinner or skipping a correction dose after a light meal—can make a big difference.
Diabetes management, the daily routine of monitoring, medicating, eating, and moving to stay healthy with diabetes isn’t just about taking insulin. It’s about understanding why you’re adjusting it. Did your sugar spike after a big pasta dinner? Maybe you need more insulin for carbs. Did it drop after a long walk? Maybe you need less before exercise. Some people adjust based on trends over days, not just one reading. Others use apps or logs to spot patterns. The key is consistency—not perfection.
And don’t forget insulin types, the different kinds of insulin that act at different speeds and durations. Rapid-acting insulin works fast for meals. Long-acting insulin keeps your baseline steady. Mixing them wrong, or changing one without adjusting the other, can cause trouble. If you’re switching from one type to another—say, from Lantus to Basaglar—you need to know how the timing and strength differ. Even brand changes can require small tweaks.
You won’t find one magic formula for insulin adjustment. But you can learn your own patterns. Track your meals, activity, stress, and blood sugar for a week. Look for what makes your numbers climb or drop. Talk to your doctor or diabetes educator about how to safely make changes. Never double up a dose because your sugar is high. Never skip a dose because you’re scared of lows. Small, smart adjustments over time beat big, risky swings.
Below, you’ll find real stories and practical guides from people who’ve been there—how to handle missed doses, what to do when sick, how to adjust for exercise, and how to avoid common mistakes that lead to hospital visits. These aren’t theory pieces. They’re tools you can use tomorrow.