Dialysis Initiation: What You Need to Know Before Starting Treatment
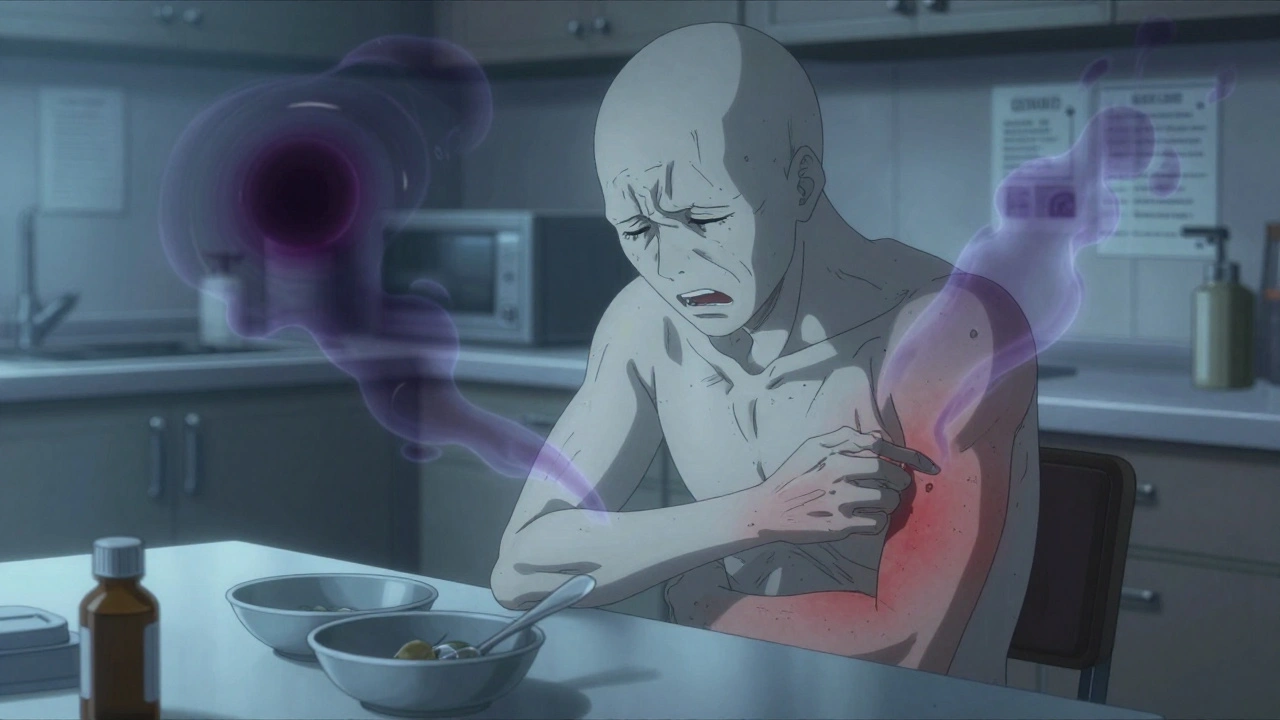
When your kidneys can no longer filter waste and extra fluid from your blood, dialysis initiation, the process of beginning life-sustaining treatment for kidney failure. Also known as renal replacement therapy, it becomes necessary when kidney function drops below 10-15%. This isn’t a choice made lightly—it’s often the result of years of uncontrolled diabetes, high blood pressure, or other chronic conditions that slowly damage the kidneys. Many people start dialysis after months or even years of warning signs: swelling in the legs, fatigue, trouble breathing, or nausea that won’t go away. The decision usually comes after blood tests show creatinine and eGFR levels are dangerously low.
There are two main types of hemodialysis, a treatment that uses a machine to filter blood outside the body and peritoneal dialysis, a method that uses the lining of your abdomen as a natural filter. Hemodialysis typically happens three times a week at a clinic, where needles are inserted into a surgically created access point in your arm. Peritoneal dialysis can be done at home, often overnight, using a fluid that’s swapped in and out of your belly through a catheter. Neither is perfect—both come with risks like infection, low blood pressure, or access site complications—but each gives you control over your schedule and lifestyle in different ways.
What most people don’t realize is that dialysis initiation isn’t just about the machine or the procedure—it’s about preparing your body, your mind, and your support system. Nutrition changes are critical: you’ll need to limit potassium, phosphorus, and sodium. Fluid intake becomes a daily calculation. Medications shift, too—some drugs are removed during dialysis, others become more dangerous if not adjusted. And while many fear dialysis will end their independence, thousands live full lives on it—working, traveling, even raising families. The key is starting early enough to avoid emergency dialysis, which carries much higher risks.
You’ll work with a nephrologist, a dialysis nurse, a dietitian, and sometimes a social worker to build your plan. They’ll help you choose the right type of dialysis, train you or your caregiver, and set up your access—whether it’s a fistula, graft, or catheter. Timing matters: starting before you’re critically ill gives you better outcomes and more options. Waiting until you’re in crisis can mean hospitalization, longer recovery, and fewer choices.
Below, you’ll find real-world guides that cover what to expect before, during, and after dialysis initiation. From managing fluid balance to understanding why some medications need to be stopped, these posts give you the facts without the jargon. Whether you’re a patient, a caregiver, or just trying to understand what this treatment really means, you’ll find practical, no-fluff advice that helps you take control.