Diabetes and Steroids: How Steroids Affect Blood Sugar and What to Do
When you take steroids, powerful anti-inflammatory drugs like prednisone or methylprednisolone used for autoimmune conditions, asthma, or severe allergies. Also known as corticosteroids, they can seriously disrupt how your body handles sugar—especially if you have diabetes, a chronic condition where the body can’t properly regulate blood glucose. Many people don’t realize steroids can trigger high blood sugar, even if they’ve never had diabetes before. This isn’t just a side effect—it’s a common clinical issue that can lead to hospital visits if ignored.
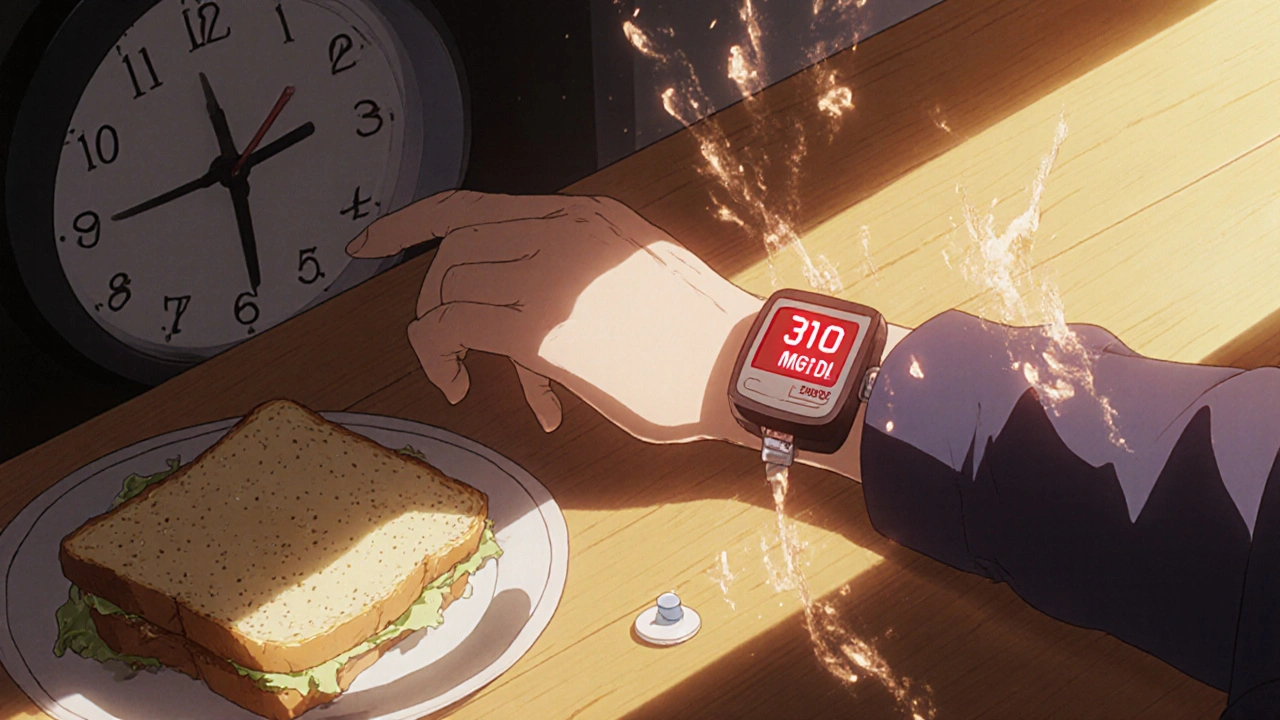
Steroids make your liver pump out more glucose and block insulin from doing its job. That means sugar builds up in your blood, fast. People with type 2 diabetes often see their numbers jump by 50% or more on steroids. Even those with prediabetes can slip into full-blown steroid-induced diabetes, a temporary but dangerous form of high blood sugar caused by steroid use. It’s not your fault. It’s biology. And it’s why doctors need to monitor blood sugar closely when prescribing steroids, especially for more than a few days. If you’re on insulin or oral diabetes meds, your dose may need adjusting—sometimes dramatically—while you’re on steroids.
What you can do? Track your blood sugar more often. Know your numbers. Talk to your doctor before starting steroids—ask if there’s a lower dose, shorter course, or alternative treatment. Don’t skip your diabetes meds because you feel fine. Steroids don’t care how you feel—they’re still messing with your metabolism. And if you’re newly diagnosed with high blood sugar after starting steroids, don’t panic. It often reverses once you stop, but only if you manage it right. This collection of posts gives you real-world strategies: how to spot trouble early, what meds to watch for, how to protect your kidneys and heart while on steroids, and what to do if your sugar spikes at night or after meals. You’ll find practical advice from people who’ve been there, backed by data—not guesses.