CPAP Therapy: What It Is, How It Works, and What You Need to Know
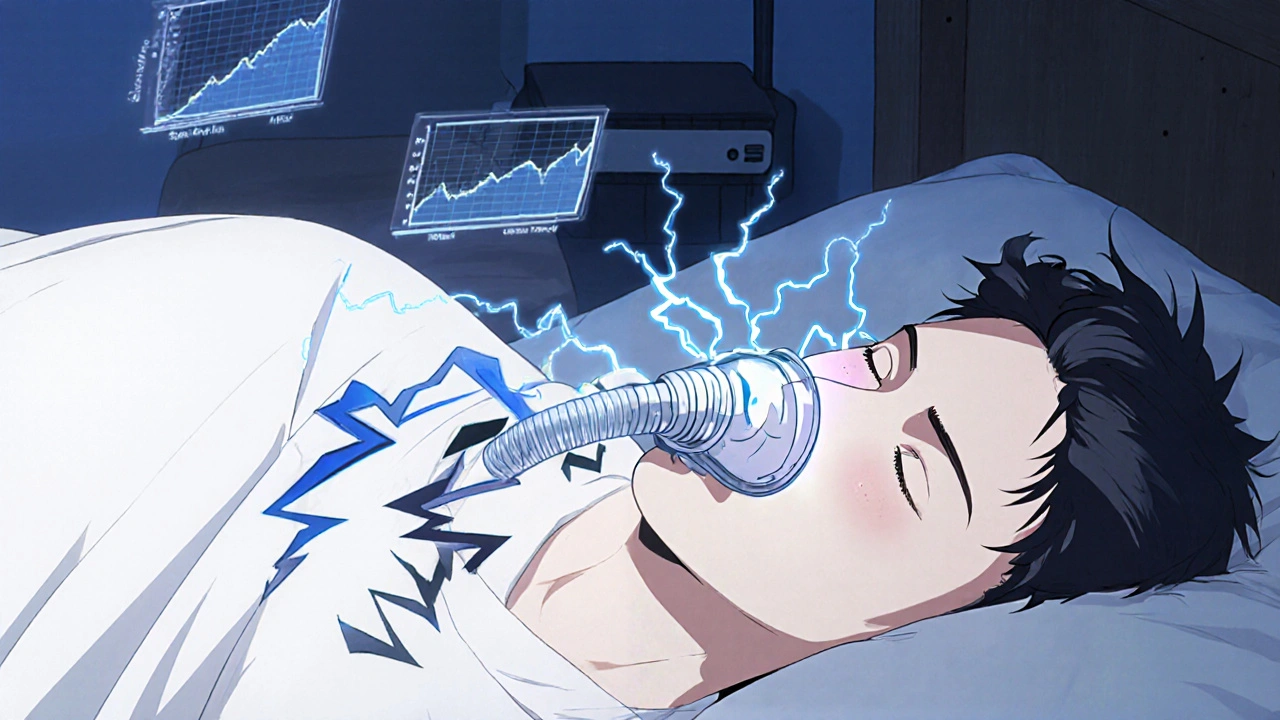
When you struggle to breathe while sleeping, CPAP therapy, a non-invasive treatment that uses steady air pressure to keep airways open during sleep. Also known as continuous positive airway pressure therapy, it's the go-to solution for millions with sleep apnea — a condition where breathing stops and starts repeatedly through the night. This isn’t just about snoring. Untreated sleep apnea strains your heart, scrambles your brain function, and raises your risk of stroke, high blood pressure, and even sudden death while sleeping.
One major reason CPAP therapy works is because it directly fights respiratory depression, a dangerous drop in breathing rate caused by drugs, obesity, or neurological issues. For example, opioids — like those used for chronic pain — can suppress the brain’s breathing signals, leading to central sleep apnea, a type where the brain fails to send proper signals to breathe. CPAP doesn’t fix the root cause of opioid-induced apnea, but it can keep your airway open and oxygen levels stable while you sleep, giving your body a fighting chance.
It’s not just about machines and masks. CPAP therapy ties into bigger health patterns. If you’re dealing with obesity, heart failure, or even chronic nasal congestion, your chances of needing CPAP go up. And if you’ve ever been told your breathing sounds irregular at night — or your partner says you stop breathing for seconds at a time — that’s not normal. It’s a red flag. The good news? CPAP therapy is proven, widely studied, and covered by most insurance plans. It’s not magic, but it’s one of the few treatments that actually changes outcomes.
What you’ll find below are real, practical posts that dig into the connections between CPAP therapy and other health issues. You’ll see how opioids make sleep apnea worse, how to spot signs you’re not getting enough air at night, and why some people give up on CPAP — and how to stick with it. There’s no fluff. Just clear facts, real risks, and what actually works when your breathing fails you while you sleep.