Corticosteroid Blood Sugar: How Steroids Raise Glucose and What to Do
When you take corticosteroids, a class of anti-inflammatory drugs used for conditions like asthma, arthritis, and autoimmune diseases. Also known as steroids, they work by suppressing the immune system—but they also interfere with how your body handles sugar. This is why many people see their blood sugar rise unexpectedly, even if they’ve never had diabetes before.
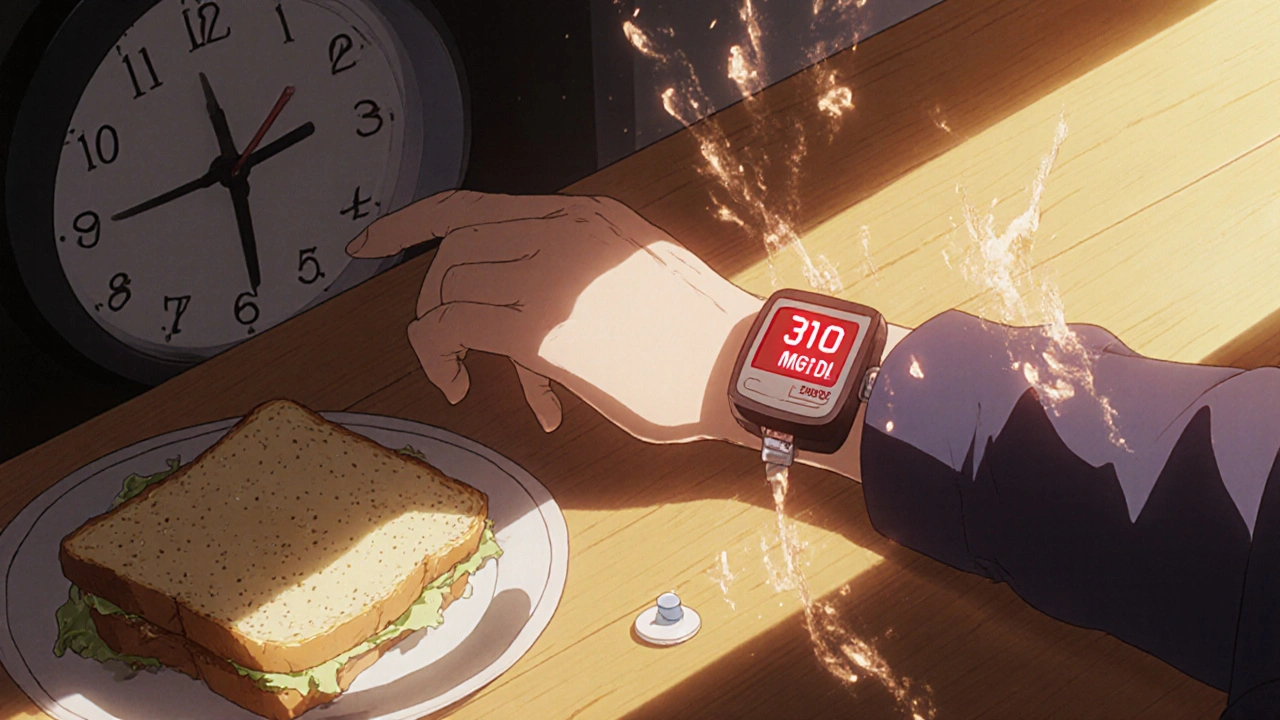
It’s not just a side effect—it’s a predictable one. Corticosteroids tell your liver to pump out more glucose, while also making your muscles and fat cells less responsive to insulin. The result? High blood sugar. Studies show that up to 30% of people on long-term steroid therapy develop steroid-induced hyperglycemia. For those already managing diabetes, it can turn a stable condition into a medical emergency. This isn’t rare. It’s common enough that doctors check blood sugar before and during steroid treatment.
People who are overweight, older, or have a family history of diabetes are at higher risk. But even healthy people can see fasting glucose jump by 50% or more after starting prednisone or dexamethasone. The effect isn’t always immediate—it often builds over days. And it doesn’t go away the moment you stop the drug. Some people need weeks to return to normal sugar control. That’s why monitoring matters. If you’re on steroids, check your blood sugar regularly. Know your numbers. Talk to your doctor about adjusting diet, activity, or even adding a short-term glucose-lowering medication if needed.
It’s not just about pills. What you eat matters more than ever. Cutting back on refined carbs and sugary drinks helps. Eating protein and fiber with every meal slows sugar absorption. Walking after meals lowers spikes. These aren’t suggestions—they’re survival tactics when your body’s insulin response is being blocked by medication.
And don’t assume it’s just a diabetes issue. High blood sugar from steroids can cause fatigue, blurry vision, frequent urination, and slow healing. These symptoms are often blamed on stress or aging—but they might be your body screaming about the steroid. If you’re on long-term treatment, ask your doctor about a glucose tolerance test. It’s simple, non-invasive, and could catch a problem before it becomes serious.
Below, you’ll find real, practical advice from people who’ve dealt with this exact problem. From how to adjust meals while on prednisone, to which medications can help without adding more risk, to what to watch for when you’re weaning off steroids. This isn’t theory. It’s what works when your blood sugar won’t cooperate—and you still need the medicine.